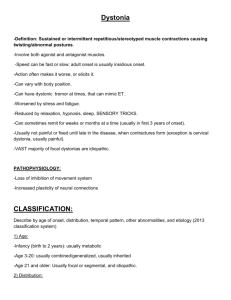
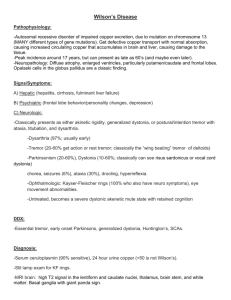
Overview of Dystonia
advertisement

Overview of Dystonia Dystonia is a neurologic movement disorder characterized by sustained muscle contractions, usually producing twisting and repetitive movements or abnormal postures or positions. Almost all dystonic movements share a directional quality that is typically sustained, sometimes for an instant, as well as a consistency and predictability Dystonia movements are directional, forcing the involved body part or region into an abnormal position, which is consistently present. Classification of Dystonia Dystonia is classified in a number of ways including... Age at which symptoms appear. Symptoms may become apparent during childhood, adolescence, or adulthood. Area or areas of the body that are affected. Sustained muscle contractions and abnormal movement patterns may be limited to one area of the body; involve two or more areas of the body that are next to each other, as in segmental dystonia or two or more areas of the body that are not next to each other (non-segmental or multi-focal); or be generalized in nature, including leg involvement and other areas of the body. Cause. Dystonia may occur as a primary condition (idiopathic dystonia) that is familial or occurs in the absence of a family history. It may result from certain environmental factors or "insults" that affect the brain (secondary or symptomatic dystonia). Dystonia may be associated with certain nondegenerative, neurochemical disorders (known as "dystonia-plus syndromes") that are characterized by neurologic features, such as parkinsonism or myoclonus. Dystonia is also a primary feature of certain, usually hereditary, neurodegenerative disorders (so-called "heredodegenerative dystonias"). Dystonia and its Relationship to Activity Dystonic movements or posturing are often described as they relate to activity or factors that may aggravate symptoms. Dystonia, particularly primary dystonia, of a body part may... Occur only during voluntary movement or become worse during these movements. This is known as action dystonia. Dystonia that appears only with specific actions, such as writing (i.e., "writer's cramp"), is a task-specific dystonia. Primary dystonias often begin as task-specific yet eventually appear with other activities as the condition progresses. For example, dystonic cramping and spasms that initially appear only when writing may eventually occur during other activities, such as eating. Occur with voluntary movements of other, unaffected bodily regions. This phenomenon, known as "overflow," may develop as a dystonic condition progresses. Occur even when the affected body part is at rest. This is referred to as rest dystonia. Rest dystonia may develop with further progression of a dystonic condition and therefore is typically considered more severe than action dystonia. Lead to sustained, abnormal, fixed postures or positions of affected body regions, potentially causing permanent contractures. Dystonic contractions are relatively slow or rapid in speed, sometimes resembling other neurologic movement disorders, such as the "shock-like" muscle contractions seen in myoclonus or the irregular, relatively brief movements of chorea. Dystonic movements are more closely associated with prolonged bursts of electrical activity in affected muscle(s) rather than the short, irregular bursts of myoclonus. In addition, dystonic movements tend to have a sustained, directional nature rather than the random, flowing contractions seen with chorea. Dystonia also typically may be distinguished from the involuntary, rhythmic, "back-and-forth" movement characteristic of tremor. In some dystonic patients, tremor-like muscle spasms or tremulous movements or dystonic tremor may be present upon attempting to actively resist abnormal, involuntary movements. Dystonic spasms typically increase in intensity during stress, emotional upset, or fatigue. Spasms tend to decrease in intensity during periods of rest or sleep. Many patients temporarily suppress dystonic movements or spasms by "sensory tricks." These tricks usually consist of touching the affected or adjacent body parts. Also known as gestes antagonistes, these sensory tricks are a phenomenon almost unique to dystonia; therefore, they may play a helpful role in differential diagnosis. Examples of commonly described sensory tricks include... Placing a hand on the side of the face, the chin, or the back of the head or touching these areas with one or more fingers may sometimes reduce neck contractions associated with cervical dystonia. Also known as spasmodic torticollis, cervical dystonia is characterized by abnormal movements or postures of the neck and head. Applying pressure on the eyebrows or touching skin to the side of the eyes may improve involuntary contractions of eyelid muscles or blepharospasm. Touching the chin or the lips, applying pressure beneath the chin, or placing an object in the mouth, such as a toothpick, may reduce dystonia of the jaw, mouth, and lower face (oromandibular dystonia). Touching the affected hand with the other hand may help to alleviate writer's cramp. Leaning against the wall while standing, pressing on the hips, or applying pressure to the back of the neck may help to alleviate dystonia of the trunk (truncal dystonia). Classification of Dystonia Dystonia is classified in various ways. The most current, widely accepted classification consists of three major categories: Bodily site(s) of involvement (anatomical distribution) Age at symptom onset Cause (etiology) or origin Anatomical Distribution Dystonia usually begins in a single body part. It may either remain restricted to that area or spread to involve another region or regions. Therefore, it is helpful to classify dystonia based upon anatomical distribution as follows: Focal—limited to one area of the body Segmental—affecting 2 or more nearby or contiguous areas of the body Multifocal—involving 2 or more distant regions of the body Hemidystonia—affecting one half of the body Generalized—leg involvement plus eventual involvement of another region or regions of the body Focal Dystonias There are several forms of focal dystonia as well as other dystonias that may be limited to one area of the body. Focal dystonias often become apparent during the fourth or fifth decade, so called adult onset. However, symptoms may become obvious earlier in life. Overall, women are affected approximately 3 times more frequently than men. The symptoms associated with the focal dystonias are variable and depend upon the intensity and severity of the spasms and the specific body region and muscle groups involved. The rate of progression from symptom onset to difficulties in activities of daily living and disability are extremely variable, ranging from rapid development over days or weeks to a gradual progression over a decade or more. Symptoms of focal dystonias may initially be periodic, occurring only during stressful periods or randomly. At first, symptoms tend to appear when the affected body part performs certain movements; they typically disappear when the affected area is at rest. However, as the disease progresses, dystonic spasms begin to develop with other activities of the affected region. Symptoms may occur with voluntary actions involving other bodily areas. This phenomenon is known as overflow. Eventually, dystonia may be present when the affected part is at rest. Gradually, the affected area may assume an unusual and sometimes painful posture. In up to 30 percent of patients, focal dystonias may extend to involve nearby areas, resulting in segmental dystonia. Less commonly, symptoms may begin to affect certain non-adjacent regions (multifocal dystonia). Focal dystonias often stabilize within a few years and may gradually slightly improve. In addition, some patients may experience a temporary diminishing or complete remission of symptoms for days or months, usually within 2 to 3 years following disease onset. Evidence suggests that remissions most frequently occur in patients with cervical dystonia, as compared with other focal dystonias. Focal dystonias are usually considered primary (idiopathic) dystonias, meaning that dystonia is the only sign, with the possible exception of tremor, and secondary