Standard Operating Procedure for Spontaneous Reporting
advertisement

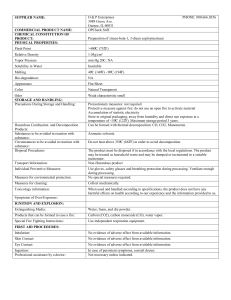
Standard Operating Procedure Spontaneous Reporting of Adverse Drug Reactions (This SOP consists of X pages (including this cover sheet and addendum). Name of National Drug Regulatory Board Drug safety Department Page # x of xxx SOP Owner xxxxx Division/Function SOP # Revision # Implementation Date Last Reviewed/Update Date Approval Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions Table of Contents Standard Operating Procedure ..................................................................................................... 1 1 Introduction ......................................................................................................................... 3 2 Purpose ................................................................................................................................ 3 3 Scope .................................................................................................................................... 4 4 Responsibilities .................................................................................................................... 4 5 Reporting Procedure ............................................................................................................ 4 5.1 Reporting : Reporting Form .......................................................................................... 4 5.2 Where to Report ............................................................................................................ 5 5.3 What to Report: Essential data elements ...................................................................... 6 5.4 Advice to reporters ........................................................................................................ 8 5.5 Report follow-up ........................................................................................................... 9 5.6 When to report .............................................................................................................. 9 5.7 Who should report......................................................................................................... 9 5.8 Reporters feedback...................................................................................................... 10 5.9 Alternative Reporting methods ................................................................................... 10 5.10 Data Entry and Data Management .......................................................................... 11 6.0 Definitions ......................................................................................................................... 12 6.1 Pharmacovigilance ...................................................................................................... 12 6.2 Pharmacovigilance Centre .......................................................................................... 12 6.3 Signal .......................................................................................................................... 12 6.4 Adverse Drug Reaction ............................................................................................... 13 6.5 Serious adverse reaction ............................................................................................. 13 6.6 Adverse Event ............................................................................................................. 13 6.7 Healthcare Proffessional ............................................................................................. 13 6.8 References ................................................................................................................... 13 Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions 1 Introduction Pharmacovigilance using a spontaneous reporting system is designed to detect Adverse Drug Reactions (ADRs) occurring in clinical practice, particularly those not previously observed in preclinical or clinical studies, to improve understanding of the potential risks, including reactions resulting from drug interactions or drug effects in particular populations, and to help provide a basis for effective patient management, drug regulation, education and consequent changes in practices by prescribers and consumers. Spontaneous reporting is dependent on the potential reporter being educated and motivated to record and submit her/his observations . This is the most common form of pharmacovigilance. It is sometimes referred to as “voluntary” reporting. In some countries this form of reporting is mandatory. Clinicians, pharmacists and community members should be trained on how, when and what to report. Targeted (stimulated, facilitated, enhanced) spontaneous reporting provides reporters with targets (drugs and ADRs of special interest), tools (standardized data collection forms and facilitation of transmission to the pharmacovigilance centers) and training as to what methods to use to overcome the known limitations of spontaneous reporting especially under-reporting. While cohort event monitoring may be "gold standard" it may not always be feasible or sustainable in resource limited settings. In such situations, spontaneous reporting may be an acceptable alternative. Spontaneous reporting also provides a long-term view of medicines. By definition, a spontaneous report is an unsolicited communication by health care professionals or consumers that describes one or more ADRs in a patient who was given one or more medicinal products and that does not derive from a study or any organized data collection scheme. 2 Purpose The purpose of this standard operating procedure is to outline a step by step approach for employing the spontaneous reporting of adverse drug reactions in monitoring medicines safety for use at National Pharmacovigilance Centers. It is applicable to all medicines. Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions 3 Scope This document is relevant to personnel intending to establish and/ or running a pharmacovigilance centre (PvC). 