Unit 9: Renal System
advertisement

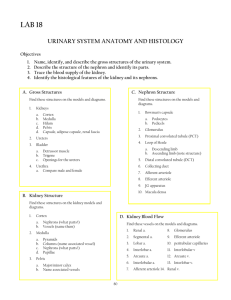
1 Objectives for the Renal System 1. State the function of the renal system 2. List the organs of the renal system 3. Describe the blood supply of the kidney 4. Explain the function of the nephron 5. Describe the structure & function of the glomerulus 6. Name the 4 tubular components of the nephron 7. Discuss the hormonal control of the kidney 8. Describe how the sympathetic nervous system controls the kidney & filtration 9. Explain the micturition reflex 10. Name the 2 sections involved in fluid & electrolyte movement 11. Discuss the function of Sodium ion 12. Discuss the function of the cation Potassium 13. Discuss the major cardiovascular manifestations in hyperkalemia & hypokalemia 14. Describe the function of calcium, phosphate, & magnesium 15. Discuss the differences & manifestations of metabolic alkalosis, metabolic acidosis respiratory alkalosis & respiratory acidosis 16. Discuss the types of renal alteration such as kidney stones, UTI, Acute renal failure & trauma. 2 Unit 9: Renal System It is no exaggeration to say that the composition of the blood is determined not so much by what the mouth takes in as by what the kidneys keep. Homer Smith, From Fish to Philosopher I. Renal System A. Functions 1. Regulation of blood volume & blood pressure – renin, volume, erythropoietin 2. Regulation of the concentrations of plasma ions - Na, K, Cl, Ca (calcitriol) 3. Blood pH (acid/base balance) – loss of hydrogen ion and bicarbonate 4. Conservation of nutrients – glucose & amino acid conserved but eliminating organic wastes B. Organs of the Renal System 1. Kidney = produce urine = liquid with water, ions, small soluble compounds (leaves kidney to ureters, bladder to urethra to exit) a. Location 1) Bilateral – last thoracic to 3 lumbar 2) Retroperitoneal (not as big threat to peritoneal cavity) 3) Right lower than Left (liver) 4) Retroperitoneal – behind peritoneum b. Protection 1) Adipose tissue 2) Rib structure 3) Renal capsule – dense, fibrous 4) Position maintained by overlying peritoneum, adjacent organs, supportive connective tissue (suspensory collagen fibers) c. Shape – kidney bean 1) Hilus indented spot – nerves, blood vessels, ureters 2) Multilobular (18 lobes) 3) Nephron – functional unit 4) Divisions a) Cortex – reddish brown with glomeruli & convoluted tubules & blood vessels b) Medulla – light color cone shaped masses (renal pyramids) = 6-18 (1) Papillae – tips of renal pyramids (2) Renal columns – between pyramids; cortical tissue (3) Minor calyx – cup shaped drain from papilla (4) Major calyces – merging of 4-5 minor calyces 3 5) Renal pelvis – funnel shape that drains kidney – connects to ureter (1) Combination of minor & major calyces 6) Capsule – fibrous outside cover surrounded by fatty connective tissue d. Blood Supply 1) Renal artery – bilateral from abdominal aorta a) Divides into 5 segments (1) Lobular arteries (2) Interlobular arteries towards renal pyramids (3) Arcuate arteries – between cortex & medulla (4) Intralobular arteries- cortex (5) Afferent arterioles – into glomerulus (6) Efferent arterioles – away from glomerulus 2) Venous a) Interlobular vein to arcuate vein, to renal vein to inferior vena cava 3) Nephron capillary system (surround where solute movement is) a) Glomerulus (1) High pressure, filter (2) Between afferent & efferent arterioles b) Peritubular capillary network (1) Low pressure, reabsorption system from efferent arteriole c) Medullary nephron (1) Peritubular – similar to one in cortex (a) Rejoin