causes are excluded. Adult-onset focal dystonias usually occur sporadically, in the absence of a family history. However, in some relatively rare cases, more than one family member may be affected. (For further information, see the section entitled "Etiology/ Primary Dystonia") Commonly described forms of focal dystonia include... Cervical dystonia (spasmodic torticollis) Blepharospasm Oromandibular dystonia Laryngeal dystonia (spasmodic dysphonia) Limb dystonia Cervical Dystonia (CD) Cervical dystonia (CD) is a focal dystonia. It is also known as spasmodic torticollis and is characterized by abnormal movements or postures of the neck and head. It is considered the most common form of focal dystonia. Although CD may become apparent at any age, symptoms usually begin between the ages 20 to 60 years. Women are affected approximately twice as commonly as men. The dystonic spasms of CD affect any combination of neck (cervical) muscles, resulting in jerky head movements or periodic or sustained unnatural position of the head . There is also sideways or lateral rotation of the head and twisting or torticollis of the neck, often with head tilt. There may be isolated turning, flexing, or extending of the neck to the side (laterocollis), front (anterocollis), or back (retrocollis). One shoulder may be elevated and displaced forward on the side toward which the chin turns. In addition, there is often mild associated dystonia in the upper arm muscles on the same side (segmental dystonia). Symptoms of CD often worsen while walking or during stress. Symptoms typically improve with rest or sleep. In addition, CD is the most common focal dystonia that responds to sensory tricks. For example, patients with CD may place their hand on the side of their face, chin, or the back of the head. This may reduce the intensity of dystonic spasms. Lightly touching or applying pressure to certain areas of the head on the side that is opposite to that which the head is turned may temporarily allow correction of abnormal head position. The reason why sensory tricks work for some patients is not fully understood. Over two-thirds of patients, particularly those with sustained head deviation, have associated neck pain. About one-third also experience head tremor (i.e., dystonic tremor), hand tremor, or both. Approximately 20 percent of patients with CD also have dystonic spasms of the eyelids (blepharospasm) or other muscles or of muscle groups of the arm or hand. Evidence suggests that about 10 percent of those with cervical dystonia may have brief, spontaneous remissions. An additional 10 percent, particularly patients with an earlier age at symptom onset, may have longer remissions of about 2 to 3 years, typically beginning during the first few years following disease onset. Blepharospasm This form of focal dystonia also affects women more frequently than men, with symptoms typically becoming apparent after age 50. The term blepharospasm refers to intermittent or sustained closure of the eyelids due to abnormal, involuntary contractions or spasms of certain muscles that function to close the eyelids. Some individuals with blepharospasm experience relatively mild spasms of the muscle underlying the skin of the eyebrows and the root of the nose as well as of the middle and lower facial muscles. These spasms may resulting grimacing or facial distortions. The condition is sometimes called essential blepharospasm or dystonic blepharospasm. In some patients, blepharospasm may begin in just one eye (unilateral). Initial signs of the condition include eye irritation and burning, an increased sensitivity to light (photophobia), and excessive blinking. With disease progression, patients may experience narrowing of the opening of the eyelids due to dystonia muscle contractions; involuntary, potentially forceful closure of the eyelids; and an inability to voluntarily raise the eyelids in order to open their eyes. Excessive blinking and involuntary eyelid closure may be temporarily relieved by certain sensory tricks, including singing, humming, or talking; laughing; yawning; opening the mouth; chewing; or applying pressure on the eyebrows, temple, or skin next to the eyes. These dystonic spasms generally disappear with sleep. In contrast, symptoms may worsen with stress, walking, reading, exposure to bright light, looking upward, watching television, or driving. Accordingly, blepharospasm may cause varying levels of difficulty with daily tasks, including reading and driving. Without treatment, blepharospasm often results in functional blindness, although vision may be normal. In some patients with blepharospasm, dystonic spasms may extend to nearby cranial areas, such as muscles of the tongue, mouth, jaw, neck, vocal cords, or other areas, thus becoming a segmental dystonia. (Also see description below of Meige syndrome, which involves blepharospasm with lower facial involvement.) Oromandibular Dystonia Oromandibular dystonia (OMD) may be characterized by dystonic spasms affecting the jaw, mouth, and lower face. The tongue may be involved as in lingual dystonia. In some cases, this may be the most prominent sign of OMD. In patients with OMD, involuntary contractions may involve the muscles used for chewing (masticatory muscles). These may include the thick muscle in the cheek that closes the jaw (buccinator muscles) and the broad muscle that draws back the lower jaw and closes the mouth (temporalis muscle). Some patients may also experience involuntary contractions of the wide muscle at the side of the neck that close the jaws. This muscle draws down the corner of the mouth and lower lip (platysmal muscles) or other muscle groups. Associated findings of OMD may include spasms of jaw closure with difficulty opening the mouth (trismus) and clenching or grinding of the teeth (bruxism); spasms of jaw opening; or sideways deviation or protrusion of the jaw. Additional symptoms may also be present, such as lip tightening and pursing; drawing back (retraction) of the corners of the mouth; or deviation or protrusion of the tongue. Due to such findings, OMD may cause jaw pain as well as difficulties eating and speaking (dysarthria). In addition, in some patients, the dystonic spasms may sometimes be provoked by certain activities, such as talking, chewing, or biting. As discussed earlier, particular activities or sensory tricks may sometimes temporarily alleviate OMD symptoms, including chewing gum, talking, placing a toothpick in the mouth, lightly touching the lips or chin, or applying pressure beneath the chin. Dystonic spasms may extend to involve nearby areas including the muscles of the eyelids, nose, neck, or vocal cords. Laryngeal Dystonia Spasmodic dysphonia or SD is a focal dystonia that affects the vocal cords. It usually becomes apparent between ages 30 to 50 and affects women more frequently than men. There are two distinct forms of SD: adductor SD and abductor SD. Adductor SD is the more common form of this condition and is characterized by contraction of certain vocal muscles that draw the vocal cords together during speech. This causes the voice to have a restricted, strangled, or hoarse quality. Vocal expression is often interrupted by sudden, short pauses followed by abrupt bursts of speech, which may become less and less understandable. In most patients, singing is not as severely affected as speech. In abductor SD, contractions of certain muscles that draw the vocal cords apart causes the voice to have a breathy, whispering quality. Patients tend to "run out of air" as they attempt to speak and are unable to speak loudly. As a result, their speech may also be difficult to understand. Symptom onset is typically relatively gradual. Initial signs often include increased effort during speech and the loss of voice control that occurs with emotional stress. The condition tends to stabilize after about 1 to 2 years of increasing symptom severity. Speech may temporarily improve subsequent to sneezing or yawning. In some patients, sensory tricks, such as pressing the hand on the abdomen or the back of the head, may temporarily relieve symptoms. In up to 30 percent of patients, dystonia may also affect other body regions, particularly the muscles of the neck or head. In addition, SD is sometimes associated with dystonic tremor of the vocal cords