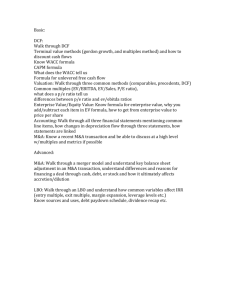
Preferred Practice Standards - ABH
advertisement

Substance Abuse Family Evaluation Preferred Practice Standards Key Contact Information .............................................................................................5 Welcome to Project SAFE ........................................................................................6 History........................................................................................................................6 Program Overview .....................................................................................................6 Project S.A.F.E Covered Services ............................................................................7 Evaluation ______________________________________________ 8 Adolescent Evaluation: .............................................................................................................. 9 Comprehensive Evaluation: ........................................................................................................ 9 Individual Therapy _______________________________________ 10 Group Therapy __________________________________________ 10 Family Therapy _________________________________________ 10 Intensive Outpatient Therapy (IOP) __________________________ 10 Partial Hospitalization Program (PHP) ______________________ 10 Urine Drug Screens ______________________________________ 11 Hair Testing ____________________________________________ 11 Treatment Levels of Care __________________________________ 11 Service Limitations and Exclusions __________________________ 12 Level of Care Guide (Table I) ................................................................................13 Level I: (SA I.1 & SA I.1) Outpatient _________________________ 13 Level of Care Guide (Table II) ...............................................................................14 Level II: (SA II.1 & MH II.1) Intensive Outpatient (IOP) _________ 14 Level of Care Guide (Table III) ..............................................................................15 Level II: SAII.5 & MH II.5 Partial Hospital & SA Day/Evening ____ 15 Referral and Authorization Process .......................................................................16 Service Authorization and Referral Process for Covered Services .......................17 Referral and Authorization Process (CHART)......................................................23 Type of Service/Level of Care ______________________________ 23 Information Needed From DCF _____________________________ 23 Information Need from the Provider _________________________ 23 Information needed or provided by ABH ______________________ 23 Authorization Requirements ________________________________ 23 Rev. 11/07 2 Reimbursement Protocol ...................................................................................24 Provider Credentialing ............................................................................................25 Reimbursement ........................................................................................................25 Reimbursement for Evaluation ..............................................................................26 DCF Responsibilities ___________________________________ 26 Provider Responsibilities _______________________________ 26 ABH Project S.A.F.E. Will ______________________________ 26 Reimbursement for Treatment ...................................................................................27 DCF Responsibilities ___________________________________ 27 Provider Responsibilities _______________________________ 27 ABH Project S.A.F.E. Will ______________________________ 28 Reimbursement for IOP or PHP Levels of Care .........................................................29 DCF Responsibilities ___________________________________ 29 Provider Responsibilities _______________________________ 29 ABH Project S.A.F.E. Will ______________________________ 29 Reimbursement for Hair Testing ................................................................................30 DCF Responsibilities ___________________________________ 30 Provider Responsibilities _______________________________ 30 ABH Project S.A.F.E. Will ______________________________ 30 Reimbursement for Random Urine Drug Screens Only ..............................................31 DCF Responsibilities ___________________________________ 31 Provider Responsibilities _______________________________ 31 ABH Project S.A.F.E. Will ______________________________ 31 Requests for Court Cost Reimbursement ....................................................................33 DCF Responsibilities ___________________________________ 33 Provider Responsibilities _______________________________ 33 ABH Project S.A.F.E. Will ______________________________ 33 Special Exceptions ..................................................................................................34 Six Tab Web Base Claim System ............................................................................36 Rev. 11/07 3 Complaints, Grievances, and Appeals ...........................................................38 Appendix A ...........................................................................................................42 CLIENT REFERRAL FORM (page 1) ________________________ 42 CLIENT REFERRAL FORM (page 2) ________________________ 43 Appendix B ..............................................................................................................44 CLIENT REPORT FORM ____________________________________ 44 PROJECT SAFE.....................................................................................................44 Appendix C ...........................................................................................................45 Needs Assessment Form _____________________________________ 45 Appendix D ..............................................................................................................46 TANF ELIGIBILITY SCREENING FORM ____________________ 46 Appendix E: Outpatient Treatment Request Downloading Procedure ...............47 Outpatient Treatment Request Downloading Procedure (page 2) __ 48 Outpatient Treatment Request Downloading Procedure (page 3) _________ 49 Appendix G ..............................................................................................................51 Special Exception _________________________________________ 51 FAQ for Project SAFE Special Exceptions ...........................................................52 (Formerly Regional Administrator’s Approval) ________________ 52 Appendix H: ............................................................................................................54 Screen Shot of Web-Based Claims System _____________________ 54 Rev. 11/07 4 Key Contact Information Advanced Behavioral Health 213 Court Street Middletown, CT 06457 Referral Hotline:…………………………1-800-272-0097 Main Number:……………………………1-860-638-5309 Billing Department……………………….1-860-704-6144 Fax:………………………………………..1-860-638-5302 Advanced Behavioral Health Website: https://www.abhct.com/ Online access to information and materials, such as newsletters, alert memos, and forms. Department of Children and Families Website: http://www.state.ct.us/dcf/ Online access to a wide variety of information related to the Department of Children and Families such as newsletters, other publications, and forms. Department of Mental Health and Addiction Services Website: http://www.dmhas.state.ct.us/ Online access to a wide variety of information related to the Department of Mental Health and Addiction Services such as newsletters, publications, and forms. Rev. 11/07 5 Welcome to Project SAFE Welcome to the Advanced Behavioral Health (ABH) Project S.A.F.E. Provider network. As a member of the Project S.A.F.E. Provider network you have joined a group of highly respected behavioral health professionals. We recognize that you share our commitment to improve the quality of life for clients by providing a continuum of high quality accessible behavioral health care services. This Preferred Practice Standards handbook has been developed to inform you of standard practice of participants in the ABH Project S.A.F.E. network The handbook begins with an introduction, states policies and procedures for referral, authorization, claims submission, and the complaints, grievances, and appeal process. Finally, the necessary forms are included, along with a glossary and index for your convenience. Services provided for ABH Project S.A.F.E. clients must be consistent with the practices encompassed in this handbook Should you have any questions, please contact ABH Project S.A.F.E. at: 1-800-272-0097 History The Department of Children and Families (DCF) initiated Project S.A.F.E. (Substance Abuse Family Evaluation) in 1995 as a way to connect its child protection system with the adult substance abuse treatment system. DCF contracted with ABH to coordinate central intake and priority access to drug screening, evaluation, and ambulatory treatment for substance abusing primary caregivers of children receiving protective services. DCF began collaborating with the Department of Mental Health and Addiction Services (DMHAS) in October 1999 to identify and address more effectively substance abuse issues and to coordinate and blend state, federal, and private resources to meet the needs of these populations. Program Overview Project S.A.F.E. is a program, jointly funded by DCF and DMHAS, designed to provide priority access to substance abuse evaluation and outpatient treatment services. Clients are eligible for Project S.A.F.E. services if they meet the following criteria: Parents or Primary Caregiver involved in child Protective Services The completed DCF Substance Abuse Screen has identified that substance use/abuse may be effecting the ability to parent effectively and substance abuse treatment or further evaluation is needed; A Referral has been made by DCF Social Worker prior to any treatment and \or evaluation service Funding for Project S.A.F.E. services is provided by DCF and DMHAS, and administered by ABH. This funding system is designed as a payer of last resort. The term ‘payer of last resort’ indicates that the Project S.A.F.E. funds are used to reimburse providers on a fee-for-service basis when there is no other source of reimbursement available. Rev. 11/07 6 Project S.A.F.E. Covered Services There are a variety of services that are reimbursed under Project S.A.F.E.’s payer of last resort system. In the following section, we will outline identify and define all services covered by Project SAFE. Rev. 11/07 7 Project S.A.F.E Covered Services There are eight basic treatment services that are reimbursable within Project S.A.F.E. Evaluation Individual