Nuclear refractive index as a novel molecular marker for cancer
advertisement

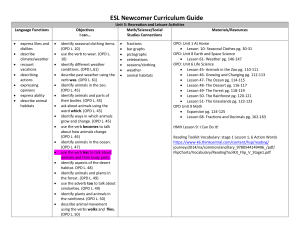
Article Title: Nuclear nano-morphology markers of histologically normal cells detect the “field effect” of breast cancer Journal: Breast Cancer Research and Treatment Authors: Rajan K. Bista*, Pin Wang*, Rohit Bhargava†, Shikhar Uttam*, Douglas J. Hartman‡, Randall E. Brand*, and Yang Liu*,§ * Department of Medicine, Division of Gastroenterology, Hepatology and Nutrition, University of Pittsburgh, Pittsburgh, PA 15232, USA † Department of Pathology, Magee-Womens Hospital, University of Pittsburgh Medical Center, Pittsburgh, PA 15213, USA ‡ Department of Pathology, University of Pittsburgh School of Medicine, Pittsburgh, PA 15232, USA § Department of Bioengineering, University of Pittsburgh, Pittsburgh, PA 15219, USA Corresponding author: Yang Liu, Ph.D. Email: liuy@pitt.edu SUPPLEMENTARY METHODS S1. Correction of stain variations To account for the effect of variation in the stain-induced optical pathlength difference, we have developed a correction model [1] based on the following equation: OPDc ( x, y) OPD( x, y) OPDc , where OPDc is the corrected optical pathlength difference (OPD), OPD is the measured OPD value before the correction, and OPDc is the stain-induced OPD value. This correction model follows directly from the linear relation between optical path length and change in cell dry mass concentration [2]. The detailed description and validation of this model have been reported in our paper [1]. In brief, a technician in a clinical pathology laboratory at University of Pittsburgh Medical Center (UPMC) prepared a calibration sample set using normal tissue with a 1 series of standard histology slides with different amounts of H&E stain, representing the range of variation that could be encountered in routine clinical specimens. We then measured the absorbance (A) of each histology slide through the transmission-mode optics and established a relationship between the various A and OPDc , which shows a linear dependence with a slope of ( OPDc A , where is the modified specific refraction increment [3,2]) and used as a constant calibration factor (Fig. S1). Fig. S1 The effect of variation in the stain-induced nuclear optical pathlength difference (OPD). The measured OPD as a function of the absorbance before and after applying correction model in the validation set of histology specimens. The solid lines represent the linear regression fits. After the calibration factor is determined from the calibration sample set, for any given histology slide, we perform both the reflectance measurement to obtain OPD values and the transmission measurement to obtain absorbance A, and the corrected OPD is obtained through relation OPDc ( x, y) OPD( x, y) A . As shown in Fig. S1, before 2 correction, the OPD shows a strong dependence on the different stain levels and the variation in OPD (quantified by the standard deviation of OPD ) is 2.6 nm. After applying the correction model, the OPD remains nearly constant for varying stain levels for the same sample set, as suggested by a clearly flat line in Fig. S1, and the variation in OPD is 0.89 nm, which is within the system sensitivity level of 0.9 nm. Therefore, the OPD after applying the correction model is nearly unaffected by staining levels. S2. Variation due to the thickness of tissue section Although the tissue section thickness can be controlled by a microtome, sub-micron scale variation is inevitable. Therefore, we investigated the effect of variation in section thickness on the measured OPD . We first prepared histology slides sectioned at 4 µm setting with 3 different microtomes (10 slides from each microtome) in the clinical pathology laboratory at UPMC that are routinely used for clinical specimen processing. This setting represents a real clinical scenario that the tissue sectioning was often performed with different microtomes which have variations in tissue section thickness. As shown in Fig. S2(a), we found that our method to extract OPD is not sensitive to variation in the tissue section thickness from different microtomes (no statistical difference, P = 0.7) and that the OPD from histology slides prepared with 3 different microtomes had a maximal variation of 0.5 nm, within the system sensitivity. Hence, we confirm that the variation in the tissue section thickness among different microtomes does not make a significant contribution to our results. 