that may develop prior to the onset of laryngeal dystonia. Dystonic vocal cord tremors need to be distinguished from essential tremor (ET), a common neurologic movement disorder that is often associated with tremor of the hands or head. Limb Dystonia Focal limb dystonia (LD) is associated with dystonic spasms of arm or leg muscles. These spasms are accompanied by repetitive, twisting movements or abnormal positions or postures of the affected limb. Limb dystonia may be segmental, i.e., affecting muscle groups of an arm as well as the neck, and is also present in those with hemidystonia or generalized dystonia. Upper limb dystonias often appear only when performing specific tasks. Thus, these dystonias are often referred to as task-specific dystonias. The most common task-specific limb dystonia of the arm occurs with writing and is therefore known as writer's cramp. Writer's cramp (WC) typically affects the person's dominant side, meaning the "writing hand." It is often characterized by an abnormally pronounced, forced grip on the writing instrument. This may occur immediately upon grasping the pen or pencil or shortly after beginning to write. Less commonly, there may be excessive extension of the fingers that causes the writing instrument to drop from the hand. Additional findings may include exaggerated flexion or extension of the affected wrist, forcing the palm of the hand downward or upward. In some patients, dystonic spasms may also extend to involve certain muscles of the arm and shoulder, potentially resulting in elevation of the elbow and outward extension of the shoulder. Writing may be labored and shaky with discomfort or pain in the forearm. Some individuals are not able to write–even after just a few words. Touching or stabilizing the affected hand with the other hand may help to alleviate symptoms. In approximately one-third of patients with writer's cramp, dystonic spasms may eventually occur with tasks other than writing. In about 25% who attempt to write with the uninvolved hand, writer's cramp may extend to the previously unaffected hand (bilateral WC). In some patients, dystonic spasms may eventually affect adjacent or other body regions. In addition, writer's cramp is often associated with hand tremor that may occur with writing (action tremor) or while holding the hand in a fixed position against gravity (postural tremor). Other focal task-specific limb dystonias have also been described that may affect... Musicians. Characteristic task-specific dystonias (TSDs) have been reported among pianists, guitarists, and clarinetists. TSDs may affect musicians using almost any type of instrument. Participants in certain sports. For example, TSDs have been described in golfers (a TSD known as the "yips"), tennis players, and dart throwers. Workers in certain occupations, such as seamstresses, shoemakers, or milkers. Generally, activities that may provoke certain TSDs include those requiring highly specialized, precise actions or extremely repetitive movements. Although most TSDs affect the upper limbs, they have rarely been described in the lower limbs, such as among dancers, or cyclists. Lower limb dystonia is a focal dystonia that may primarily affect the ankle and foot, often resulting in inward turning of the heel with upward bending of the sole of the foot. The dystonic spasms initially occur only with walking (action dystonia). However, the dystonia may gradually be present at rest and eventually lead to sustained, fixed postures. Lower LD that appears during childhood is usually associated with the onset of generalized dystonia. However, lower LD that initially becomes evident during adulthood is rare. In such cases, experts indicate that diagnostic evaluations should be conducted to determine whether lower limb dystonia is present secondary to Parkinson's disease, parkinsonism syndromes, or other underlying causes. Other Focal Dystonias Rare forms of focal, typically adult-onset, dystonia have been described, including the following: Truncal dystonia. Dystonic spasms may cause unusual stretching, bending, or twisting of the trunk, sometimes accompanied with sideways curvature of the spine (scoliosis). At symptom onset, the spasms may occur only with standing or walking. Eventually, symptoms may also be present during rest. Dystonic spasms may eventually extend to involve adjacent regions, such as muscles of the upper arms or legs or the pelvis. Abdominal wall dystonia. Also known as "belly-dancer's dyskinesia," this condition is characterized by sustained contractions and involuntary, writhing movements of the abdominal wall. Segmental Dystonia As many as 30 percent of patients with a primary focal dystonia experience dystonic spasms in areas next to the primary site. When dystonia affects two areas of the body that are next to each other, this is termed segmental dystonia. Dystonic spasms affect at least 2 adjacent areas of the body, such as facial and neck muscles ; muscle groups of the neck and upper arm; or trunk and leg muscles. One common segmental dystonia involves muscles of the eyelids, jaw, mouth, and lower face. Known as Meige syndrome, the condition is characterized by periodic or sustained closure of the eyelids (blepharospasm). Eyelid closure is accompanied by forceful spasms of jaw opening or closure, clenching or grinding of the teeth, sideways displacement of the jaw, lip tightening and pursing, and tongue protrusion . In addition, this form of segmental dystonia may spread to neck muscles or other muscle groups. Meige syndrome more frequently affects women than men and typically becomes apparent during the sixth decade of life. Multifocal Dystonia If a focal dystonia spreads to involve an additional area of the body, it usually affects an adjacent area (segmental dystonia). Less commonly, dystonic spasms may begin to affect a non-adjacent region or regions, resulting in signs of multifocal dystonia. In those with multifocal dystonia, the dystonia involves two or more non-adjacent areas of the body, such as both legs; one or both arms and a leg; or the face and a leg. Hemidystonia Hemidystonia is a form of dystonia that affects one side of the body or is characterized by unilateral involvement of the upper and lower limbs. It is considered a type of multifocal dystonia. Hemidystonia typically occurs secondary to certain underlying conditions, particularly multiple sclerosis, tumor, stroke, or vascular malformations. Generalized Dystonia In patients with generalized dystonia, dystonic spasms involve the legs or one leg and the trunk as well as one other area of the body. Unlike primary focal dystonias, primary generalized dystonia is typically associated with a younger age at symptom onset (early onset). "Primary dystonia" indicates that dystonia is the essential or principal finding, with the possible exception of tremor, and that a secondary cause is excluded. Dystonia: Age of Onset The age at symptom onset of primary dystonia is an important indicator of whether the dystonia will potentially progress to involve other body regions. Generally, the younger the patient at symptom onset, the greater the likelihood that dystonia will gradually affect multiple areas of the body. In patients with early-onset primary dystonia, the dystonia usually starts in a leg or arm and progresses to affect other limbs and the trunk. In addition, early onset with initial involvement of a leg is also considered an important indicator suggesting eventual progression to generalized dystonia. In contrast, the older the patient at symptom onset, the greater the likelihood that the dystonia will remain localized , potentially with limited involvement of adjacent regions. In patients with primary late-onset dystonia, the dystonia often begins in the upper body, such as the neck, head and/or neck, or an arm. Dystonia may be classified based upon age of onset as follows: Childhood onset—0 to 12 years Adolescent onset—13 to 20 years Adult onset—older than 20 years The broader term early onset generally refers to dystonia that develops before age 21; however, the late twenties have also been suggested to be early onset. "Late onset" indicates symptom onset later than age 20 or the late twenties. Dystonia: Cause Dystonia may be further classified based upon its cause. More specifically, dystonia may be