Therapy (SA I.1) Group Therapy (SA I.1) Family Therapy (SA I.1) Intensive Outpatient Therapy (IOP) (SA II.1) Partial Hospitalization Program (PHP) (SA II.5) Urine Drug Screens Hair Testing The following section contains a description of these services. Evaluation Clients are referred for a Project S.A.F.E evaluation because the DCF Social Worker has completed the DCF substance abuse screen (DCF form 2110) and found reason to believe that the individual’s ability to parent effectively is impaired as a result of his/her use. The evaluation is conducted by an approved Project S.A.F.E Provider and consists of a bio-psycho-social assessment focusing on the following areas: Demographic Information Family composition and history Substance abuse history Trauma history Medical history and current medical status DSM IV TR Diagnostic formulation Drug screen results Summary and recommendations Each evaluation should contain a written narrative in the aforementioned areas. Once the evaluation is completed by the provider, the results of the evaluation should be verbally communicated to the DCF Social Worker within twenty-four (24) hours (one business day) of its completion. A written clinical summary will be forwarded to both the Social Worker and the DCF Substance Abuse Specialist within five (5) business days of the evaluation. Rev. 11/07 8 In specific cases there are two different evaluation subtypes that may be completed. They are an adolescent evaluation or a comprehensive evaluation. Adolescent Evaluation: Project S.A.F.E. also has capacity to conduct adolescent specific evaluations. The Project S.A.F.E. Adolescent Evaluation Project was initiated in (the then )Region IV to provide Substance Abuse Evaluations to adolescents who are suspected of substance abuse, but do not meet the basic Project S.A.F.E. criteria. DCF Region IV Social Workers who believe that an adolescent would benefit from a Project S.A.F.E. evaluation should complete the following forms prior to contacting the North Central Region ARG: Adolescent Screening Form Project SAFE Referral Form These two forms are then reviewed by the ARG, and approved if clinically appropriate. Once approved, the ARG or designee will call the ABH Intake Coordinator at 1-800-272-0097, and make the referral. Comprehensive Evaluation: The Comprehensive Evaluation Pilot Project began in March 2002, with the following objectives: To develop and standardize a comprehensive bio-psycho-social evaluation for Project S.A.F.E. clients; To collect comprehensive information about the clients served by Project S.A.F.E.; To provide a process for efficient and effective distribution of substance abuse evaluation results. There are ten (10) providers that are participating in the Comprehensive Evaluation Pilot Project. The referral process for this pilot project is as follows: 1. Make an evaluation referral by calling the 1-800 Project S.A.F.E line 2. Once referred, the provider utilizing a specifically designed Bio-Psycho-social Evaluation that has been standardized will evaluate the client. 3. The form itself is used to collect data and should be completed entirely by the evaluating clinician. 4. Once it is completely filled out, the form is faxed to ABH within thirty (30) days of the date of service for processing. 5. ABH enters all of the information into a database, and then distributes a data processed form to the following: Referring DCF Social Worker; Treatment Provider; Regional Substance Abuse Specialist (if requested). Rev. 11/07 9 Individual Therapy Individual therapy consists of one to one therapy in duration of up to one hour, with a frequency of no more than once weekly and no less than once per month. Treatment focuses on reducing symptoms, improving function, maintaining abstinence and relapse prevention. Group Therapy Group therapy consists of therapy in duration up to one and a half hours, with a frequency of once weekly. Treatment focuses on reducing symptoms, providing psycho-education, improving functioning, relapse prevention and maintenance of abstinence. Groups should be limited to no more than twelve (12) clients per group session. Family Therapy Family therapy consists of therapy sessions with a client and one or more individual(s) identified by the client as family, with duration of up to one hour, a frequency of no more than once weekly. Treatment focuses on building and maintaining supports for recovery, repairing relationships, reducing symptoms, providing psycho-education and maintenance of abstinence. Intensive Outpatient Therapy (IOP) A non-residential service provided in a general hospital, private freestanding psychiatric hospital, state operated facility or in a facility licensed by the Department of Public Health as a “Psychiatric Outpatient Clinic for Adults”. IOP services provides each client with three to four (3-4) hours per day, three to five (3-5) days per week of clinically intensive programming based on an individualized treatment plan. Treatment focuses on reducing symptoms, improving functioning, maintaining community connection and relapse prevention. As a client is preparing for discharge, titration of IOP may occur, decreasing the frequency to less than three (3) times per week. IOP must include one therapy session per day, inclusive of (at least) one individual therapy session per week. Random drug screens can be completed on the same day that a patient attends and are reimbursed separately. Partial Hospitalization Program (PHP) A non-residential service provided in a general hospital, private freestanding psychiatric hospital, state operated facility or by a provider that is a non-profit entity that involves ambulatory intensive psychiatric and/or substance abuse treatment services. PHP services are designed to serve individuals with significant impairment resulting from substance abuse as well as cooccurring psychiatric disorders. These services target adults who have recently been discharged from inpatient facilities, or whose admission to inpatient care may be prevented by treatment in PHP program. PHP consists of therapeutic programming of a minimum of four (4) hours per day, at least four (4) days per week, based on a comprehensive and coordinated individualized treatment plan involving the use of multiple concurrent treatment services and modalities. Treatment focuses on reducing symptoms, improving functioning, maintaining community connection, and relapse prevention. As a client is preparing for discharge, titration of PHP may occur, decreasing the frequency to less than four (4) times per week. PHP must include one therapy session per day, inclusive of (at least) one individual therapy session per week. Random drug screens can be completed on the same day that a patient attends and are reimbursed separately. Rev. 11/07 10 Urine Drug Screens Urine drug screens are used to determine the recent use/abuse of substances. Random urine drug screens are defined as two (2) urine drug screens per week for a period of six (6) weeks. Random screens should not occur on the same day and time each week. In order for the screens to be random, the client may be contacted by the treatment provider and asked to come in within the next twenty- four (24) hours for a drug screen, provided it is not on a day when treatment services are provided. Random drug screens can also be requested for a client who is not in active treatment under the following circumstances: In response to a court ordered request or; Has had an evaluation within the past six (6) months. Hair Testing Hair testing is utilized to determine a three-month history of substance use/abuse history prior to the hair test. Careful collection of samples by authorized treatment providers following collection guidelines is necessary to ensure effective use of hair testing. Positive hair test results can be further analyzed to determine if the client’s use/abuse of substances occurred within 30/60/90 days prior to collection. This multi-sectional testing can be performed on a positive sample per request of the referring DCF Social Worker. A hair test may be requested for some of the following reasons: Family reunification planning is expected to occur in the immediate future. DCF or provider staff has reason to believe that client has attempted to alter the urine drug screens or failed to keep scheduled appointments. Central or Area Office has concerns about a particular high risk or high profile case. DCF staff identifies cases in which domestic violence is connected with substance abuse. The Court requires documentation of historical drug use during a 30/60/90 day period DCF staff identifies abuse/neglect cases in which the primary caregivers are said to be in recovery from substance abuse. Treatment Levels of Care In this section guidelines adapted from the ASAM Patient Placement Criteria for the Treatment of Substance Related Disorders, Second Edition Revised (ASAM PPC-2R), published by the American Society of Addiction Medicine ASAM in 2001 are used to define treatment levels of care. Each level of care has general characteristics and criteria. Project S.A.F.E provides reimbursement to providers for all of the outpatient levels of care: Outpatient Services – Level I SA1.1 Individual Counseling, Family Counseling, Group Counseling, Urine Screens, and Hair test Intensive Outpatient Services – Level II, SA II.1 Partial Hospitalization Program Services – Level II, SA II.5 In an effort to provide general guidelines, we have included a level of care (page 13-15) table in this Preferred Practices document. It is intended as a guide for clinical practice rather than a set of rules. Rev. 11/07 11 Service Limitations and Exclusions A. The following limitations shall apply to substance abuse services performed under Project S.A.F.E a. Covered services and procedures are limited to those listed in the Project S.A.F.E. fee schedule b. At the time of initial referral from the DCF Social Worker the following types of visits can be authorized: i. One (1) evaluation ii. One (1) urine drug screen iii. Twelve (12) random drug screens iv. One (1) hair test v. Undisclosed number of outpatient SA I.1 levels of care c. Medication Management is not a reimbursable service under Project S.A.F.E. B. Reimbursement for the following behavioral health services is excluded under Project S.A.F.E a. Psychiatric evaluation b. Medication Management c. Psychological Assessment d. Services that Project S.A.F.E., DCF and DMHAS determine are not directly related to the diagnosis and treatment of a behavioral health disorder or those that do not reduce symptoms and/or psychological distress. e. Services, consultation or information provided over the telephone f. Services that Project S.A.F.E., DCF and DMHAS determine are primarily for vocational or educational guidance or that is related solely to a specific employment