to form venous outflow (2) Vasa recta – loop of Henle for exchange 4) Flow – all through cortex only 10% via medulla 1% in papillae a) Decreases in flow decrease filtration for urine concentration 5) Hormones affecting kidneys a) Renin-Angiotensin b) ADH c) Aldosterone d) Atrial Natriuretic Peptide e. Parts of the Kidney 1) Nephron – functioning unit (1,000,000/kidney) begins at renal corpuscle (Bowman’s capsule) and ends in renal tubule a) Function – filtrate = protein free solution (1) Reabsorbs all useful organic molecules 4 (2) Reabsorbs 90% water (3) Secretes into fluid any waste products missed in filtration b) Glomerulus – blood filtered – capillary knot (1) Bowman’s capsule – encasement of Capillaries – outer wall renal corpuscle (a) Blood flows into afferent arteriole & out efferent (2) Bowman’s space – filtration space (a) Filtrate (3) Renal corpuscle – encapsulates glomerulus & Bowman’s (a) Capsular epithelium – outer wall (b) Capsular space – space between outer wall & glomerulus receives the filtrate, empties to tubules (4) Glomerular capillary membrane (fenestration) (a) Endothelial layer – covers Bowman’s Capsule – lines & contact with blood [1] Separate podocytes & epithelial layer- cover capillaries [2] Fenestrations on capillaries – pores (b) Basement membrane – acellular meshwork of collagen, glycoprotein, monosaccharidedetermines permeability [1] Size too small for RBC & plasma passage (c) Mesangium [1] Macrophagocytic [2] Contractile To enter filtrate solution the solutes must be small enough to pass through pores of endothelial cells, fibers basement membrane, & fenestrated slits in podocytes!!!!!! 2) Tubular Component – water, electrolytes & other substances reabsorbed or excreted a) 4 segments (1) Proximal convoluted tubule - reabsorb organic nutrients, reclaim 60-70% volume & reclaim glucose, AA, organic nutrients, Na, K, Ca, Mg, bicarb, PO4, 5 sulfate, work ion pump, move urea & uric acid in tubules (2) Loop of Henle (thin) (a) Descending limb towards renal pelvis permeable to water = osmosis not permeable to solutes (b) Ascending limb – towards the cortex impermeable to water & solutes highly concentrated solution (c) Active transport Na & Cl reabsorbed in ascending (d) Half the volume enters reabsorbed in descending loop (e) Left are the wastes (3) Distal convoluted tubule(a) Passes between afferent & efferent arterioles (b) Active secretion ions, acids, drugs, toxins (c) Active transport Na & exchange for K (d) 80% H2O & 85% solutes reabsorbed by this period (e) Aldosterone influences ion pumps higher amounts = more Na absorbed & more K lost (f) ADH effects water absorb (g) Macula Densa cells of epithelium associated with smooth muscle fibers – Juxtaglomerular in afferent arteriole (h) Juxtaglomerular apparatus - renin (4) Collecting tubule (late & cortical) (a) Merge to papillary duct (b) Transport tubular fluid to minor calyx (c) Final adjustments – reabsorb water, Na, K, Hydrogen, bicarb ions (d) ADH affects 3) Juxtaglomerular apparatus – endocrine structure a) Secretes rennin & erythropoietin b) Made of macula densa cells & Juxtaglomerular cells c) Found in the afferent arteriole wall 4) Nephron classification (a) Cortical nephron (b) Juxtaglomerular capillaries 6 To accomplish waste secretion: Kidney must Filter, Reabsorb, Secrete f. Metabolic wastes 1) Urea – breakdown of amino acids 2) Creatinine – breakdown skeletal muscles 3) Uric acid – breakdown & recycle of RNA g. Glomerulus filtration 1) Filtration pressure – net force promoting filtration a) Pressure higher in efferent