3 Second, we prepared histology slides using different settings of tissue section thickness (4 µm and 5 µm) on the same microtome. As shown in Fig. S2(b), the extracted OPD is independent of tissue section’s thickness (no statistical difference, P = 0.8), with a difference of 0.3 nm between 4 µm and 5 µm, also within the system sensitivity. This result also justifies that the measured OPD is due to the changes in internal structural properties of the cell nucleus, rather than the sample thickness difference. Fig. S2 Statistical analysis to investigate the effect of the variations in tissue sectioning thickness: (a) for three different microtomes with the same setting of section thickness at 4µm (ANOVA test, two-sided P-value = 0.67); (b) for different settings of section thickness at 4µm and 5µm, respectively (student t-test, two-sided P-value = 0.8). Error bar represents the standard error. Here we provide a preliminary theoretical interpretation why our method to extract OPD is minimally affected by the thickness variation. In clinical histology specimens, there is no strong reflection interface due to the closely matched refractive index between the mounting medium and the sample. We obtain the optical path length (OPL) profile based on spectral signals from the interfaces and scatterers within the 4 sample. In our method, we select a constant point (the same OPL value of interest for all samples) on the OPL profile plot, where the phase-related information is derived. This selected OPL value of interest must be within the sample, and the light beam should pass through most of the cell nucleus to capture the required phase information. By selecting the same OPL value of interest on OPL profile for each sample, we exclude sample thickness variation from our measurements and produces reliable results in which only phase variations due to internal structure occur. S3. Quantification of stain absorbance To confirm the result that the nano-morphology markers detect the “field effect” in breast carcinogenesis that is not due to the artifact of staining variations in cell nuclei, we quantified the absorbance from the cell nuclei. Specifically, we measured the light intensity in the transmission configuration from the background ( I 0 ) and from the same cell nuclei ( I nu ) as we used for nano-morphology marker analysis, from patients with normal cells (Cat 1), ‘malignant-adjacent’ normal cells (Cat 5) and malignant cells (Cat 6). We calculated the absorbance based on the standard Beer’s law: A log10 ( I 0 / I nu ) for each cell nucleus, and obtained the characteristic value of average absorbance for an individual patient by taking the average value of 40-60 cell nuclei from each patient. As shown in Fig. S3, the absorbance does not show any similar correlation to our nanomorphology markers (as shown in Fig. 2 in the manuscript). Evidently, the stain absorbance from the cell nuclei cannot distinguish normal and “malignant-adjacent” normal groups (P = 0.58), but distinguish “malignant-adjacent” normal from malignant groups (P = 4.1E-6). While the statistical analysis shows that the nano-morphology 5 markers from ‘malignant-adjacent’ normal cells (Cat 5) are distinct from normal tissue from healthy patients (Cat 1), with a great similarity to malignant cells (Cat 6) (P < 0.001 between Cat 1 and Cat 5, and P > 0.05 between Cat 5 and Cat 6). Hence, we confirmed that the “field-effect” detected by the nano-morphology markers is not due to the artifact of staining variations. 1.4 P = 0.0006 Absorbance 1.2 P = 0.58 P = 4.1E-6 1.0 0.8 0.6 0.4 Normal 'Malignantadjacent' normal Malignant Fig. S3: Statistical analysis of the stain absorbance from the cell nuclei in patients with normal cells (Cat 1), ‘malignant-adjacent’ normal cells (Cat 5) and malignant cells (Cat 5). The statistical comparison between two patient groups was obtained using Wilcoxon’s rank-sum test at 95% confidence interval, and two-sided P-values were used. The error bar represents the standard error. REFERENCES 1. Uttam S, Bista RK, Hartman DJ, Brand RE, Liu Y (2011) Correction of stain variations in nuclear refractive index of clinical histology specimens. J Biomed Opt 16 (11):116013. doi:10.1117/1.3650306 6 2. Barer R (1957) Refractometry and interferometry of living cells. J Opt Soc Am 47 (6):545-556 3. Barer R (1952) Interference microscopy and mass determination. Nature 169:366-367 7