categorized according to its causes as follows: Primary (idiopathic) dystonia—dystonia is the only sign and a secondary cause is ruled out. Secondary (symptomatic) dystonia—dystonia results primarily from environmental causes, underlying disease, which may or may not be genetic, or injury to the brain. Dystonia-plus syndromes—this classification refers to nondegenerative, neurochemical disorders in which dystonia is associated with other neurologic features, such as myoclonus or parkinsonism. Heredodegenerative dystonia—this category refers to usually hereditary, neurodegenerative disorders in which other neurologic symptoms are present in addition to dystonia. Primary (Idiopathic) Dystonia In patients with primary dystonia, dystonia occurs as the only symptoms with the possible exception of tremor. The primary dystonias are frequently described as "pure dystonias." Primary dystonias were often referred to as "idiopathic torsion dystonia" or ITD, with the term "idiopathic" meaning "of unknown cause or etiology." However, because disease genes have been identified as an underlying cause, most experts now recommend using the term "primary." The word "torsion," which is still in use, refers to the twisting nature of the abnormal movement patterns seen in dystonia. Primary dystonia may be familial or appear to occur in the absence of a family history (sporadic). The primary dystonias include several genetic disorders, some of which have been linked to changes (mutations) of specific genes mapped in some families to a particular chromosome. However, most primary dystonias are sporadic, have adult onset, and are focal or segmental in nature. Certain primary dystonias have been mapped to particular genes. These include... Dystonias Caused by DYT1 Gene Mutation Most cases of early-onset primary dystonias, which may become symptomatic during childhood or early adulthood, are due to mutations of a gene known as DYT1. This gene has been mapped to the long arm of chromosome 9 at 9q34.1. This form of primary dystonia is also known as Dystonia musculorum deformans (DMD). Other forms of DYT1 dystonia include... Early-onset primary dystonia Idiopathic torsion dystonia (ITD) Primary torsion dystonia Primary generalized dystonia To avoid confusion with other primary dystonias, researchers suggest that this form of the disorder should be referred to as DYT1 dystonia or Oppenheim dystonia, after the researcher who first identified the disease. The mean age of onset of DYT1 dystonia is approximately 12 years. Symptoms rarely begin after the age of 29 years. In approximately 90 to 95 percent of cases, symptoms begin in a leg or an arm, and then spread to other regions of the body. Patients whose symptoms initially involve a leg tend to have an earlier age of onset than those whose symptoms initially affect an arm. Symptom onset involving a leg is also associated with an increased likelihood that the condition will evolve to generalized dystonia. The rate of progression to generalized dystonia typically occurs more quickly in patients with leg onset compared to those with initial arm involvement. Although the rate of progression is extremely variable from patient to patient, it usually is more rapid within the first 5 to 10 years following symptom onset. For patients with initial arm involvement, dystonic spasms first appear when performing specific activities, such as writing or playing a musical instrument. As the disease progresses, dystonic symptoms occur with other unrelated activities of the arm and be provoked by the actions of other body parts. This phenomenon is known as overflow. In some affected individuals, walking causes the arm to move backward behind the body. Eventually, dystonia may be present even when the arm is at rest, potentially leading to a sustained, twisted position or posture. For those with symptom onset in the arm, dystonia tends to progress to the other arm or nearby areas of the upper body and neck. There is about a 50 percent chance of progression to generalized dystonia. In contrast, for patients with initial leg involvement, there is an approximate 90 percent chance of progression to generalized dystonia. Those with leg onset develop distinctive gait abnormalities, such as unusual twisting or swinging of the leg as it is moved forward; however, these symptoms may not occur with other activities, such as dancing, running, or walking backward. The hip may also be extended or abducted in an outward position. The foot may swing and elevation or extension of the knee may be present. In some patient, inward turning of the heel and upward bending of the sole of the foot (equinovarus deformity) is associated with difficulty positioning the heel on the ground. In addition, severe flexion of the trunk may result in a "bent over" posture with extension of the neck. As the disease progresses, dystonic spasms occur with less specific activities of the leg and are triggered by actions of other parts of the body (overflow). Eventually, symptoms are present even when the leg is at rest, resulting in abnormal, sustained positions or postures. As DYT1 dystonia progresses, symptoms may spread to involve other areas of the body, particularly in those patient with initial leg involvement. The dystonia may eventually become segmental and then generalized in nature, with distortion of affected regions. In such cases, associated findings may include... Involvement of the neck (cervical dystonia or CD), including jerky head movements. The head may become temporarily tilted or twisted (torticollis) in a sideways, forward, or backward position. These episodes may become more sustained as the disease progresses. Twisting movements or abnormal posturing of the upper body and severe bending of this area. This posturing may result in a fixed sideways curvature of the spine, known as scoliosis. In addition, there may be pronounced inward spinal curvature of the lower back, known as lordosis as well as twisting of the pelvis. Difficulty walking or eventually the inability to walk, in some cases. In rare cases, difficulties in speech or dysarthria may develop along with facial grimacing. However, the throat (pharynx), vocal cords, face, and tongue, tend to remain unaffected. The DYTI gene DYT1 dystonia is an autosomal dominant disorder, meaning that it may be manifested in some individuals who have a single copy of the mutated DYT1 gene. However, the disorder has reduced penetrance. In other words, not all individuals who carry the gene mutation will develop DYT1 dystonia. Evidence suggests that 30 to 40 percent of those with the mutated DYT1 gene have symptoms of the disorder; thus, most people with the mutated gene do not develop symptoms of dystonia. Although most individuals with DYT1 dystonia are affected by early limb-onset dystonia, disease severity may vary greatly from patient to patient. In other words, the DYT1 gene has variable expressivity, meaning that the symptoms vary in range and severity. Some individuals with DYT1 dystonia have no apparent family history of the disorder. This may be explained by low penetrance of the gene in other family members who are carriers or by the variable expression of the condition. Therefore, the disease may remain undiagnosed in mildly affected family members. Other evidence suggests that the disorder results from a new genetic mutation that occurs randomly for unknown reasons (sporadically). The underlying cause or causes of the gene's low penetrance and variable expressivity remain unknown. Various mechanisms may play some role. These include the interaction of other genes that modify or change the activity of other genes, genetic anticipation, or other genetic factors. Environmental influences may also play a role, including trauma, such as injuries to the arms, legs, or head. Symptoms may begin or worsen in a previously injured part of the body. Peripheral injury may influence functioning of the basal ganglia and its pathways and play some role in "triggering" symptom onset in certain individuals who have a mutated DYT1 gene. The mutation responsible for DYT1 dystonia is deletion of one of a pair of certain basic chemical "building blocks" of DNA known as guanine, adenine, and guanine (GAG trinucleotides) in the DYT1 gene's coded instructions. The DYT1 gene regulates or "encodes" production of a protein known as torsinA. Although the protein's specific function is unknown, it appears to be related to a class of proteins (heat-shock proteins) that enable cells to recover from injury or stress. TorsinA is found in neurons throughout the brain. Most ethnic populations are affected by DYT1 dystonia. However, the disorder is most common among individuals of European Ashkenazi Jewish descent. (For further information, please see the section entitled "Epidemiology.") The DYT1 gene mutation is responsible for most cases of early limb-onset primary dystonia in Jewish families (kindreds). Genetic analysis of affected Ashkenazi kindreds has shown that these families share a common set of genes (known as a haplotype) that are closely linked to the DYT1 gene (on chromosome 9q) and typically inherited with it as a unit. (Such sharing of a specific haplotype more commonly than normally expected by chance is known as "linkage disequilibrium.") Experts indicate that the association of the linked genes with DYT1 suggests that the disorder is largely due to a single mutation event in the past (founder mutation). It has been calculated that the original or founder mutation was introduced into the Ashkenazi Jewish population approximately 350 years ago in Lithuania. Genetic analysis has revealed that the DYT1 disease gene also appears to be responsible for most cases of early limb-onset primary dystonia in non-Jewish kindreds. However, such investigation has not revealed a common set of closely linked genes (i.e., linkage disequilibrium) to suggest a single founder mutation in these non-Jewish families. In a study of 174 Ashkenazi individuals with early- or late-onset primary dystonia, more than 90 percent of those with isolated or familial early limb-onset dystonia carried the chromosome 9q haplotype. Most of these patients had progression to multifocal or generalized dystonia. In contrast, those who did not carry the haplotype comprised the majority of patients who had late-onset dystonia with initial involvement of head or neck (cervical) muscles rather than limb muscles. In almost all of these patients, the dystonia remained focal or segmental. Thus, such evidence suggests that a single mutation event is responsible for most cases of early limb-onset dystonia in individuals of Ashkenazi descent, yet is not the cause of primary adult-onset cervical dystonia. Rather, researchers indicate that the latter may result from either DYT1 mutations, other dystonia genes, and/or other factors. In at least some families, evidence suggests that late-onset and cervical- or cranial-onset primary dystonia–or, more rarely, late-onset dystonia that also involves the legs or trunk–is due to mutation of other dystonia genes. Accordingly, following is a description of primary dystonias that have been mapped to genes other than the DYT1 gene (or simply excluded from the DYT1 gene) in certain families. DYT6 Dystonia DYT6 dystonia is an autosomal dominant primary dystonia that has been mapped to chromosome 8 (8p21q22). The disorder has been described in members of 2 large Mennonite families (kindreds). Affected members of these kindreds have been shown to share a common set of genes (haplotype) closely linked to DYT6, suggesting a shared mutation in the past. Symptoms, which may become apparent in either childhood or adulthood, may initially affect muscles of the limbs or the neck (cervical) regions. In almost all affected members, there has been extension of the dystonia from the initial site of involvement to multiple body regions, with most affected by dystonia of limb, head, and cervical regions. Reports suggest that the most disabling feature of the disorder often consists of severe difficulties articulating speech (dysarthria). DYT7 Dystonia Several families have been described with autosomal dominant, adult-onset, primary dystonia that is focal in distribution, affecting the neck region (known as familial torticollis). In a German kindred, the autosomal dominant disorder has been mapped to chromosome 18p. This genetic location (locus) has been designated as DYT7. However, other kindreds with familial torticollis have been excluded from the DYT7 (as well as the DYT1) regions and the responsible gene location has not yet been identified. Other Familial Primary Dystonias Additional families have also been described with autosomal dominant primary dystonias that have been excluded from the DYT1 region. These include kindreds with a form of primary dystonia that usually initially affects the neck (cervical) region, often spreads to involve head, and, in some instances, affects the arm. In addition, the dystonia has become generalized in a few cases. Symptom onset has occurred during childhood or adulthood. This type of dystonia, sometimes described as "familial cervical-cranial predominant dystonia," has been reported in some non-Jewish families, including Italian and North American kindreds. Research is ongoing to determine additional genes, specific gene mutations, and/or environmental factors that may play some role in causing primary dystonia in certain families. Other familial primary dystonias that have been given specific "genetic designations" include the following: DYT2: This genetic designation has been reserved by experts for any possible autosomal recessive form of familial primary dystonia. However, none has been confirmed to date. DYT4: This refers to an autosomal dominant primary dystonia in a large, multigenerational Australian kindred affected by abductor ("whispering") spasmodic dysphonia (laryngeal dystonia). Although the dystonia first involved speech in most affected family members, a few initially were affected by dystonia of the neck region, later developing dysphonia. (For further information, see the section entitled "Anatomical distribution, focal dystonia, laryngeal dystonia.") Researchers expect that additional familial primary dystonias will be described that may map to other, currently unknown genetic loci. (For further information on dystonias that have been given specific genetic designations, please see the section entitled "Genetic Designations for the Dystonias.") Primary Adult-onset Focal/Segmental Dystonias As discussed earlier, focal dystonia refers to dystonia that is limited to a single region of the body. In some patients, focal dystonias may extend to involve adjacent areas, resulting in segmental dystonia. Primary focal dystonia is most commonly of adult onset, often becoming apparent during the fourth or fifth decade of life. The cause of primary adult-onset focal dystonia is usually unknown, with the condition appearing to occur in the absence of a family history (sporadically). Rarely, however, more than one family member may be affected. For example, as mentioned earlier, a gene location (designated DYT7) for adult-onset primary dystonia predominantly affecting the neck region (familial torticollis) has been mapped to chromosome 18p in a German family. However, in most cases, the role of heredity in primary adult-onset focal/segmental dystonia remains unknown. Yet some experts suggest that heredity may be a factor in the development of these dystonias, based upon several findings, such as the following: In addition to the kindreds discussed above, familial cases of primary adult-onset focal dystonia have been reported, including cervical dystonia, writer's cramp, and orofacial dystonia. In one study, 25 percent of 40 non-Jewish individuals with focal dystonia (e.g., cervical dystonia, cranial dystonias, writer's cramp) had relatives with symptoms of dystonia. According to multiple large studies of primary adult-onset focal dystonia, 2 to 15 percent of patients have had relatives with signs of focal or segmental (but not generalized) dystonia. Based upon these and other findings, some researchers suggest that primary adult-onset focal dystonias may commonly be transmitted as an autosomal dominant trait with reduced penetrance and variable expressivity. In addition, some investigators speculate that adult-onset primary focal dystonias may represent a localized manifestation of primary generalized dystonia, with the final anatomical distribution reflecting patient age and specific site of onset. Possible support for this theory includes the fact that primary generalized