4 Responsibilities Identify the personnel that have a primary role in the SOP and describe how their responsibilities relate to this SOP. If necessary, include contact information. 5 Reporting Procedure 5.1 Reporting : Reporting Form 5.1.1 Each country with a pharmacovigilance centre needs to have at least one standard reporting form for documenting ADRs. 5.1.2 Pharmacovigilance centers will have, or should develop their own standard reporting form(s) 5.1.3 The reporting form needs to be available in the local language(s) 5.1.4 The reporting form should have features relating it to the responsible authority e.g. a logo, the address and contact details of the issuing institution. 5.1.5 The reporting form should be simple and easy to complete 5.1.6 The reporting form should not request too much information, particularly information that is difficult to find and record, or information that is unlikely to be used. Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions 5.1.7 The reporting form should be widely distributed to all health professionals including those who are working privately. Difficulty in finding a reporting form is a common barrier to reporting. 5.1.8 The forms should be printed on a single sheet of paper and be easily folded and sealed. 5.1.9 To facilitate postage, the return address should be printed on the outside, preferably with postage pre-paid. 5.1.10 It is desirable to have only one type of reporting form available in the country for use for all medicines. 5.1.11 The reporting form should have sufficient space in which to describe the suspected reaction(s). The form should carry a statement reassuring confidentiality of information given 5.2 Where to Report 5.2.1 Reports should be sent to the designated PvC (national,regional, or zonal). 5.2.2 If it is not practical to send the forms directly to the centre, it may be necessary to arrange points of collection at other sites such as specific hospitals or clinics. 5.2.3 The reports should be stored securely to maintain privacy. Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions 5.3 What to Report: Essential data elements 5.3.1 Patient details 5.3.1.1 Health number (depending on availability): this may be a national identifier (preferred), hospital, clinic, or programme number. 5.3.1.2 Name: full name or initials depending on the requirements of local privacy legislation. Patient identification is important for follow-up purposes and avoidance of duplication. 5.3.1.3 Address: to allow for follow-up and accurate identification. This may take various forms depending on the location. 5.3.1.4 Sex 5.3.1.5 Date of birth (preferred) or age (add ‘est’ if age is estimated). 5.3.1.6 Weight and height Pregnancy status Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions 5.3.2 Patient medical history of significance 5.3.3 Details of medicines: 5.3.3.1 Name(s): (this may be brand or generic) and formulation (e.g. tablets, syrup, injection). Reporting the brand name gives more specific information and is recommended. 5.3.3.2 Mode of administration (e.g. oral, rectal, injection). 5.3.3.3 Indication(s) for use. 5.3.3.4 Dose: Size of each dose and dosage interval is preferred. If not availablerecording the total daily dose is appropriate. 5.3.3.5 Date of commencement 5.3.3.6 Date of withdrawal. 5.3.3.7 Duration of use, if dates of commencement and withdrawal are not available. 5.3.3.8 All medicines being taken at the time of the event should be listed. Each suspect medicine can be indicated by an asterisk or any other appropriate means. 5.3.4 Reaction details 5.3.4.1 Date of onset. 5.3.4.2 Reporters should be asked to give a brief clinical description. They should not be asked to give the official pharmacovigilance reaction term. 5.3.4.3 Laboratory or other test results if available, together with units. 5.3.4.4 Seriousness and outcome of event: resolved, resolving, no change, disabling, worsening, requiring hospitalization or treatment , life-threatening, fatal (with date), congenital anomaly. 5.3.4.5 Effect of drug withdrawal and re-exposure (if relevant)re-challenge (if any). Previous medical history e.g. allergy or experience with same or similar medicine Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions 5.3.5 Reporter details 5.3.5.1 Name. 5.3.5.2 Contact details. 5.3.5.3 Status: e.g. physician, nurse, patient. 5.3.5.4 Date and place of report 5.4 Advice to reporters 5.4.1 Report any suspected adverse reaction of concern. 5.4.2 Report all suspected serious reactions. A serious reaction: results in death; is life-threatening; requires hospitalization or prolongation of hospitalization; results in persistent disability; is a congenital anomaly. 5.4.3 Report persistent adverse reactions that could threaten adherence. 5.4.4 Reporters should be advised that they need not to be sure that the medicine caused the event. Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions 5.5 Report follow-up 5.5.1 All reports of serious events should be followed up if details are incomplete. This may require the involvement of health professionals trained and appointed for this type of work. 5.5.2 Occasionally follow-up information is required to fully assess reports of non-serious events. Follow-up requests should be kept to a minimum because they can act as a deterrent to further reporting. Examples might be: a request for essential missing details; information on the final outcome; the result of re-exposure; the results of laboratory or other tests; post-mortem results from the health facility where autopsy is undertaken. 5.6 When to report 5.6.1 A report should be completed and submitted as soon as possible after the reaction happened. 5.6.2 It is better to advice reporters not to wait until final results and information such as hospital letters are received, because the report may be forgotten. These additional details can be sent to the PvC at a later date 5.7 Who should report The following is a list of potential reporters. They may work in the public or private health sectors. Physicians and dentists. Pharmacists. Nurses. Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions Other (literate) health and community workers should be encouraged to detect and report, preferably to the clinician who prescribed the treatment, or directly to the PvC. Public health programmes. Pharmaceutical companies. Patients or patient representatives. 5.8 Reporters feedback 5.8.1 Anyone who sends in a report should receive an acknowledgement letter and further reporting forms. 5.8.2 The letter should, if possible,provide some brief information about the reaction reported and measures that will be taken to potentially prevent reoccurrence in that particular patient or other patients 5.9 Alternative Reporting methods 5.9.1 Telephone. The person receiving the report should have a reporting form to record the details and make sure that essential data are not missing. 5.9.2 Fax. Sending reports by fax is equivalent to posting the report, but faster. A fax machine is a very important asset for national PvC and its major sentinel sites. 5.9.3 E-mail. A written case-report submitted by e-mail may be acceptable. Further details can be obtained by follow-up. Reporting forms can be sent to reporters as e-mail attachments and they can be e-mailed, faxed or posted to the PvC when completed. 5.9.4 The Internet. An Internet site is a valuable asset for a PvC and a reporting form could be made available for downloading or for completion online (entering data through web-based data entry) if the site is secure Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions 5.10 Data Entry and Data Management 5.10.1 All PvC should have a complete data/ case management system e.g. VigiFlow™ (see below) for managing data within the country 5.10.2 All PvC should have trained data entry personnel 5.10.3 Details of reports should be sent for international analysis to the WHO Collaborating Centre for International Drug Monitoring (UMC) at least monthly. 5.10.4 The PvC should decide which data can be transferred to WHO database (Vigibase) and when it will be transferred. The use of VigiFlow (described below) simplifies this procedure. 5.10.4.1 VigiFlow It is web-based and requires no local support or maintenance. VigiFlow provides an online database unique to the national PvC. Data entered are confidential to, and are owned by the country that enters them. VigiFlow is compatible with the international standard for exchange of individual case safety information (ICH-E2b) and provides for standardized entry of data from reports. It has built-in error avoidance features. A search and statistics module provides summary tabulations, line listings and a range of standard statistical analyses National data can be accessed and used by the national and local PvC. The data can be exported to local country databases or to marketing authorization holders (e.g. in pdf or Excel format) for ad hoc searches and to meet local analytical requirements. It provides live access to up-to-date terminologies: WHO Drug Dictionary (DD) and MedDRA and WHO Adverse Reactions Terminology (WHO-ART). Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions VigiFlow is maintained, continuously developed and provided to national PvCs by the Uppsala Monitoring Centre 6 Definitions 6.1 Pharmacovigilance Pharmacovigilance has been defined as: The science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other drug-related problem (WHO). 6.2 Pharmacovigilance Centre The Pharmacovigilance Centre (PvC) of an individual country is responsible for meeting the requirements for pharmacovigilance of all medicines and is a centre of expertise for the art and science of monitoring and analysis, and use of the analysed information for the benefit of patients. National and any regional Pharmacovigilance Centers should be set up with the approval of the authority responsible for the regulation of medicines (“regulatory authority”). The centre may function within the regulatory authority, a hospital, an academic institution or as an independent facility such as a trust or foundation. 6.3 Signal Reported information on a possible causal relationship between an adverse event and a drug, the relationship being unknown or incompletely documented previously. Usually more than a single report is required to generate a signal, depending upon the seriousness of the event and the quality of the information. (WHO) Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions 6.4 Adverse Drug Reaction A response to a medicinal product which is noxious and unintended and which occurs at doses normally used in man for the prophylaxis, diagnosis or therapy of disease or for the restoration, correction or modification of physiological function. (WHO) 6.5 Serious adverse reaction Any untoward medical occurrence that at any dose results in death, is life threatening, requires or prolongs patient hospitalization, results in persistent disability/incapacity, or is a congenital anomaly/birth defect (International Conference on Harmonization (ICH)). The term Life-threatening” in the definition of “serious” refers to an event in which the patient was at risk of death at the time of the event; it does not refer to an event, which hypothetically might have caused death if it was more severe. 6.6 Adverse Event Any untoward medical occurrence that may present during treatment with a pharmaceutical product but which does not necessarily have a casual relationship with this treatment. (WHO) 6.7 Healthcare Professional For the purposes of suspecting adverse reactions, healthcare professionals are defined as medically qualified persons such as physicians, dentists, pharmacists and nurses. 6.8 References List resources that may be useful when performing the procedure; for example, Admin policies, Municipal Code, government standards and other SOPs. Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions Standard Operating Procedure: Spontaneous Reporting of Adverse Drug Reactions