opportunity, work skill work setting and/or the development of an academic skill. g. Breathalyzer h. Methadone Maintenance C. Project S.A.F.E. shall not reimburse for inpatient or residential levels of care. D. Project S.A.F.E. does not reimburse for psychiatric evaluation or medication management. E. Project S.A.F.E. does not reimburse for any required spend-down funding, and/or copayment requirements Rev. 11/07 12 Level of Care Guide (Table I) Level I: (SA I.1 & MH I.1) Outpatient Level of Care Guide Level of Care Level I: (SA I.1 & MH I.1) Outpatient ASAM Dimension Description of general criteria Dimension 1 Patient has no signs and symptoms of withdrawal. If any biomedical conditions are present, they are sufficiently stable to permit participation in outpatient treatment. Any symptoms of a co-occurring disorder are generally stable, may require some monitoring, and do not interfere with the patient’s ability to focus on addiction treatment issues. Mental status does not preclude ability to understand information, and participate in treatment. Patient is willing to participate and cooperate with treatment, acknowledges that he or she has a substance–related problem and wants to change. If having difficulty with the above, the patient may need monitoring. Patient is able to achieve abstinence and/or an awareness of a substance related problem The patient’s psychosocial environment is sufficient to support treatment feasibility. Dimension 2 Dimension 3 Dimension 4 Dimension 5 Dimension 6 Rev. 11/07 13 Level of Care Guide (Table II) Level II: (SA II.1 & MH II.1) Intensive Outpatient (IOP) Level of Care Guide (continued) Level of Care ASAM Dimension Description of general criteria Level II: (SA II.1 & MH II.1) Intensive Outpatient (IOP) Dimension 1 Patient has no signs and symptoms of withdrawal. If any biomedical conditions are present, they are sufficiently stable to permit participation in outpatient treatment. Patient engages in abuse of family or significant others, and requires intensive outpatient treatment to reduce the risk of further deterioration, or the patient has a diagnosis requiring intensive outpatient monitoring to minimize distractions from recovery. Patients meeting Dimension 3 description require dual diagnosis treatment. Efforts at outpatient level (SA I.1 or MH I.1) have failed to promote recovery, or although the patient is willing to participate, their perspective inhibits ability to make behavior change with repeated structured intervention. The patient has been an active participant at a less intensive level of care, he or she is experiencing an intensification of symptoms, and his or her level of functioning is deteriorating. The patient lacks social contacts so as to jeopardized recovery and/or continued exposure to school, work, or living environment will render recovery unlikely. Dimension 2 Dimension 3 Dimension 4 Dimension 5 Dimension 6 Rev. 11/07 14 Level of Care Guide (Table III) Level II: SAII.5 & MH II.5 Partial Hospital & SA Day/Evening Level of Care Guide (continued) Level of Care ASAM Dimension Description of general criteria Level II: (SA II.5 & MH II.5) Partial Hospital & SA Day/Evening Dimension 1 Patient has no signs and symptoms of withdrawal. If any biomedical conditions are present, they are sufficiently stable to permit participation in outpatient treatment, however they may provide distraction from recovery efforts. The patient’s mental status history is characterized by a mild to moderate psychiatric decompensation on discontinuation of the drug(s) of abuse. Patients meeting Dimension 3 description require dual diagnosis treatment. Efforts at another treatment level have failed and structured programmatic milieu interventions are not likely to succeed at Level II.1, or, although the patient is willing to participate, their perspective and lack of impulse control inhibits ability to make behavior change with repeated structured intervention. The patient has been an active participant at a less intensive level of care, he or she is experiencing an intensification of symptoms, and his or her level of functioning is deteriorating; or a lack of awareness of relapse triggers creates is a high likelihood of relapse. The patient’s family members or significant others who live with the patient are not supportive of recovery goals, and continued exposure to school, work, or living environment will render recovery unlikely. Dimension 2 Dimension 3 Dimension 4 Dimension 5 Dimension 6 Rev. 11/07 15 Referral and Authorization Process There are a variety of procedures in which each party of Project S.A.F.E. is required to follow. In the following section, we will outline what we (ABH) will do, and what DCF and/or the Provider are required to do, in order that our clients receive services in an efficient, professional, and timely manner. Rev. 11/07 16 Service Authorization and Referral Process for Covered Services One of Project S.A.F.E.’s goals is to ensure that adults involved in the child welfare system have priority access to drug screening, substance abuse evaluations and outpatient services. By definition Priority Access means once contacted with an evaluation referral the provider will offer an evaluation appointment within five (5) business days. If requests are urgent, the provider should attempt to offer an appointment within twenty-four (24) hours. The following section sets forth the general requirements for referrals and service authorization for service types and levels of care. 1. Initial Referral An initial referral is the first time DCF Worker has called ABH Project S.A.F.E. regarding an identified client to make a referral. a. An initial referral must be made to ABH in order for an individual to be considered a Project S.A.F.E. client. b. The DCF Social Worker must obtain a release of information for ABH prior to making the referral. c. A referral will only be accepted from a DCF Social Worker or other DCF designated staff (Supervisor, Area Resource Group, Central Office). d. To make a referral the DCF Social Worker calls the ABH Project S.A.F.E. intake line (1-800-272-0097). e. The DCF worker will be asked a series of questions including which Provider they would like the client to see. f. The Project S.A.F.E. Intake Coordinator(s) will enter the information into the database all information asked, creating a Project S.A.F.E. Client ID number and electronic record. The electronic record will include demographic information, substance use concern as identified by the DCF Social Worker and an initial authorization for the service/services being requested. g. The Project S.A.F.E. intake coordinator will then fax the referral (which also serves as the authorization) to the Project S.A.F.E. Provider. 2. Evaluation: The DCF Social Worker requests an evaluation once the DCF substance abuse screen (DCF form 2110) is completed and there is suspicion that the individuals’ ability to parent effectively is impaired as a result of substance use. To include a urine drug screen as part of the evaluation the DCF Social Worker should also request one (1) urine drug screen. 1. Prior to making the ABH Project S.A.F.E. referral, the DCF Social Worker will obtain a release of information from the client for Advanced Behavioral Health and the provider. 2. The DCF Social Worker calls the Intake Coordinators at 1-800-272-0097. 3. The DCF Social Worker will provide basic demographics, reason for referral and any updated information. 4. Once the Telephonic referral is completed, the Project S.A.F.E. Intake Coordinator will fax the client referral form and substance abuse screening Rev. 11/07 17 form [Appendix A] to the Project S.A.F.E. Provider. This serves as an authorization for the evaluation. 5. The DCF Social Worker should fax the release of information to the provider. Providers will be unable to schedule an appointment without a signed release of information. 6. The Provider should verify the client’s health insurance using the EDS. If the client has insurance the Provider should submit a claim to both ABH Project S.A.F.E. and the client’s health insurance carrier. ABH Project S.A.F.E. is the payer of last resort. 7. The preferred location for conducting evaluations is at the Provider’s place of business; in addition the provider is expected to conduct a chain of custody (See glossary of terms) urine screen. 8. Upon completing the evaluation, results should be verbally communicated to the DCF Social Worker within twenty-four hours (one business day). 9. A written clinical summary should follow this verbal communication within five (5) business days. The summary should contain the following minimum information: Demographic information Family composition and history Substance abuse history Trauma history Medical history and current medical status DSM IV TR Diagnostic formulation Drug screen results 10. Upon completion of the evaluation Providers are responsible for faxing the following forms to Project S.A.F.E. 860-638-5302 claims department a. Client Report Form [Appendix B] b. Needs Assessment Form (for females only) [Appendix C] c. TANF Eligibility Form [Appendix D] d. OTR completed if the Provider is recommending IOP or PHP levels of care. 11. The Provider must inform the DCF Social Worker within twenty- four hours when a client fails to show for a drug screen and/or evaluation before rescheduling. It should be decided jointly who will contact the client to reschedule. If a client has a history of “no shows” with the assigned Project S.A.F.E. Provider, while reasonable efforts should be made to provide priority access, the Provider may apply their agency’s policy regarding rescheduling. The appointment has to be rescheduled and the client seen within 45 days of the date of the original referral date. If this does not occur the DCF Social Worker has to make another referral by calling the Project S.A.F.E. Intake Coordinators. 3. Outpatient 1.1 levels of care: There are three (3) basic Outpatient services, which falls under 1.1 levels of care that are reimbursable within Project S.A.F.E. (individual psychotherapy, group counseling, and family counseling). Rev. 11/07 18 a. The DCF Social Worker will make a telephonic treatment referral by calling the intake coordinator at the ABH Project S.A.F.E.1-800 272-0097 b. The DCF Social Worker will need to provide: i. Release of Information ii. Client Insurance Information iii. Client Social Security Number iv. Results of DCF Substance Abuse Screen v. Basic Demographic Information vi. Reason for Referral c. The intake coordinator will enter the referral information into the Project S.A.F.E. data system and fax the referral. This referral also serves as the authorization for the treatment provider. d. The authorizations will allow the provider to receive reimbursement for the provision of individual, group and /or family/couple counseling treatment. e. The treatment must begin within forty-five (45) days of the start date of the referral. If the client does not attend treatment within the forty-five (45) days of the start date of the referral, then the DCF Social Worker must make a new treatment only referral. The Provider should notify the DCF Social Worker when a referral lapses beyond the 45-day limit to request that the DCF Social Worker call in a treatment only referral. f. The Provider is to notify the DCF Social Worker if the client does not show for their treatment appointment. g. The Provider should regularly report to DCF the course of the client’s treatment. 