dystonia often begins as a focal dystonia. In addition, primary focal and generalized dystonias are both characterized by effective "sensory tricks" and both respond similarly to certain medications. Yet, as mentioned earlier, dystonia that begins in the neck or cranial region rarely results from mutations of the DYT1 gene, indicating that most focal dystonias that do not begin in a limb are probably distinct from primary generalized dystonia. Therefore, whether primary focal and generalized dystonias may be variations of the same disorders or are truly distinct disease entities remains unclear. Some studies also suggest that focal dystonia may be precipitated by trauma and/or overuse of the affected bodily region (i.e., peripheral factors). As mentioned earlier, some investigators theorize that prior trauma may play some role in triggering disease onset in patients who carry a mutated DYT1 gene for DYT1 dystonia. In addition, several studies have suggested a possible association of focal dystonias with prior peripheral trauma. For example, researchers have reported that... Trauma occurred 3 to 6 months prior to symptom onset in approximately 5 to 12 percent of patients with cervical dystonia. Inflammation of the vocal cords (laryngitis) has occurred prior to the onset of laryngeal dystonia in some patients. Writer's cramp has sometimes occurred subsequent to localized hand injury. Oromandibular dystonia (OMD) has been described following dental treatment. In some cases, the relationship between trauma and the onset of dystonia is clear when dystonia follows brain injury or severe peripheral trauma. (For further information, please see the section entitled "Etiology/Secondary Dystonia.") However, researchers indicate that, in many instances, the relationship is less clear and trauma alone probably would not be sufficient for the development of dystonia. Rather, they suggest that trauma may play some role in triggering dystonia in those with previously, very mild, undetectable cases–or in patients with an existing, potentially genetic, susceptibility to the disorder. Further research is necessary to determine the various underlying genetic, environmental, and/or other underlying mechanisms that may play a role in causing the primary dystonias. (For more information, please see the section entitled "Pathophysiology.") Secondary (Symptomatic) Dystonia Secondary dystonia refers to dystonia that results primarily due to environmental factors or "insults" that affect the brain. In addition, spinal cord or peripheral injury may also be responsible for secondary dystonia. Causes of secondary or symptomatic dystonia include the following: Abnormalities of brain function due to insufficient oxygen supply to tissues shortly before, during, or after birth (perinatal cerebral anoxia), such as cerebral palsy Vascular malformations of the brain in which a tangle of abnormal blood vessels form communications between the arterial and venous systems (arteriovenous malformations) Brain tumors Brainstem lesions Head injury Inflammatory, infectious, and postinfectious conditions affecting the brain (encephalitis), such as Reye syndrome, Creutzfeldt-Jakob disease (CJD), and human immunodeficiency virus (HIV) infection Stroke or localized brain damage due to temporary interruption of its blood supply or leakage of blood outside blood vessel walls (cerebral infarction or hemorrhage) Multiple sclerosis (MS), a progressive disease of the central nervous system characterized by loss of myelin Thalamotomy, a procedure involving surgical destruction (ablation) of a selected region of the thalamus, which is a paired structure deep in the brain involved in regulating movement. This procedure has been used to help treat certain neurologic movement disorders, including Parkinson's disease, essential tremor, and dystonia. Injury or lesions of the spinal cord within the neck region (cervical spinal cord) Narrowing (stenosis) of the spinal canal within the lower back region (lumbar canal stenosis). (The spinal canal is the cavity within the spinal column that contains the spinal cord.) Peripheral trauma, which may be followed by focal dystonia in the affected body part Certain metabolic conditions, such as hypoparathyroidism, which is characterized by decreased activity of the parathyroid glands Prolonged or substantial exposure to toxic environmental agents, such as carbon monoxide, cyanide, manganese, or methanol Therapy with certain medications, such as the following: o Particular anticonvulsant medications, including phenytoin (Dilantin®) or carbamazepine (Tegretol®) o Dopamine receptor blockers (antagonists), such as certain antipsychotic drugs, including haloperidol (Haldol®); antidepressants, such as amoxapine (Asendin®); antinausea (antiemetic) medications, such as prochlorperazine (Compazine®) or metoclopramide (Reglan®); or other agents. In some patients, therapy with certain dopamine receptor blockers may result in a sudden (acute) onset of dystonia or the development of persistent dystonia known as tardive dystonia. o Levodopa (L-dopa), a precursor of the neurotransmitter dopamine, for the treatment of parkinsonism Psychogenic changes in which symptoms have a mental or an emotional basis rather than an organic origin Secondary dystonia most commonly results from therapy with dopamine receptor antagonists (i.e., tardive dystonia). In adults, tardive dystonia is often focal or segmental in nature and may sometimes be difficult to distinguish from primary adult-onset dystonias, necessitating a careful patient medication history. For example, tardive dystonia often initially involves muscles of the face or neck and may resemble oromandibular/lingual dystonia or other primary adult-onset focal dystonias. Involvement may remained confined to the initial site or become segmental, affecting the arms and trunk. In children, however, tardive dystonia is more likely to be generalized in nature, involving limb and trunk muscles. Other common causes of secondary dystonia include perinatal cerebral anoxia, psychogenic causes, stroke, or inflammatory conditions of the brain (encephalitis). In addition, as mentioned above, researchers continue to question the relationship between injury and the development of dystonia in some cases, such as the potential role peripheral trauma may play in "triggering" dystonia onset in patients who carry a copy of the mutated DYT1 gene. (For further information, see the section entitled "Etiology/Primary Dystonia.") However, evidence suggests that the relationship between injury and secondary dystonia is sometimes clear, such as due to localized brain injury or severe peripheral trauma. In those with apparent, peripherally induced dystonias, the region injured is usually the area that develops dystonia. For example, blepharospasm has been reported following localized eye disease and cervical dystonia has developed subsequent to whiplash. Experts indicate that peripherally induced dystonias may tend to differ from other secondary dystonias in some areas, such as the following: A relatively short period between the event and symptom onset. In contrast, dystonia that occurs secondary to localized brain lesions sometimes may not develop for long periods. For example, children who had insufficient oxygen supply to the brain during birth may not develop associated dystonia for several years, such as when they are approximately 7 or 8 years of age. From the onset of symptoms, dystonia present during periods of rest Persists during sleep Limited range of movement and fixed postures Potentially associated with development of pain (causalgia or reflex sympathetic dystrophy) Absence of temporary improvement with "sensory tricks" (i.e., no gestes antagonistes) (For more information on the potential relationship between trauma and the development of dystonia, please see the section entitled "Pathophysiology.") Signs Potentially Suggestive of Secondary Dystonia Evidence suggests that the relative association between age at symptom onset and disease course is somewhat different for those with secondary dystonia in comparison to patients with primary dystonia. For example: Generally, for those with primary dystonia, the younger the patient at symptom onset, the greater the likelihood that the dystonia will become