arteriole (diameter) leads to blood back-up & increased BP b) Altered by BP c) This outward pressure must exceed other pressures d) Low pressure (10mm Hg) – if Glomerular blood pressure falls = fall in filtration pressure 2) Glomerular filtration – filtrate production at glomerulus a) Glomerular filtration rate (GFR) – amount filtrate produced in kidneys/minute (125ml/min) (20% volume sent to kidney by artery leaves and goes into capsular space) (1) 180 liters/day but 99% reabsorbed (2) No filtration wastes, pH, & volume at risk (3) Depends on adequate BP & volume (4) Hormonal helps (5) Renin-angiotensin system changes rate h. Reabsorption & Secretions 1) Filtration – renal corpuscle across glomerulus 2) Proximal Convoluted Tubule – reabsorb nutrients 3) Loop of Henle – regulates amounts water, Na ions, K ions lost & interacts with collection system 4) Distal Convoluted Tubule – active secretion 2. Ureters a. Muscular tubes b. Retroperitoneal c. Peristaltic contractions & sweep urine out renal pelvis to bladder 3. Urinary bladder a. Muscular distensible sac b. Storage & collection (1 liter) 1) Female anterior to uterus 2) Male between rectum & pubic symphysis c. Ureteral openings – d. Neck – muscular sphincter e Internal urethral sphincter – involuntary discharge of urine f. Trigone g. Internal urethral 7 4. Urethra a. Female = short b. Male = long, prostate gland c. External urethral sphincter – skeletal muscle fibers, voluntary control 5. Property of Urine (1200 ml/day) C. Control of the Kidney 1. Automatic adjustments or Local regulations a. Diameter changes in vascular system 2. Sympathetic Activation (direct & indirect) a. Lowering the glomerular filtration rate by changing the blood flow 1) Triggered by drop in blood pressure b. Changes in blood circulation (constriction of afferent arterioles) 1) Weather or excessive exercise can cause decrease flow c. Long term = rennin secretion d. Dopamine 3. Hormonal a. Renin-Angiotensin System- fall in volume leads to lower BP leads to rennin release from juxtaglomerular. 1) Renin leads to the conversion of angiotensinogen to angiotensin I (short & long term regulation) 2) Angiotensin-converting enzyme converts angiotensin I to angiotensin II in lungs a) Vasoconstriction = increase BP renals b) Nephron site contraction afferent arteriole = increase in GFR c) CNS releases ADH – Na & water reabsorption c) Adrenal secretion of aldosterone & epinephrine = increase in systemic BP & Na reabsorption d) Renin stimulated by Angiotensin II to constrict efferent causes stabilization of GFR 3) Angiotensin II stimulates aldosterone b. Erythropoietin (89-95% kidney) 1) Causes RBC differentiation 2) Stimulated by decrease in O2, anemia, high altitudes, cardiac pulmonary diseases 3) Kidney disease = anemia c. Vitamin D 1) Activation occurs in kidney 2) Calcium absorption in GI & deposition in bone 3) Types 8 a) Natural – ultraviolet light b) Synthetic Vitamin D 4) Renal disease hinders or prevents activation d. Antidiuretic hormone (ADH) 1) Increases water permeability of DCT & Collecting ducts 2) Reabsorption of water from fluid 3) Thirst sensation for increase water intake 4) Stimulation by angiotensin II & hypothalamic 5) Special receptors in hypothalamus e. Aldosterone 1) Na absorption & K release 2) Stimulated by angiotensin II & hyperkalemia f. Atrial Natriuretic Peptide (ANP) 1) Decrease in Na reabsorption 2) Dilation glomerular capillaries -= Increase GFR & H2O loss 3) Inactivation of rennin-angiotensin system by inhibitin rennin Aldosterone, ADH 4) Results = increased volume