4. IOP: IOP services provides each client with three to four (3-4) hours per day, three to five (3-5) days per week of clinically intensive programming based on an individualized treatment plan. a. IOP services may be recommended based on a bio-psycho-social evaluation that has been completed within six (6) months of the service request. b. The Provider must complete an OTR to ABH via facsimile at 860-638-5302. The OTR can be downloaded from the following web address: www.abhct.com (for process see Appendix E). c. Services will be authorized based on a Utilization Review process d. Clinical staff at ABH will review all OTR information for clinical appropriateness and provider compliance with submission criteria. i. Submission criteria 1. The OTR should be completed in its entirety. 2. The OTR should be submitted prior to admission to the IOP level of care. 3. The Provider should promptly respond to any inquires for supporting clinical information. e. ABH will help to educate treatment providers about clinically appropriate treatment planning and decision-making processes regarding level of care, review OTR within three (3) business days. An OTR will be processed with one of the following four outcomes: Rev. 11/07 19 i. Authorization – an authorization will be processed, entered into the ABH system and fax authorization notification will be generated and forwarded to the provider ii. Request for Additional Information- the clinician submitting the OTR will be contacted telephonically, with a request for additional information; iii. Administrative Denial – a denial letter will be issued based on procedural exceptions; iv. Clinical Denial – a clinical denial will be issued based upon a review of clinical information. f. ABH will provide an appropriate appeal process for all adverse determinations. 5. PHP: PHP consists of therapeutic programming with a minimum of four (4) hours per day, at least four (4) days per week, based on a comprehensive and coordinated individualized treatment plan involving the use of multiple concurrent treatment services and modalities. a. PHP services may be recommended based on a bio-psycho-social evaluation that has been completed within six (6) months. b. The Provider must complete an OTR and fax to ABH at 860-638-5302. The OTR can be downloaded from the following web address: www.abhct.com (for process see Appendix E). c. Services will be authorized based on a Utilization Review process d. Clinical staff at ABH will review all OTR information for clinical appropriateness and provider compliance with submission criteria. i. Submission criteria 1. The OTR should be completed in its entirety. 2. The OTR should be submitted prior to admission to the IOP level of care. 3. The Provider should promptly respond to any inquires for supporting clinical information. e. ABH will review the OTR within three (3) business days. An OTR will be processed with one of the following four outcomes: i. Authorization – an authorization will be processed, entered into the ABH system and an authorization notification will be generated and forwarded to the provider ii. Request for Additional Information- the clinician submitting the OTR will be contacted telephonically, with a request for additional information; iii. Administrative Denial – a denial letter will be issued based on procedural exceptions; iv. Clinical Denial – a clinical denial will be issued based upon a review of clinical information. f. ABH will provide an appropriate appeal process for all adverse determinations. 6. Random Drug Screens: Random urine drug screens are defined as two (2) urine drug screens per week for a period of six (6) weeks and should not occur on the same day and time each week. Urine Screens can be requested for clients who are not in treatment if in response to a court ordered request. Rev. 11/07 20 a. The DCF Social Worker makes a telephonic referral. This referral results in an authorization for services b. ABH Project S.A.F.E. will authorize 12 random urine screens. c. The screens can be initiated at any time during the next forty-five (45) days. Once the random screens have begun they may continue for a period of no longer than six (6) weeks. d. The Provider is required to collect all urine samples using the chain of custody protocol as indicated on the reverse side of the chain of custody form. e. The Provider, to schedule a random screen, will contact the client asking the client to come in within the next twenty-four (24) hours for a drug screen, provided it is not on a day when treatment services are provided. f. The Provider will verbally communicate all toxicology screen results to the DCF Social Worker within forty-eight (48) hours. Written results should be faxed to the DCF Social Worker within 24 hours of receipt of written correspondence from the lab. 7. Extended Drug Screens (e.g. Opiate Search) a. The DCF worker consults with the SAS to receive authorization for any extended drug screens, once the standard screen has been completed with a positive result. b. If a urine screen is positive for heroin an Extended Opiate Search can be conducted by having the Substance Abuse Specialist or designee of the Substance Abuse Division approve this test by calling the ABH Billing Coordinator at 860704-6144. An Extended Opiate Search can differentiate the positive opiate as heroin, hydrocodone, hydromorphone, morphine and oxycodone. c. Once this has been obtained the SAS must call the ABH Billing Coordinator at 860-704-6144 with client name, ABH number, and verification of approval from the Substance Abuse Specialist. d. The provider will then be contacted by the SAS or DCF social worker notifying of approval. e. The provider will then complete the LabCorp request. f. When results of the extended drug screen are received, the results should be communicated to DCF upon receipt. g. When received, the Provider should forward the specific LabCorp Invoice to ABH via mail 213 Court Street, Middletown, CT 06457 or fax to 860-638-5302. 8. Hair Testing: Hair testing is utilized to determine the substance use/abuse history of a client up to three (3) months prior to the sample collection. This ‘standard’ test will indicate whether a client has used any of the following substances during that period: Cocaine Opiates PCP; Methamphetamine Marijuana/THC Rev. 11/07 21 In addition, when a positive result is determined by the standard hair test results, a multisectional test can be performed per request of the referring DCF Social Worker. b. The DCF Social Worker will discuss the necessity and request for approval with the Substance Abuse Specialist and/ or supervisor or designee in the Substance Abuse Division. c. The DCF Social Worker then calls the ABH Intake Coordinator at 1-800-2720097 for the hair test referral and provides the following information: i. Name of person authorizing the test (SAS or designee has to approve before the referral is called into ABH Project S.A.F.E.) ii. Name and ABH number of the client d. ABH Project S.A.F.E. identifies the provider performing the test, enters an authorization and faxes notification to that provider. e. The Provider will complete a Standard Test Request Form (TRF-ST-004) and complete a hair test. f. The Provider should collect a sufficient quantity of hair (about 2 inches in length and 50 strand of hair cut about ¼ inch from the scalp). If the client has short hair more hairs will be need to meet the collection needs. g. The hair testing facility will complete a 5-panel hair toxicology screen (Cocaine, Methamphetamine, Opiates, PCP, Marijuana). Results will be reported within 2-6 business days. h. If there are positive results reported from the Standard Hair Test Screen, the Provider can call the testing facility (Psychmedics at 1-800-522-7424) to request a complete sectional analysis. It is important to clarify that you are calling about an ABH client and requesting the additional testing. Psychmedics will invoice. ABH directly for additional testing. Rev. 11/07 22 Referral and Authorization Process (CHART) Type of Service/Level Information Needed of Care From DCF Information Need from the Provider Information needed or provided by ABH Authorization Requirements Evaluation (up to 90 minutes) Results and recommendations forwarded to DCF within five (5) business days. Client Referral Form, which serves as the authorization for the evaluation. Basic demographic information and substance abuse information from the DCF worker. Telephonic call from DCF Random screens are included. An evaluation has been conducted within the last six (6) months. Outpatient (Individual, Group, Family/Couples) Release of Information from the client. Telephonic referral to ABH. Telephonic referral if treatment only referral or if there has been a 45 day lapse from the initial referral call IOP PHP Urine Drug Screen Telephonic referral Extended Drug Screens SAS authorization Hair Test SAS authorization, Court Order and/or Program Supervisor authorization Rev. 11/07 Client Reporting Form, TANF, and Needs Assessment for women. Verify client’s insurance, check for existing referral An OTR needs to be submitted before services rendered An OTR needs to be submitted before services rendered Random screens have to be done within six (6) weeks Utilization Review of OTR There has to be an evaluation that has been completed within the last six (6) months. An open referral must exist. OTR faxed to ABH directly. Utilization Review of OTR OTR faxed to ABH directly. Will authorize 12 units to be conducted within six (6) weeks. LabCorp invoice via fax for reimbursement See Hair testing procedure Reimbursement for pre-authorized test Telephonic referral by DCF worker needs to be called in prior to services Telephonic authorization Set up a referral upon telephonic referral Telephonic authorization 23 Reimbursement Protocol There are a variety of procedures that each party involved in ABH Project S.A.F.E. is required to follow. In the following section, we will outline what we (ABH) will do, and what DCF and/or the Provider are required to do, in order that client services are reimbursed. Rev. 11/07 24 Provider Credentialing Project S.A.F.E. services will be provided by agencies