generalized. However, secondary dystonia beginning during adulthood is more likely to generalize than in those with adult-onset primary dystonia. A relatively higher percentage of patients with secondary dystonia seem to have early symptom onset or a form of generalized dystonia. In addition, according to experts, there are a number of factors that may suggest that dystonia is secondary rather than primary. Such factors may include the following: Patient history of a possible causative (etiologic) factor, such as exposure to certain medications or toxins; perinatal cerebral anoxia; inflammatory conditions of the brain (encephalitis); or head, spinal, or peripheral trauma Dystonia that occurs in association with other neurologic signs, such as symptoms of parkinsonism, including rigidity, slowness of movement (bradykinesia), and postural instability; myoclonus; sudden episodes of uncontrolled electrical activity in the brain (seizures); certain eye (ocular) abnormalities; muscle weakness; impaired coordination of voluntary movements (ataxia); spasticity; dementia; or other findings Dystonia that occurs during periods of rest, rather than during voluntary action. Primary dystonia typically initially occurs with certain voluntary movements (action dystonia); in contrast, some secondary dystonias may initially be characterized by dystonia of the affected body part at rest (rest dystonia. Initial leg involvement during adulthood. (As noted previously, lower limb dystonia that initially becomes evident in an adult is extremely rare. Thus, in such cases, diagnostic evaluations should be conducted to determine whether the condition has occurred secondary to Parkinson's disease, other parkinsonism syndromes, or other underlying conditions.) Hemidystonia. (Evidence suggests that a significantly higher percentage of patients with secondary dystonia develop hemidystonia compared with those affected by primary dystonia.) Early onset of speech involvement in association with dystonia Abnormal laboratory test results Abnormal neuroimaging results, such as based upon computed tomography (CT) scanning or magnetic resonance imaging (MRI) Signs suggestive of psychogenic causes, such as an abrupt onset, spontaneous remissions, disappearance of dystonic movements with distraction, etc. Drugs That May Cause Dystonia Drugs belonging to a class called "dopamine receptor blocking agents" (DRBAs) can cause dystonia. The following is a list of such drugs that can cause dystonia. Generic (Trade Names) Acetophenazine (Tindal®) Amoxapine (Asendin®) Chlorpromazine (Thorazine®) Fluphenazine (Permitil®, Prolixin®) Haloperidol (Haldol®) Loxapine (Loxitane®, Daxolin®) Mesoridazine (Serentil®) Metaclopramide (Reglan®) Molindone (Lindone®, Moban®) Perphenazine (Trilafon® or Triavil®) Piperacetazine (Quide®) Prochlorperazine (Compazine®, Combid®) Promazine (Sparine®) Promethazine (Phenergan®) Thiethylperazine (Torecan®) Thioridazine (Mellaril®) Thiothixene (Navane®) Trifluoperazine (Stelazine®) Triflupromazine (Vesprin®) Trimeprazine (Temaril®) Dystonia-plus Syndromes Experts established the "dystonia-plus syndrome" etiologic classification to help differentiate dystonic disorders that are distinct from primary (idiopathic) dystonias; secondary (symptomatic) dystonias; and neurodegenerative, usually hereditary (heredodegenerative) disorders in which other neurologic signs are typically present. In contrast, the dystonia-plus syndromes include nondegenerative, neurochemical disorders characterized by dystonia as well as additional neurologic features, such as myoclonus or parkinsonism. Myoclonus is characterized by sudden, involuntary, "shock-like" muscle contractions. In addition, these brief, jerk-like movements are often accompanied by periodic interruptions in voluntary muscle contraction (muscle inhibition), leading to lapses of sustained posture. Signs of parkinsonism include slowness of movement (bradykinesia), rigidity, postural instability, and tremor at rest. Dystonia-plus syndromes currently include the following: Dopa-responsive dystonia (DRD) or Segawa syndrome Rapid-onset dystonia-parkinsonism (RDP) Myoclonus-dystonia Dopa-responsive Dystonia Also known as Segawa syndrome, dopa-responsive dystonia (DRD) is a genetic disorder that typically becomes apparent from approximately age 6 to 16. Girls are affected about 2 to 4 times more frequently than boys. Evidence suggests that approximately 10 percent of patients with childhood-onset dystonia are affected by DRD. In many patients, onset is characterized by an abnormal, "stiff-legged" manner of walking (gait), with upward bending of the sole of the foot (plantar flexion) or turning of the foot outward at the ankle (eversion) and a tendency to walk on the toes. Dystonia may also extend to involve muscles of the arms, trunk, and, less frequently, the neck. In addition, DRD is typically characterized by signs of parkinsonism that may be relatively subtle. Such signs may include slowness of movement (bradykinesia), stiffness and resistance to movement (rigidity), balance difficulties, and postural instability. Approximately 25 percent also have abnormally exaggerated reflex responses (hyperreflexia), particularly in the legs. Many patients experience improvement with sleep, are relatively free of symptoms in the morning, and develop increasingly severe symptoms as the day progresses (i.e., diurnal fluctuation). Accordingly, this disorder has sometimes been referred to as "progressive hereditary dystonia with diurnal fluctuations." Yet some DRD patients do not experience such diurnal fluctuations, causing many researchers to prefer other disease terms. For example, in those with DRD, symptoms typically dramatically improve with low-dose administration of levodopa (L-dopa), an amino acid that is a biologic "forerunner" or precursor of the neurotransmitter dopamine. (Neurotransmitters are naturally produced chemicals that may transfer nerve impulses across the spaces between neurons, enabling nerve cells to communicate.) Low-dose L-dopa usually results in near-complete or total reversal of all associated symptoms for these patients. In addition, the effectiveness of such therapy is typically long term, without the complications that often occur for those with Parkinson's disease who undergo L-dopa treatment. Thus, most experts indicate that this disorder is most appropriately known as dopa-responsive dystonia (DRD). DRD is an autosomal dominant disorder that usually appears to result from mutations of a gene known as guanosine triphosphate (GTP) cyclohydrolase I (GCH1 or DYT5). The GCH1 gene, which has been mapped to chromosome 14q22.1, regulates production of an enzyme that speeds (catalyzes) the first step in the "building up" of a compound (i.e., the cofactor tetrahydrobiopterin) required for tyrosine hydroxylase and other enzymes. In turn, these enzymes are required for the production (synthesis) of certain neurotransmitters, such as dopamine. In patients with DRD, there are significantly reduced dopamine concentrations in substructures of the basal ganglia collectively known as the striatum. (As mentioned earlier, the basal ganglia are specialized nerve cell clusters deep within the brain that play an essential role in regulating motor behavior.) As with DYT1 dystonia, DRD has reduced penetrance and variable expressivity. In other words, evidence suggests that only about 30 to 40 percent of those who carry a copy of the disease gene manifest symptoms. In addition, the severity of associated symptoms may vary greatly from patient to patient, including among affected members of the same family (kindred). Related genetic disorders have been described that may result in similar symptoms and signs (phenotype), with improvement from therapy with L-dopa or certain agents that produce dopamine-like effects (dopamine agonists). For example... A rare autosomal recessive disorder has been reported in which mutation of the gene that regulates production of tyrosine hydroxylase (see above) results in symptoms similar to those of DRD. Such symptoms also respond to L-dopa therapy. In patients with this disorder, signs of dystonia and parkinsonism typically begin during infancy or early childhood. Several autosomal recessive disorders have also been described in which biopterin deficiency is associated with