urine produced & increased Na losses D. Micturition Reflex 1. Micturition reflex a. Stretch receptors in wall of bladder 1) Afferent sensory fibers in pelvic nerves impulses to sacral Spinal cord 2) Impulses sent to cerebral cortex = awareness b. Urge occurs at 200ml 1) Motor neurons stimulate smooth muscles - parasympathetic 2) Fluid pressures raised – motor neuron detrusor muscle bladder wall 3) Internal & external sphincters relax a) External = voluntary; must relax first before internal b) Contraction elevates pressure 4) 500ml causes internal reflex to open 5) 10ml left after micturition & cycle begins again – 1 hour a) Stretch receptors stimulated II. Fluid, Electrolyte, Acid-Base Balance A.Homeostasis – affects the whole body 1. Water intake = water output 2. Electrolyte gain = loss 3. Acid – base = hydrogen ion loss = gain B. Fluid & Electrolyte 1. Compartments (exchanges occur across a membrane) a. Intracellular = inside the cell (proteins & organic compounds) – 60% 9 b. Extrcellular = outside cell (tissue, plasma, lymph, pleural, pericardial peritoneal fluids, CSF, Synovial fluid, Serous fluid, Aqueous humor, endolymph) – measured in blood - 40% 1) Transport for gases, nutrients, waste, and reservoir for reserve 2) Subdivisions a) Tissue/interstitial fluid b) Plasma c) Minor c. Cell membrane – separate the two compartments 2. Fluid balance (intake= output) a. Water moves between blood & cerebrospinal b. 2500 ml lost /day in urine, feces, perspiration c. Fluid shift – between ECF & ICF d. Moves from higher concentration to lower concentration e. ICF >volume than ECF = ICF reserve f. Fluid movement controlled by 1) Filtration pressure – pushes water out capillary – thru capillary pores 2) Capillary colloidal osmotic pressure – pulls water into capillary generated by plasma proteins too big to move in 3) Interstitial fluid pressure – opposes water movement out cap. 4) Tissue colloidal osmotic pressure – pulls water out capillary into interstitial spaces g. Excess 1) Edema 2) Third-spacing – trapping of ECF in transcellular space 3. Electrolytes a. Terminology 1) Ion – particles dissociate a) Cations = positive b) Anions = negative 2) Diffusion – movement of charged particles higher to lower concentration 3) Osmosis – movement of water over semipermeable membrane down a gradient (water towards more solutes) a) Osmotic pressure – pressure created by water movement 4) Tonicity – tension or effect osmotic pressure causes cell to swell or shrink b. Sodium (most abundant cation in body) 1) Movement is across cell membrane (sodium & water together) 2) Most sodium in ECF = 135-145 mEq/L 3) Movement by Na/K ATP pump – against gradient 4) Regulates fluid volume in both extracellular & vascular 5) Major player in acid/base balance (Na bicarb) & contributes to 10 Nervous system excitability 6) Dietary uptake and kidneys involved in uptake & regulation 7) Sodium regulation a) Sympathetic nervous system b) Renin-Angiotensin-Aldosterone System 8) Alterations a) Hyponatremia less than 135 mEq/L (1) Causes: diuretics, excessive sweating, excessive water intake, adrenal insufficiency, GI irrigations (2) Manifestations (a) Muscle cramps, weakness, fatigue Nausea/vomiting, lethargy Headache (brain swelling) (b) Deep tendon reflex depression, Seizures b) Hyponatremia above 145 mEq/L (1) Causes: decrease volume intake, excessive fluid loss, diarrhea, cell dehydration, excessive Na intake (Na bicarb or hypertonic Na IV intake) (2) Manifestations: decreased urine output & osmolality, increase temp., increase HR, decreased