licensed by the Department of Public Health to provide outpatient substance abuse services and that have an agreement with ABH. Professionals within an agency who hold one of the following qualifications will be eligible to conduct evaluations: Certified Alcohol and Drug Counselor (CADC) Certified Alcohol Counselor (CAC) Licensed Alcohol and Drug Counselor (LADC) Masters or doctoral level clinician with at least two years of experience in the treatment of substance abuse Connecticut licensed Registered Nurse with at least two years of experience in the treatment of substance abuse Staff with backgrounds other than those listed above will be considered on a case-by-case basis and approved by the ABH Project S.A.F.E. Program Manager or designee. All non-certified or nonlicensed evaluators must be supervised by a licensed masters or doctoral level clinician. Reimbursement Project S.A.F.E. provides reimbursement for all authorized evaluations, outpatient treatment services, drug screens/hair tests, and court costs. ABH Project S.A.F.E. offers providers a web based electronic system to submit claims electronically; ABH Project S.A.F.E. encourages providers to make use of this system. ABH offers training twice annually on how to submit claims using the electronic system. ABH Project S.A.F.E. will make itself available to providers for assistance or individual trainings on an ad hoc basis. ABH Project S.A.F.E. is the payer of last resort and as such clients are expected to use their insurance plan when receiving Project S.A.F.E. services. Providers will be reimbursed the difference between what the insurance company pays, and the approved ABH reimbursement rate. Fee schedules are furnished to provider groups as part of the initial and annual contracting. Reimbursement Procedures: Evaluation Treatment IOP and PHP Drug Screens o Urine Screens o Extended Drug Screens o Hair Test Court Appearances Rev. 11/07 25 Reimbursement for Evaluation DCF Responsibilities Provider Responsibilities The DCF Social Worker will need to call ABH Project S.A.F.E. 1-800-2720097 to make an evaluation referral. The DCF Worker will need to provide the following information: Release of Information Client’s Insurance Information Client’s Social Security Number Results of DCF Substance Abuse Screen Basic Demographic Information It is important to remember that an evaluation referral includes a referral for treatment if the treatment services begin within 45-days of the date of the referral. **************************************************************** The Evaluation provider needs to be aware of any existing referrals. Appointments should be provided within the priority access guidelines, if the Provider is unable to do so, they should notify ABH Project S.A.F.E. The provider needs to contact the DCF Social Worker with verbal results of an evaluation within 24 hours, and with written results within 5 days. A referral will lapse if no service is provided within a forty-five (45) day limit. To determine if the Referral has lapsed, the Provider will look on the Client Referral Form [Appendix A] review the service(s) requested end date. The evaluation needs to be conducted before this date; if not the Provider should request that the DCF Social Worker call ABH Project S.A.F.E. to make a new referral. The Provider needs to complete the following information and submit to the ABH claims department: Client Report Form [Appendix B] For women only the Needs Assessment Form [Appendix C] TANF Eligibility Screening Form [Appendix D] The Provider must submit claims for reimbursement no more than 30 days following the date the service was provided. Claims submitted beyond this time frame will be denied reimbursement for “untimely filing”. If there is a correction required on any submitted claim, the Provider has 90 days from the service date to correct the claim. **************************************************************** ABH Project S.A.F.E. Will Rev. 11/07 ABH will fax the referral information to the Provider when a DCF Social Worker makes an evaluation referral. This referral information serves as the authorization. [Appendix A] ABH will maintain an electronic record of every referral, which will allow reimbursement for an evaluation provided. 26 Reimbursement for Treatment DCF Responsibilities Provider Responsibilities The DCF Social Worker will need to call ABH Project S.A.F.E. 1-800-272-0097 to make a treatment only referral. The DCF Social Worker will need to provide the following information: Release of Information Client’s Insurance Information Client’s Social Security Number Results of DCF Substance Abuse Screen Basic Demographic Information It is important to remember that if treatment begins within 45 days of the evaluation referral start date no treatment referral needs to be called in by the DCF worker. ******************************************************************* The Treatment provider needs to be aware of any existing referrals. If the treatment services begin within 45 days of the start date of the evaluation referral, the Provider can submit claims as described in the claims submission portion of this document. If a referral lapses because it is beyond the 45 day limit, the provider should contact the DCF Social Worker and request that he or she call in a new referral. The provider should communicate the course of client treatment by contacting the DCF Social Worker regularly. Providers who create a treatment plan which recommends IOP or PHP must complete an OTR (see following reimbursement section). The Provider must submit claims for reimbursement no more than 30 days following the date the service was provided. Claims submitted beyond this time frame will be denied reimbursement for “untimely filing”. Providers should verify the client’s insurance and indicate this information in the claims submission process. If a client does not have insurance a special exception can be granted. See Special Exception procedure (page 29). Treatment-only referrals can be made under the following circumstances: Treatment-only referrals following an acute care episode; Treatment-only referrals resulting from the need to transfer a client from one provider to another; Treatment-only referral following a lapsed forty-five (45) day referral. In every case it is required that an evaluation has been completed (within the previous six (6) months) prior to the DCF Social Worker making a treatment-only referral through contacting the Project S.A.F.E. Referral Hotline at ABH. ***************************************************************** Rev. 11/07 27 ABH Project S.A.F.E. Will Rev. 11/07 ABH Project S.A.F.E. will fax the referral information to the Provider when a DCF Social Worker makes the treatment referral. ABH Project S.A.F.E. will fax the Client Referral Form with Treatment Only indicated in the service(s) requested section. (Appendix B) ABH will maintain an electronic record of every referral, which will allow reimbursement for treatment. A separate referral for urine screens is not required under a treatment only referral. Chain of custody random urine screens will be reimbursed by ABH under the treatment only authorization called in by the DCF worker. 28 Reimbursement for IOP or PHP Levels of Care DCF Responsibilities Provider Responsibilities Ensure that all necessary information is available to both the treatment provider and ABH. ************************************************************ IOP and PHP levels of care are authorized based upon a process of Utilization Review (UR). To engage in this process the Provider must submit an Outpatient Treatment Request Form (OTR) [Appendix E]. The OTR form must be completely filled-out, with the necessary demographic and clinical information prior to admission to the IOP or PHP levels of care. An OTR form needs to be completed prior to the expiration or completion of services previously authorized. Any subsequent OTR forms should be completed with new clinical information and an updated treatment plan. The provider is required to respond promptly to any inquiries for supporting clinical information. Once a it has been determined that the client is no longer in need of IOP or PHP services a Discharge Notification Form [Appendix F] needs to be completed. ABH Project S.A.F.E. Will The Provider must submit claims for reimbursement no more than 30 days following the date the service was provided. Claims submitted beyond this time frame will be denied reimbursement for “untimely filing”. IOP and PHP services can also be denied if the client does not meet clinical criteria. ************************************************************* Help educate treatment providers about clinically appropriate treatment planning, and decision-making processes regarding level of care decisions as requested. Receive and process Outpatient Treatment Requests (OTR) for IOP and PHP levels of care through Utilization Review. In order to assure that the patients who require IOP and PHP levels of care, these services are authorized based upon a process of Utilization Review (UR). While no effort is being made to restrict access to these levels of care, the goal of UR ensuring that limited treatment funding provides treatment for those clients with clinically appropriate need. Provide a three-day turnaround time on authorization decisions, with access to urgent authorizations when clinically necessary. Provide an appropriate appeal process for all adverse determinations. (See Appeals Process page) Maintain a copy of the OTR for download at the following web address: https://www.abhct.com Rev. 11/07 29 Reimbursement for Hair Testing DCF Responsibilities Provider Responsibilities Hair test can be requested by the DCF Social Worker to determine if a client has abused a substance over the past 90 days. Hair testing is useful for obtaining historical use within a 90-day period. To request a hair test and receive reimbursement the DCF Social Worker will contact the Substance Abuse Specialist in their respective offices for approval. Once this approval has been granted DCF should contact ABH Project S.A.F.E. ************************************************************ The provider is required to collect a sufficient sample for a hair test in accordance with standards for hair testing as specified in the training. The provider then submits the sample, with a request for a standard screen to Psychemedics. If the results are positive the provider can request a multi-sectional testing of the positive result, by calling Psychemedics at their toll-free number and requesting a multi-sectional be completed. This multi-sectional does not require the client to return to the office and will not be reimbursed by ABH. Results should be discussed with the DCF Social Worker through telephone contact as soon as possible. ABH Project S.A.F.E. Will