Shortage of Non-Consultant Hospital Doctors (NCHDs)
advertisement

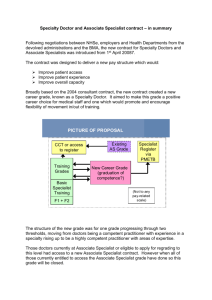
Submission to Joint Committee on Health and Children, Houses of the Oireachtas Thursday, 13th October 2011 This is a joint submission from the Royal College of Surgeons in Ireland, the Royal College of Physicians of Ireland and the Institute of Obstetricians and Gynaecologists. The career path for a doctor trained in Ireland ideally should follow structured training route from the point of entry to medical school to certification as a specialist (e.g. GP; Orthopaedic Surgeon; Gastroenterologist, Pathologist, Obstetrician, Public Health Specialist etc.) Below is a short summary of the steps within this training system. Medical School: Entry as an undergraduate or at graduate level. The undergraduate programme is a five or six year programme. The postgraduate programme is a four-year programme open to graduates from any discipline. Intern Year: The intern year is the first level of postgraduate medical training. Successful completion of the intern year leads to the award, by the Medical Council (of Ireland), of a Certificate of Experience. This year consists of two or three rotations i.e. time spent working in Medicine, Surgery and another specialty such as Psychiatry or General Practice. Basic Specialty Training: This programme commences after the intern year at Senior House Officer level and is of two-year to three-year duration. The trainees follow a structured curriculum, record training activity in a logbook, undertake assessments and rotate through a number of posts in order to obtain a broad grounding in all aspects of the specialty. For example a typical BST rotation in Medicine could include 3 to 4 month periods in Cardiology, Endocrinology, Gastroenterology, Respiratory etc. As well as providing a broadly-based training in these areas, it also allows the trainee doctor to decide on their future preference. Higher Specialist Training: This is a five to six year structured programme. Entry onto the Higher Specialist Training Programme is by competitive interview. The trainee follows a structured curriculum, records training activity in a logbook, undertakes assessments and rotates through a number of posts. The successful trainee is awarded a Certificate of Satisfactory Completion of Specialist Training. With this certification, which is granted under the auspices of the Medical Council and is internationally recognisable, the doctor is eligible to enter the specialist division of the Medical Council Register and apply for a Consultant post. While the optimum path for medical graduates it to progress from intern year to Basic Specialty Training to Higher Specialty Training to become a fully qualified specialist, there is always a degree of attrition in the system. The reasons for this attrition vary and include the fact that many Irish doctors choose to work abroad for a time to gain additional experience; or indeed there may be family reasons for not progressing from one stage of training to another. Some doctors who complete Basic Specialty Training may not enter the Higher Specialist Training programme either by choice or due to an unsuccessful application to the programme. The majority of doctors who fall into this category will enter into Registrar service posts. It should be noted that there is a significant cohort of NCHDs in Ireland who have been recruited directly into service posts. The majority of the NCHD posts which are vacant within the Irish healthcare system are designated “service” posts – that is the doctors in those posts are not engaged in a structured specialist training programme. Currently the number of doctors in these posts could be as high as 1000. NCHD Shortage The acute shortage of NCHDs is a workforce challenge that has been on-going within the Irish Health System for several years. This challenge poses a real threat to the integrity of the overall healthcare delivery system. Urgent and well-informed action steps are thus required to increase the capacity and flexibility of our mid-level clinical workforce to ensure sustainable service delivery. The primary reason for the NCHD shortage is that many more Irish medical graduates than previously are choosing to work abroad and far fewer overseas doctors are choosing to work in Ireland. Put simply, Ireland is no longer an attractive destination for NCHDs. The reasons behind this declining numbers of doctors working in the health service are multiple and complex. This shortage will not be corrected through aggressive overseas recruitment. Some of the key reasons behind the decline in NCHDs in the Irish Health Service; as has been previously highlighted in several publications include; Medical Migration Medicine is a global market. Currently there is a worldwide shortage of doctors Easier access for doctors into “alternative” markets in other jurisdictions Aggressive recruitment by other countries resulting in a more competitive environment for the attraction and retention of doctors Career Progression The number of posts providing postgraduate training has been greatly reduced in recent years to deliver only against consultant level manpower requirements. The recent changes have resulted in many of those posts been designated as “service only.” This has made them considerably less attractive for overseas graduates seeking career advancement. For NCHD’s not in training, there is no career development or structures available to them. In the past overseas doctors came to Ireland to train. Perception of lack of career opportunities in Ireland Service Pressures Service delivery is today very dependent upon NCHDs, 60% of whom come from non EEA countries. The current service delivery issues which have arisen from the budget cuts (elective beds, lists cancelled, A&E etc) make the learning environment even more frustrated for all NCHDs and Interns. Quality of Training Programmes Immense pressure on service has created a negative environment for training – many trainees report not being available to participate in mandatory training activities Clarity of progression through training Experience in Employment Slow introduction of the EWTD with consequent implications for work/life balance General breakdown in trust between junior doctors and the system Conclusion It is the view of the Colleges’ that there is a need for a comprehensive, but focussed, manpower planning exercise across the health service. This might include the examination of the development of new grades (either medical or non-medical) and extending the scope of practice of existing grades. To date undertaking a meaningful manpower planning exercise has been virtually impossible due to the protracted re-configuration debate. It should also be noted that when fully implemented, the European Working Time Directive will have a major knock-on effect on the already existing manpower issues. The following actions are recommended: Creation of a rapid, high level group focusing on the reasons for the problem is recommended. A national forum on the retention of doctors in Ireland is being organised for early December – this will involve all relevant stakeholders i.e. Trainees, NCHD’s; HSE. DoHC, Colleges, Medical Schools, Unions. Restructure the workforce towards the goal of a Consultant provided service and a training cohort of NCHDs that will staff this workforce into the future and provide the training opportunities for as many of our young graduate doctors as possible; to ensure that they can obtain specialist status and be capable of independent clinical practice. Re-skilling and redeployment, task shifting, the development of the role of nurse specialists will be crucial Reconfiguration of specialist services to provide critical mass and to ensure that patients have access to services of high quality will be crucial to this process. New clinical programmes developed by the HSE in partnership with the Colleges are crucial to success in this area. Medical training should be aligned with the national clinical programmes. The fundamental question to ask is; how do we ensure that our health systems, structures and policies are effective and attractive enough to both EEA and Non EEA NCHDs so that Ireland can attract and retain the highest calibre of doctor to provide the highest level of patient care?