BP, agitation, restlessness, Seizures c. Water 1) Varies with age, weight, gender (infants more; elderly & obese less) 2) Gains via oral intake; losses via kidney a) Obligatory urine output (300-500 ml/day) b) Insensible water losses (skin, respiratory) 3) Regulation a) Thirst b) ADH 4) Alteration in output a) Diabetes insipidus (DI) b) Syndrome of Inappropriate Antidiuretic Hormone (SI) d. Potassium (2nd most abundant cation & major player ICF) – 3.5- 5.0 1) Regulation a) Renal – aldosterone affect b) Extracellular-Intracellular shifts 11 2) Functions a) Acid/base balance b) Kidney’s urine concentration c) Growth & chemical reactions d) Assists with glucose conversion, amino acid to proteins e) Nerve impulses of skeletal musculo system f) Opens Na channels 3) Hypokalemia a) Causes: inadequate intake, excessive GI & renal loss (1) Kidneys – diuretic therapy (thiazide & loop) (2) Magnesium depletion present with K loss (3) Stressors (trauma) with aldosterone & cortisol (4) Adrenal tumors b) Manifestations (occurs at 3.0 or less) (1) Nausea, vomiting, abdominal distention (2) Cardiovascular – hypotension, digitalis toxicity PVC’s, prolong PR with depressed ST, flat T-wave (3) Weakness, tired, leg cramps 4) Hyperkalemia above 5.0 a) Causes (1) Decrease renal excretions (aldosterone) (2) Excessive rapid administration (3) Movement of K from intracellular to ECF b) Manifestations (1) Neuromuscular excitability (2) Cardiovascular (a) Peaked T-waves (b) Wide QRS complex (c) Disappearance of P (d) Slow HR (e) V-tach/V-fib 5) Calcium, Phosphate, Magnesium a) Parathyroid (calcium & phosphate) (1) Hypoparathyroid (a) Hyposecretion parathyroid gland (b) Manifestation: tetany, spasms, convulsions, anxiety, lethargy blurred vision (2) Hyperparathyroid (a) Hypersecretion parathyroid (b) Manifestation: Bone demineralization, b) Calcium (stored in bone; excreted by kidney) (1) Enters thru GI (2) Functions 12 (a) Neuronal excitability (b) Releases hormones (c) Muscle contractions (d) Release neurotransmitter (e) Blood clotting (f)Cardiac contractility (3) Hypocalcemia (a) Causes [1] Impaired mobilization [2] Abnormal losses by kidney [3] Increased protein binding [4] Soft tissue grabbing Acute pancreatitis (b) Manifestation [1] Cramping [2] Hyperactive reflexes [3] Tetany [4] Positive Chvostek & Trousseau’ signs [5] Hypotension [6] Prolonged QT [7] Bone pain & fracture (4) Hypercalcemia (a) Causes [1] Excessive Vit D [2] Excessive Ca in diet [3] Malignant tumors [4] Thiazide diuretic [5] Lithium therapy [6] Prolonged immobilization (b) Manifestation [1] Loss of muscle tone [2] Lethargy [3] Hypertension [4] Short QT [5] Heart block AV [6] Kidney stones [7] Constipation c) Phosphate (intracellular anion) (1) Function (a) Bone formation (b) Formation ATP (c) Metabolism fat, protein, carbohydrate (d) Acid/base buffer (2) Hypophosphatemia (a) Causes 13 [1] Intestinal absorption lack [2] Increase renal loss [3] Alcoholism [4] Glucose administration [5] Respiratory alkalosis (b) Manifestation [1] Confusion [2] Seizures [3] Joint stiffness & bone pain [4] Platelet disorders [5] Impaired WBC (3) Hyperphosphatemia (a) Causes [1] Renal failure [2] Excessive administration (b) Manifestation (similar to Ca loss) [1] Tetany [2] Hypotension [3] Cardiac dysrhythmia d) Magnesium (intracellular anion) (1) Function (a) Intracellular enzymes reaction (b) Replication & transcription DNA (c) Na/K pump (d) Nerve conduction (e) Ion transport & Ca channel activity (2) Hypomagnesemia (a) Causes [1] Alcoholism [2] Malnutrition [3] Small bowel bypass surgery [4] Diuretic