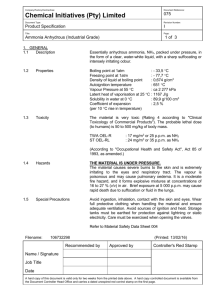
Ammonia
advertisement

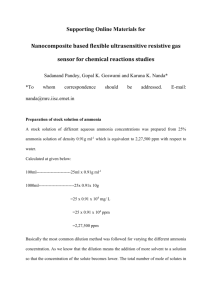
Ammonia Ammonia is produced in the gastrointestinal tract by the action of bacterial enzymes on proteins and amino acids. It enters the portal circulation and is normally metabolized in the liver to urea and glutamine. When the liver is unable to perform this function, increased amounts of ammonia enter the arterial circulation and diffuse across the blood-brain barrier. Helicobacter pylori in the stomach appear to be an important source of ammonia in patients with cirrhosis. The use of ammonia for monitoring patients with hepatic encephalopathy is controversial. It is unlikely that ammonia is solely responsible for the encephalopathy of hepatic insufficiency. Plasma ammonia levels have usually been found to correlate poorly with the clinical stage of hepatic encephalopathy. A normal level does not rule out early stage hepatic encephalopathy. Measuring plasma ammonia may be useful in suggesting a hepatic origin for an encephalopathy of unknown origin. It is not useful in patients with known liver disease. Elevated levels are also seen in: Reye's syndrome and other urea cycle enzyme deficiencies Acute leukemia Bone marrow transplantation Blood transfusion Portal-systemic shunts Gastrointestinal bleeding Chronic renal failure Many factors can affect ammonia levels: Age Four- to eightfold higher in neonates; two- to threefold higher in children ,3 years; reaches adult concentrations by adolescence Specimen source: Arterial ammonia is higher than venous; differences are greater in renal, hepatic disease; capillary blood shows falsely increased because of NH3 is present in sweat if skin inadequately cleaned. Arterial NH3 correlates better with change in liver function than venous NH3; tourniquet use, clenching fist increase venous NH3 Exercise Increases up to threefold after exercise. Increase is greater in males than in females. Smoking Increases 10 mmol/L after 1 cigarette Delay in analysis NH3 increases because of metabolism by red blood cells: 20% in 1 h and 100% by 2 h. Use of ice water, rapid centrifugation, and separation of plasma minimize increases; rate of increase higher in liver disease because of high GGT activity in specimen releasing NH3 from peptides Other factors Increased in acute leukemia, blood transfusion, bone marrow transplantation, portal-systemic shunts, gastrointestinal bleeding, or high protein intake Medications Valproic acid and glycine (in irrigation fluids used in prostate, endometrial resection) increase NH3 production Reference range is 10 - 40 umol/L. Cautions Ideally, arterial, rather than venous, specimens should be used Plasma should be separated from cells within 15 min of collection to prevent artifactual increases in NH3 Blood should be drawn without a tourniquet and then placed in ice for immediate transport to the lab. The tube should be full and must be kept tightly stoppered. It should be centrifuged immediately and the plasma separated into a screw top plastic vial. If the vial cannot be delivered to the lab immediately, it should be frozen at -70 C. Reference D. Robert Dufour,John A. Lott, Frederick S. Nolte, David R. Gretch,Raymond S. Koff, and Leonard B. Seeff Diagnosis and Monitoring of Hepatic Injury. I. Performance Characteristics of Laboratory Tests Clinical Chemistry 46:12 2027–2049 (2000) Howanitz JH, Howanitz PJ, Skrodzki CA, Iwanski JA. Influences of specimen processing and storage conditions on results for plasma ammonia. Clin Chem 1984;30:906–8.