The Provider must submit claims for reimbursement no more than 30 days following the date the service was provided. Claims submitted beyond this time frame will be denied reimbursement for “untimely filing”. ************************************************************* ABH will serve as the coordinator of Hair testing requests, and as the conduit for information between Psychemedics and other parties involved. ABH will help expedite procedures whenever possible, and will provide a forum for annual training for any provider who is interested. ABH will ensure that Psychemedics is meeting the criteria for timely reporting of results, through a monitoring program. ABH will provide reimbursement to providers, which includes an administrative fee related to collection and submission of the sample to LabCorp, and the actual cost that LabCorp invoices the provider for completion of urinalysis. Rev. 11/07 30 Reimbursement for Random Urine Drug Screens Only DCF Responsibilities The DCF Social Worker will contact ABH with a request for random drug screens. Project S.A.F.E. allows a Provider to perform random urine drug screens for clients who are not engaged in treatment, but require monitoring. Random urine toxicology screens cannot be implemented in the absence of a completed evaluation in the past six months, or a court order, or a client being in active treatment. Provider Responsibilities Providers are required to follow the to chain of custody protocol for collecting and forwarding urine specimens. Providers are required to report to the DCF worker the results of all negative drug screens within forty-eight (48) hours and all positive drug screens within seventy-two (72) hours. Written results should be faxed to the DCF Social Worker upon receipt of the results. If there is a positive Opiate result, the DCF Social Worker can request an extended opiate search. (See below for instruction:) Extended Opiate Search has to be approved by the Substance Abuse Specialist in the respective DCF area office. Once this has been obtained DCF needs to call the ABH Billing Coordinator at 860-704-6144 with client name, ABH number, and verification of approval from the Substance Abuse Specialist. The Provider should then send in the Labcorp Invoice to ABH via mail 213 Court Street, Middletown, CT 06457 or fax to 860-6385302. (see detail in Reimbursement for Extended Opiate Search ) ABH Project S.A.F.E. will authorize 12 random drug screens over a sixweek period. The Provider at the end of this period shall notify the DCF Social Worker to call ABH Project S.A.F.E. for subsequent referrals for urine screens if applicable. The Provider must submit claims for reimbursement no more than 30 days following the date the service was provided. Claims submitted beyond this time frame will be denied reimbursement for “untimely filing”. ************************************************************* ABH Project S.A.F.E. Will Rev. 11/07 ABH will authorize a total of twelve (12) random drug screens over a sixweek period. ABH Project S.A.F.E. will receive referrals for this service via their toll-free Project S.A.F.E. intake line. 31 Reimbursement for Extended Drug Screens (extended opiate search) DCF Responsibilities Provider Responsibilities The DCF Social Worker will review the case with the Substance Abuse Specialist (SAS) in their Area Office. The SAS will contact the Project SAFE Billing Coordinator to authorize an extended drug screen. ************************************************************ Providers are required to follow the to chain of custody protocol for collecting and forwarding urine specimens. Providers are required to report to the DCF worker the results of all negative drug screens within forty-eight (48) hours and all positive drug screens within seventy-two (72) hours. Written results should be faxed to the DCF Social Worker upon receipt of the results. If there is a positive Opiate result, the DCF Social Worker can request an extended opiate search. (See below for instruction:) Extended Opiate Search has to be approved by the Substance Abuse Specialist in the respective DCF area office. Once this has been obtained DCF needs to call the ABH Billing Coordinator at 860-704-6144 with client name, ABH number, and verification of approval from the Substance Abuse Specialist. The Provider should then send in the LabCorp Invoice to ABH via mail 213 Court Street, Middletown, CT 06457 or fax to 860-6385302. (see detail in Reimbursement for Extended Opiate Search ) ABH Project S.A.F.E. will authorize 12 random drug screens over a sixweek period. The Provider at the end of this period shall notify the DCF Social Worker to call ABH Project S.A.F.E. for subsequent referrals for urine screens if applicable. The Provider must submit claims for reimbursement no more than 30 days following the date the service was provided. Claims submitted beyond this time frame will be denied reimbursement for “untimely filing”. ************************************************************* ABH Project S.A.F.E. Will Rev. 11/07 ABH will authorize a total of twelve (12) random drug screens over a sixweek period. ABH Project S.A.F.E. will receive referrals for this service via their toll-free Project S.A.F.E. intake line. 32 Requests for Court Cost Reimbursement DCF Responsibilities Provider Responsibilities Project S.A.F.E. providers on occasion are subpoenaed to testify in court regarding DCF cases. In order to support the benefit of such testimony, DCF has agreed to reimburse providers for their time as related to court testimony through Project S.A.F.E. ****************************************************************** When a provider receives a subpoena to give testimony in court on a Project S.A.F.E. case, the provider may request to be placed “on call” by contacting the Assistant Attorney General (AAG) at the telephone number listed on the subpoena. If the provider is unable to reach the AAG, the provider may contact the Attorney General’s Office in Hartford at 860-566-3696 and request to be placed “on call” for the specific case. If the provider goes to court on a Project S.A.F.E. case, the provider may bill ABH based on the time spent in the courtroom, whether or not the provider actually testified in the case. To be reimbursed, the provider will type a brief letter to the ABH Project S.A.F.E. Manager identifying the client by name and ABH number, the date of the court appearance, and the name of the clinician with the appropriate rate and final figure (please refer to the fee schedule). Whenever possible the letter should be co-signed by the Executive Director of the agency. **************************************************************** ABH Project S.A.F.E. Will Rev. 11/07 ABH will provide reimbursement to providers, for time spent in court. ABH will remit that reimbursement upon receipt of appropriate written documentation. 33 Special Exceptions ABH is the payer of last resort; the term ‘payer of last resort’ indicates that the Project S.A.F.E. funds are used to reimburse providers on a fee-for-service basis when there is no other source of reimbursement available. DCF and DMHAS recognize that there are circumstances under which a client may not be able to access services under their current payer source or under the structure or function of payer of last resort hence there may be exceptions granted. Exceptions are granted only for the circumstances indicated below: ABH provider does not participate in the client’s insurance plan and referring the client to another ABH provider is not an option. The client has no reliable transportation to the in-network provider and the client has to be referred to an out of network provider Client has insurance but does not want their employer to know they are in treatment Insurance company/entitlement does not provide the needed level of care After treatment has begun, client’s insurance plan changes Client may go from having no insurance to having insurance, with the provider being out-ofnetwork Out-of-network provider offers daycare/babysitting and/or transportation services The intention of granting special exceptions for the aforementioned circumstances is to ensure that services will not be disrupted. The special exceptions system was established to make concessions for special circumstances when appropriate and to track the frequency of such conditions. To obtain special exception the following steps need to followed: 1. A Special Exception Form [Appendix G] needs to be completed in its entirety. 2. The form should be complete on or before the date of service. ABH will only back date up to five business days. 3. The form is then faxed to ABH at 860-638-5302. All information must be provided for the exception to be granted and services reimbursed. Exceptions other than those listed here should be directed to the Project S.A.F.E. Program Manager or designee. Every effort will be made to address any and all unique circumstances in an efficient manner. Rev. 11/07 34 V. Claims Process There are a variety of procedures that each party involved in Project S.A.F.E. is required to follow. In the following section, we will outline steps to assist in claim submission. Rev. 11/07 35 Overview The claim submission process is the system in which ABH Project S.A.F.E. will reimburse network providers for services rendered to clients. ABH utilizes a web based claims submission system. For services to be reimbursed an authorization needs to exist in the ABH Project S.A.F.E. data system (please see referral and authorization section). Once a referral has been made by DCF, Providers must submit claims for reimbursement no more than 30 days following the date the service was provided. Claims submitted beyond this time frame will be denied reimbursement for “untimely filing”. In using the web based claims submission system the provider will need to have a password to access the system. Each agency will follow their internal procedure for claims submission. Providers who have submitted a claim electronically in the form of a response code “9”, or who have submitted a claim manually, have a maximum of 90 days from the service date to correct the claim. Should there be a compelling reason why the claims submission may be delayed, a call should be made in advance to the ABH Claims Coordinator (860-704-6144) to explain the reason (staff shortage, vacation schedules, etc.) In the web based claims system there will be six tabs: Six Tab Web Base Claim System Rev. 11/07 36 1. 2. 3. 