therapy [5] Hyperparathyroidism [6] Hyperaldosteronism [7] DKA (b) Manifestation [1] Positive Babinski, Chvostek, Trousseau [2] Tachycardia [3] Hypertension [4] Cardiac dysrhythmia (3) Hypomagnesaemia (a) Causes [1] Excessive intake [2] Decrease excretion – ARF 14 (b) Manifestation [1] Coma, confusion [2] Hypotension [3] Cardiac arrest 4. Acid-Base Balance (pH -7.35-7.45; PCO2 – 35-45; HCO3 – 22-29) a. Acids – gives up a hydrogen ion b. Base- accepts a hydrogen ion c. Acids in Body 1) Carbonic acid a) Dissociates into water & CO2 (CO2 eliminated by lung) 2) Nonvolatile Noncarbonic d. Regulation of pH = buffers + renal+ respiratory 1) Buffers intracellular & extracellular – limited; once combined can’t do any more a) Protein (function as acid or base) – albumin major (1) Plasma protein & RBC (2) ICF – structural proteins prevent RBC destruction b) Carbonic acid &Bicarbonate (metabolism & kidney) (1) CO2 converts to carbonic acid then H2O & bicarb (2) Prevent pH changes by metabolic acids (3) Co2 excreted by lungs (4) Body has large bicarb reserves for combin c) Phosphate buffer (1) ECF – supportive role in pH control due to high bicarb in ECF (2) ICF – major role since very high concentration here 2) Respiratory (rapid) – removal CO2 a) Increases or decreases in respiratory rate 3) Renal (long term) – removal or conserve H ions/bicarb a) Hydrogen Ion elimination & bicarb conserving b) Hydrogen & Potassium ion compete for elimination c) NaCl-bicarbonate exchange e. Acidosis (pH below 7.35) 1) Metabolic (pH < 7.35, PCO2 – normal/decreased, HCO3 – Decreased) a) Causes (1) DKA (2) Fasting & starvation (3) Kidney failure 15 (4) Diarrhea (5) Poisoning ethylene glycol, methanol, salicylate (6) Lactic acidosis (7) Intestinal suctioning b) Manifestation (1) Nausea & vomiting (2) Weakness, lethargy, stupor, coma (3) Decreased HR, cardiac dysrhythmia (4) Increased RR, Kussmaul breathing, (5) Ammonia in urine (6) Hyperkalemia c) Compensation (1) Respiratory hyperventilation (2) Kidney increased H ion excretion with bicarb conserving (slower route) 2) Respiratory (pH < 7.35; PCO2 > 45; HCO3 normal or < 24) a) Causes (1) Drug overdose (2) Lung diseases (3) Chest injuries (4) Obesity b) Manifestations (1) Confusion, depression, stupor c) Compensation (1) Improve ventilation f. Alkalosis (pH above 7.45) 1) Metabolic (pH > 7.45; PCO2 – normal or decreased; HCO3increased) a Causes (1) Excessive intake alkali/bicarbonate (2) Excessive H loss (vomiting, GI suction, Diuretic therapy, GI binge-purge b. Manifestations (1) Confusion, tetany, convulsions (2) Hypotension, dysrhythmia c. Compensation (1) Respiratory rate decreased (2) H ion retention, bicarb excretion 2) Respiratory (pH> 7.45; PCO2 > 45, HCO3 – normal or low) a. Causes (1) Hyperventilation (2) Lung disease (3) Elevated blood ammonia level 16 (4) Salicylate toxicity (5) Fever b. Manifestation (1) Dizziness, light-headedness (2) Numbness & tingling fingers (3) Seizures c. Compensation (1) Slow respiration down III. Alterations A. Kidney Stones 1. Types a. Calcium b. Struvite c. Uric acid/cystine 2. S&S – flank pain, sometimes fever, diaphoresis, nausea/vomiting B. Urinary tract infection 1. Causes – infection, bacteria, tubes 2. S&S – pain on urination, frequency, burning sensation, fever sometimes, cloudy urine specimen C. Acute Renal Failure – acute & mostly reversible 1. Causes - hypotension D. Chronic – loss of nephron function not reversible E. Benign Prostatic Hypertrophy – outflow issue F. Trauma - blunt 1. Bleeding meatus, bleeding specimen G. Acute Tubular necrosis