4. Problem/Unpaid- denials To be paid –authorized payment has been approved payment to be issued by next closing New Claim – claim needs to be submitted Reports – tells who has been paid, denied or is pending payment for a given period of time. This is based on the ABH closing date 5. Change Login – change your log in information 6. Logoff – to exit the system To complete the electronic claims process the provider will need insurance information, TANF eligibility form and basic demographic information. All fields should be completed [See Appendix H] All dollar values will pre-populate in accordance with provider rates. Provider rates are updated each fiscal year. Claims may also be submitted manually. A form can be requested from the ABH Claims Coordinator at 860-704-6144. Rev. 11/07 37 Complaints, Grievances, and Appeals Rev. 11/07 38 Utilization Review Process Before authorizing any services for Project S.A.F.E. clients ABH Utilization Review staff must ascertain whether the client’s symptoms meet Service Necessity Criteria for the requested service. The Utilization Review staff may use the ABH Medical Director or his/her designee to assist in making that determination. In order to make a determination that the requested service(s) meet the Service Necessity Criteria, the service must meet all the following criteria: The service is appropriate for the symptoms, diagnosis and treatment of a particular disease or condition that is defined under the DSM IV-TR or its successor. The service is provided in accordance with generally accepted standards of mental health and/or substance abuse professional practice and bio-psycho-social approach to rehabilitation. The type, level, and length of treatment services are needed to provide safe, adequate and appropriate care, and are intended to improve the individual’s condition. Treatment geared toward simply maintaining the individual’s current level of functioning is appropriate only when, without such treatment, the individual would be likely to suffer a relapse or deterioration of health status. Service Necessity Criteria does not include “custodial care”. All clinical denials must be based on a review made by a Connecticut licensed clinical reviewer. If during the normal course of the review, a provider decides to withdraw the request for additional services, the case does not have to be subject to clinical review. If the Utilization Review staff determines that Service Necessity Criteria has not been met, the provider will be notified via certified mail of the decision. Appeals: There are two types of appeals that may be lodged regarding denial of service by ABH Project S.A.F.E.: clinical appeals and administrative appeals. Clinical appeals: A provider, his/her authorized representative or designee may appeal a decision to deny, reduce or terminate a behavioral health service. The appeals process is as follows: Upon receipt of the denial, an appeal may be initiated by providing additional justification of the need for service. This appeal must be submitted to ABH no later than seven calendar days after receipt of the denial decision. The Provider or his/her authorized representative will be sent notice of the decision on the appeal no later than four business hours after receipt of information required rendering a decision. If dissatisfied with the first level appeal decision, a second level appeal must be submitted to ABH no later than seven calendar days after the first level appeal denial. The Provider or his/her authorized representative will be sent notice of the decision on the second appeal no later than two business days after receipt by ABH Project S.A.F.E. of information required to render a decision. Rev. 11/07 39 If dissatisfied with the second level appeal decision, a third level appeal must be submitted directly to DMHAS no later than seven calendar days after the second level denial. A third level appeal will not be considered if the first or second level appeal is still being reviewed within the established time frames. Administrative Appeals: A provider may appeal a decision by ABH that is based on noncompliance with administrative procedures. The appeals process is as follows: Within seven (7) calendar days of the denial from ABH, the provider or his/her authorized representative may initiate the administrative appeals process by providing additional information or by demonstrating “good cause”. The provider will be sent notice of the decision within seven business days following receipt of the appeal by ABH. The notification will include the principal reason (s) for the decision and instructions for requesting a further appeal, if applicable. If dissatisfied with the first level decision, the provider or his/her authorized representative may submit a second level appeal directly to DMHAS no later than seven days after the denial of the first appeal. The appeal must be accompanied by information necessary and sufficient to render a decision. For first level appeals send correspondence to: Advanced Behavioral Health Project S.A.F.E. 213 Court Street Middletown, CT 06457 For second level appeals complaints or grievances, send correspondence to: DMHAS Department of Mental Health and Addiction Services Karen Orhenberger 410 Capital Ave., MS#14HCO P.O. Box 341431 Hartford, CT 06134. Complaints and Grievances: A Project S.A.F.E. client may utilize the Providers established grievance procedure to seek resolution of complaints and grievances concerning the quality or level of services provided. Grievances are defined as a complaint against a service provider in matters other than the denial, reduction or termination of services. Rev. 11/07 40 Appendices Rev. 11/07 41 Appendix A CLIENT REFERRAL FORM (page 1) Advanced Behavioral Health, Inc. Middlesex Corporate Center 213 Court Street, 10th Floor Middletown, Connecticut 06457 Social Worker Name . . . . City . . . . . Phone . . . . FAX . . . . . . Unit . . . . . Supervisor Date: Time: Page: Provider Name . . Phone . . Address City . . . Contact . Region . Client Information ABH ID #. . Name . . . . Address . . . City . . . . . . Insurance Payor . . . . Health Plan Gender . . Race . . . . Soc Sec # . Language Link # . . . . Date of Phone . . . . Substance Abuse Treatment Code . Suspected Substance(s) Use: Reason(s) for Suspecting: Service(s) Requested: # Units Begin Date End Date Reason for referral Rev. 11/07 42 CLIENT REFERRAL FORM (page 2) Advanced Behavioral Health, Inc. Middlesex Corporate Center 213 Court Street, 10th Floor Middletown, Connecticut 06457 Date: Time: Page: Client ID . . Name . . . . Substance Abuse Screening / Information Form 1. Client appeared to be under the influence of drugs and/or alcohol. 2. Client showed physical symptoms of trembling, sweating, stomach cramps, nervousness. 3. Drug paraphernalia was present in the home, i.e., pipes, charred spoons, foils, blunts, etc. 4. Evidence of alcohol was present in the home, i.e., excessive number of visible bottles/cans whether empty or not. 5. There was a report of a positive drug screen at birth list drugs Mother Child 6. There was an allegation of substance abuse in CPS Report. 7. The child(ren) reports substance abuse in the home. 8. The client has been in substance abuse treatment. 9. The client has used the following in the last twelve Marijuana/Hashis Heroin/Opiates Cocaine/Crack Other Drugs 10. Client shared that s/he has experienced negative consequences from the misuse of alcohol, i.e., DWI/DUI Domestic Fights Job Loss Arrests Other: 11. Client shared s/he has experienced trouble with the law due to the use of alcohol or other drugs, i.e., DWI/DUI Domestic Violence Drug Possession Other: 12. There are adults who may be using drugs and/or misusing alcohol who have regular contact with the client's child(ren). 13. The client acknowledged medical complications due to the use of substances. 14. Other Comments Rev. 11/07 43 Appendix B CLIENT REPORT FORM ABH Contact: Referral Date/Time: Ref #: ADVANCED BEHAVIORAL HEALTH, INC. Middlesex Corporate Center, 10th Floor, Middletown, CT 06457 Phone: 860.638.5309 Fax: 860.704.6179 PROJECT SAFE DCF Substance Abuse Services for Primary Care Givers To:____________________________ and __________________________________ DCF SOCIAL WORKER ABH INTAKE WORKER DATE:____________ CLIENT NAME:_____________________________________ ABH CLIENT ID #______________ The above client received: (Check all that apply) DRUG SCREEN:____________ EVALUATION:______________ TREATMENT RECOMMENDED: CHECK ONE START DATE FOR BELOW TX:_____________ _____ NO TREATMENT RECOMMENDED _____ INDIVIDUAL THERAPY _____ GROUP THERAPY _____ FAMILY/COUPLE THERAPY _____ INTENSIVE OUTPATIENT _____ PHP _____ EARLY INTERVENTION _____ METHADONE (Not funded by DCF contract) _____ INPATIENT DETOX (Not funded by DCF contract) _____ AMBULATORY DETOX (Not funded by DCF contract) _____ RESIDENTIAL SERVICES (Check below; not funded by DCF Contract) With Children________ Without Children________ Clinician Name: _________________________________________ Date:___________ (Please Print/Required field) SIGNATURE_____________________________________________ Name of Provider Rev. 11/07 __________________________________ 44 Appendix C Needs Assessment Form ADVANCED BEHAVIORAL HEALTH, INC. Residential Services for Substance Abusing Women and Their Children Client Name: ABH #: Date of Evaluation: Evaluator: Provider: _____Yes _____No Is this client clinically most appropriate for residential treatment? (If No, Stop Here, if Yes Continue.) Please complete the following on all clients for whom residential is assessed as the most clinically appropriate level of care. (Regardless of whether a referral for that level of care is actually made.) _____Yes _____No Client accepted recommendation for residential treatment. If No, why not? (childcare, work, etc.) ___________________ _____Yes _____No Bed was available. Name of Residential Program__________________________ If not admitted to residential treatment, did client accept referral to alternative level of care? _____Yes _____No If Yes, specify level of care_____________________________________ DCF-Needs Assessment Form March 2003 Rev. 11/07 45 Appendix D TANF ELIGIBILITY SCREENING FORM Client Name: ABH ID #: 1: Does the case involve a foster parent or a parent with a Write Yes or No child that has been removed from the home? If the answer to question 1 is yes, you do not need to answer questions 2, 3 and 4. The family is automatically TANF eligible and the worker would need to select the code 01 (TANF eligible) in the appropriate section of the ABH-DCF Weekly Activity Report (i.e. the claims forms). If the answer is no, proceed to 2. 2: Is the client a parent or caretaker relative with a minor Write Yes or No child living in the home? If the answer to question 2 is no, you do not need to answer questions 3 or 4. The client is not TANF eligible and the worker would need to select code 02 (not TANF eligible) in the appropriate section of the ABH-DCF Weekly Activity report. If the answer is yes, proceed to 3. 3: Is the client currently eligible for Medicaid, HUSKY, Write Yes or No Food Stamps, TFA cash assistance or child care assistance? If the answer to question 3 is yes, you do not need to answer question 4. The client is automatically TANF eligible and the worker should select code 01 (TANF eligible) in the appropriate section of the ABH-DCF Weekly Activity Report. If the answer is no, or the worker is unable to determine if the client receives any of these benefits, then the worker should proceed with question 4. 4: Number of parents, 75% of 75% of Is family income below the Children, and relatives State State 75% SMI for that family’s living in the home Median Median size? Write Yes, No, or Income Income Unable to Determine (Annual) (Monthly) 2 $38,522 $3,211 3 $47,586 $3,966 4 $56,651 $4,721 5 $65,715 $5,477 6 $74,779 $6,232 7 $76,478 $6,374 8 $78,178 $6,515 9 $79,877 $6,657 10 and above $81,577 $6,799 If the answer to the question is yes, then the worker should select code 01 (TANF eligible) in the appropriate section of the ABH-DCF Weekly Activity Report. If the answer is no, then the worker should select code 02 (not TANF eligible). If the answer is unable to determine, then the worker should select code 03 (unable to determine). TANF Eligibility Status (please circle the appropriate answer): Yes No Unable to Determine Date:_______________________________ProviderName:_______________________________ Rev. 11/07 46 Appendix E: Outpatient Treatment Request Downloading Procedure Procedure for Downloading OTR Form Once you access the ABH website you will see this screen. Move the cursor to Resources tab. A drop down list will appear. Move the cursor to ABH Downloads Rev. 11/07 47 Outpatient Treatment Request Downloading Procedure (page 2) Double Click ABH Downloads, this will the following screen. Rev. 11/07 48 Outpatient Treatment Request Downloading Procedure (page 3) Move the cursor to ABH Project SAFE Highlight Project SAFE Outpatient Treatment Request Form Double click This should open the form. It is recommended that you Save As and rename the document to a folder on your computer. Rev. 11/07 49 Appendix F: Discharge Notification Form Form Completed By: Telephone #:____________________ Date: Project SAFE Discharge Notification Form* Provider Name: Provider Service Location: Admission Date: Discharge Date: (2) Client Name: Client ABH ID#: Client’s Date of Birth: DIAGNOSIS – AXIS I: (1) DISCHARGE TYPE Regular (Completed Treatment) Refused Care (Refused Treatment Referrals) AMA (Against Medical or Clinical No Care (No Discharge Referrals/Plan Made) Advice) Transfer (transfer to higher level of care, or same level of care at a different location) Noncompliance (Did not follow treatment recommendations) Administrative (Violation of program rules) AWOL (Left inpatient level of care without permission/staff knowledge) Other (Please describe): Did the client complete treatment? DISCHARGE PLAN Provider Name: Service/Level of Care: Date of 1st Appointment: Discharge Medications: Yes No Number of Sessions Attended (if known) _________________ If there was no Plan, please explain : Living Arrangements at Discharge Homeless DCF Involvement: Yes Dependent Living (Residential, Halfway house, Supportive Housing, Shelter) Independent No (if yes please complete the questions below): DCF Case Status: Closed case DCF Notified of Discharge Plan Active Case No (If yes, the date of notification, _______/_________/________) mm dd yyyy Name of DCF Worker: _______________________________________________________________________ Form Completed By: Yes Telephone #:____________________ Date: *Discharge Notifications may be submitted by fax to: Advanced Behavioral Health, Inc. at (860) 638-5302 Project SAFE requires Discharge Notification for all authorized PHP or IOP services. Rev. 11/07 50 Appendix G Special Exception ABH Project SAFE Special Exception (formerly Regional Administrator’s Approval) Date of Request: Provider Name: Person Requesting Exception: Client Name: Client ABH#: Client DOB: Client SSN: - - Client’s Insurance Provider: Reason for Exception: Provider does not participate in client’s insurance plan Insurance out of Network Client refuses to use insurance Insurance change to out of network In-network service does not have childcare Services not covered by client’s insurance plan No transportation to in-network provider Type of Treatment Requested: Individual # of sessions: Anticipated Start date: Anticipated End date: Group # of sessions: Anticipated Start date: Anticipated End date: Family # of sessions: Anticipated Start date: Anticipated End date: Random Urine Drug Screen # of sessions: Anticipated Start date: Anticipated End date: Clinician Signature: Rev. 11/07 51 FAQ for Project SAFE Special Exceptions (Formerly Regional Administrator’s Approval) 1. What is a special exception? The special exception was formerly known as the Regional Administrator’s Approval. It is a means which providers who are unable to access client’s insurance can be reimbursed for services. Special exceptions are granted under the following circumstances: Services rendered are not covered by the client’s insurance The Provider is out of the client’s insurance network The client refuses to use his/her insurance The in network provider does not have childcare or transportation available to the client. No special exception needs to be completed for evaluation services. This only applies to outpatient services including group, individual, family and urine drug screens. 2. When should I fill out a special exception? A special exception form should be completed after insurance has been verified and the client meets the above criteria. Project SAFE is the payer of last resort; as such the Provider is expected to bill the client’s primary insurance first. If the client refuses to use his/ her insurance this would then require a special exception for continued treatment of group, individual and/or family. No special exception is needed for the evaluation service. A special exception form should be completed prior to the service start date or the first date of service. Special exceptions submitted more than five calendar days after the date of service will be denied for untimely submission. 3. Who needs to complete the special exception? The special exception form can be completed by any staff at your agency familiar with the client this includes administrative assistants, case managers, clinicians or billing staff. All the information needs to be included (client name, ABH#, client DOB, Type of treatment, number of sessions being requested, start and end dates of treatment). 4. What services can be requested with the special exception? Only outpatient services can be requested by special exception. These include: group, individual, family and urine drug screen. If you are requesting group, individual or family urine drug screens are included in this treatment modality. Urine drug screens can be requested but need a prior authorization from the DCF worker. 5. If a client comes in for an evaluation and has a previous evaluation at another facility within the past year will ABH reimburse for the Project SAFE evaluation if the client’s insurance will not? Project SAFE will cover the substance abuse evaluation if the client’s insurance will not cover the service. A claim should be submitted for the evaluation with a note indicating that the client’s insurance will not cover Rev. 11/07 52 services. This does not require a special exception and should follow the traditional claims process for evaluations. 6. If there is a denial from SAGA for outpatient services, will Project SAFE reimburse under a special exception? Yes, Project SAFE would reimburse under a special exception. This would be viewed, as the client’s insurance not covering services. This however only applies to outpatient services including individual, group and family. 7. If a client is on spend down and does not have the money to cover services, will Project SAFE reimburse for services rendered? Spend down is based on the State Medical Assistance program (Medicaid) operated by DSS. There are certain qualifications that an individual must meet to be eligible for Medicaid. Spend down is used when a person is not eligible based on excess income. In some cases a person can qualify if there income is over limit. This process is spend down and lets the person reduce the excess income to bring them within eligibility for Medicaid. The provider should verify that the client is on SAGA, but indicate on the Special Exception form that the client refuses to use insurance due to spend down. 8. If a client on private commercial insurance reports that they cannot afford their co-pay will Project SAFE reimburse the provider? There is a precedent in place regarding reimburse of any co-pay. DCF and DMHAS feel that paying a Medicaid co-pay goes against the spirit of Medicaid regulation likewise with commercial co pay reimbursement of a client’s copy would subverts the payer’s co- pay policy. 9. If the client is in IOP or PHP, but is also receiving other treatment i.e. domestic violence, anger management, and the insurance is paying for IOP or PHP and will not cover the other treatment will Project SAFE reimburse for the other treatment service? Project SAFE will reimburse for treatment not covered by the insurance, if the client has been provided an Project SAFE evaluation and authorization for services have been called in by the DCF worker or treatment begins with 45 days of the initial referral. 10. If the clinician providing the clinical services is not credentialed with the client’s insurance company, but the Provider agency is in the network will Project SAFE reimburse under a special exception? Yes, this is listed as one of the reasons for special exception and will be reimbursed by Project SAFE. Rev. 11/07 53 Appendix H: Screen Shot of Web-Based Claims System User Name : Trainning, ABH Service Date: 12/28/2005 ABH ID: 42578 Service Type: Evaluation Client Name, DOB, and/or Social Security Number was corrected. Please change applicable ABH Referral information First Name: SSN: Payor: Health Plan: None TANF: ABH Amount: $ Expected Amount: $ Balance Due: $ Note/Message: Client Refused to disclose insurance information Payor source information corrected - Verification of benefits performed Client Report Form (complete only on Evaluation Claims) Evaluator Name: Treatment Recommendations (check all that apply) No Treatment Recommended Services Funded by DCF Individual Therapy Methadone Maintenance Group Therapy Family/Couple Therapy Intensive Outpatient Early Intervention/Group Day/Evening Treatment/PHP Services NOT Funded by DCF Rev. 11/07 54 Residential Services with Children Inpatient Substance Abuse Residential Services without Children Psychiatric Services Residential Services - Unspecified Submit General Help: Support@ABHCT.com Web-Based Claims System Help: EbillingSupport@ABHCT.com ©Copyright Advanced Behavioral Health, Inc. Rev. 11/07 55