dystonia, parkinsonism, as well as signs resulting from decreased levels of the neurotransmitters serotonin and norepinephrine. These may include rigidity, chorea, myoclonus, temperature disturbances, sudden episodes of uncontrolled electrical activity in the brain (seizures), contraction of the pupils (miosis), and abnormally increased levels of the amino acid phenylalanine in the blood (hyperphenylalaninemia). Patients with these disorders may have partial response to therapy with L-dopa. Another variant of DRD is an autosomal recessive disorder characterized by deficiency of the enzyme aromatic amino acid decarboxylase, which speeds the conversion of levodopa to dopamine. Associated symptoms become apparent during infancy. Such findings may include dystonia, parkinsonism, excessive sweating (hyperhidrosis), diminished muscle tone (hypotonia), feeding difficulties, drooping of the upper eyelids (ptosis), and contraction of the pupils (miosis). There may also be episodes of sudden, transient, involuntary movements; in which the eyes are held in a fixed position, such as up, down, or sideways, potentially with spasms or closure of the eyelids (oculogyria); and/or of periods of deep sleep. Symptoms respond to therapy with dopamine agonists and monoamine oxidase inhibitors. Rapid-onset Dystonia-parkinsonism Rapid-onset dystonia-parkinsonism (RDP) is an autosomal dominant disorder that has been mapped to chromosome 19q (DYT12). Symptom onset may occur during childhood, adolescence, or adulthood. RDP is characterized by the abrupt development over hours, days, or weeks of combined dystonia and parkinsonism. In many cases, the sudden onset or worsening of symptoms may develop following certain stressful events, such as exposure to extreme heat, running, childbirth, or fever. In patients with RDP, findings may include the following: Dystonic movements or postures of the limbs, with the arms typically more affected than the legs Poverty of movement (bradykinesia) Impaired articulation of speech (dysarthria) Difficulties swallowing (dysphagia) Postural instability Reports indicate that some members of affected kindreds may have an isolated, relatively mild, intermittent limb dystonia of the hand and/or foot that may remain unchanged or may be present years before the sudden onset of combined dystonia-parkinsonism. Diagnostic testing may reveal abnormally low levels of homovanillic acid (HVA) in the cerebrospinal fluid (CSF). Homovanillic acid is produced by normal metabolism of the neurotransmitter dopamine. Depleted levels of HVA may be detected in affected individuals, those who carry a copy of the mutated gene yet have no associated symptoms (asymptomatic carriers), or unaffected individuals with a symptomatic sibling or parent (at-risk individuals). In contrast to DRD, treatment with L-dopa or dopamine agonists provides only minimal benefit. Because neuroimaging techniques have not detected pathologic abnormalities in RDP, this disorder is often classified as a dystonia-plus syndrome. However, as neuropathologic studies become available, some investigators suspect that it may be shown to be neurodegenerative in nature and thus may be more appropriately classified as a heredodegenerative dystonia. (For further information, please see the section entitled "Etiology/Heredodegenerative Dystonia.") Myoclonus-dystonia Primary dystonias, particularly DYT1 dystonia, may be associated with brief, myoclonic muscle jerks. However, researchers have described a distinct genetic disorder in which dystonia may be associated with marked, rapid, "lightening-like" myoclonus. Currently known as "myoclonus-dystonia" or "inherited myoclonus-dystonia syndrome," the disorder is characterized by variable combinations of dystonia and myoclonus without other signs or symptoms of neurologic dysfunction (e.g., seizures, dementia, or impaired coordination of voluntary movements [ataxia]). As mentioned earlier, myoclonus refers to sudden, involuntary, "shock-like" muscle contractions, often accompanied by periodic interruptions in voluntary muscle contraction (muscle inhibition). Many researchers suggest that myoclonus-dystonia may represent the same disease entity as so-called "hereditary essential myoclonus," a usually familial disorder in which myoclonus is an isolated or primary finding often occurring in association with dystonia. In patients with myoclonus-dystonia, associated symptoms usually become apparent during childhood or adolescence, although onset may occur during adulthood. Myoclonus is often the most prominent feature, primarily affecting muscles of the arms, shoulders, neck, and trunk and usually sparing the face and legs. The myoclonic jerks typically occur or worsen with voluntary movement (action myoclonus) and may be exacerbated by stress or fatigue. In addition, in many patients, consumption of alcohol may alleviate myoclonus; however, a "rebound" worsening of symptoms has sometimes been described subsequent to alcohol intake. In addition to myoclonus, some affected individuals may also develop abnormal dystonic movements and postures. Myoclonic jerks and dystonic spasms may affect the same muscle groups or occur independently of one another. Various forms of dystonia have been reported in affected family members, including upper limb, cranial, cervical, and trunk dystonia. Rarely, dystonia may be the sole finding associated with the disorder. The course of myoclonus-dystonia is usually relatively benign. In members of some families, the dystonia or myoclonus may appear to spontaneously subside (remission). However, in most patients, symptoms gradually progress for a few years and then tend to stabilize with periodic fluctuations or have mild spontaneous improvement. Myoclonus-dystonia is transmitted as an autosomal dominant trait that appears to have reduced penetrance and variable expressivity, with males more commonly affected (in contrast to DRD). Genetic analysis of one family with 8 affected members demonstrated mutations of the gene that regulates production of the D2 dopamine receptor (DRD2) protein. The genetic locus (designated DYT11) has been mapped to chromosome 11q23. Further research is needed to determine whether all families with myoclonus-dystonia (and the entity known as hereditary essential myoclonus) are indeed affected by the same genetic disorder. Heredodegenerative Dystonia This etiologic classification refers to disorders in which neurodegenerative changes may lead to dystonia as a primary feature and other neurologic symptoms are typically apparent, particularly parkinsonism. However, in some patients with these disorders, dystonia may not develop and other neurologic features may be primary findings. The term "heredodegenerative" is used since many of these disorders are hereditary; however, it is important to note that some are of unknown cause. The heredodegenerative dystonias include numerous disorders, such as certain X-linked recessive, autosomal dominant, autosomal recessive, and/or parkinsonism syndromes. Such disorders include the following: X-linked dystonia-parkinsonism (Lubag) Huntington's disease Wilson's disease Neuroacanthocytosis Rett syndrome Parkinson's disease Juvenile parkinsonism Other heredodegenerative dystonias X-linked Dystonia-parkinsonism (Lubag) Known as X-linked dystonia-parkinsonism or Lubag (which is its Filipino name), this neurodegenerative disorder is transmitted as an X-linked recessive trait. It has primarily been reported in young adult males from the island of Panay in the Philippines. However, a few cases have been described in which females who carry a copy of the disease gene (heterozygous carriers) may manifest mild symptoms of the disorder, such as relatively mild dystonia or chorea. The mean age at onset is approximately 35 years, with 14 years the youngest reported age at onset. Symptoms may initially include focal dystonia of the neck; lower limbs; upper limbs; or trunk. Cranial involvement often affects muscles of the jaw, mouth, lower face, and tongue (oromandibular/lingual dystonia). In addition, in those with involvement of the vocal cords, symptoms may include an unusual, high-pitched sound upon inhalation (stridor). With disease progression, the dystonia usually becomes generalized. In some patients, signs of parkinsonism may accompany, precede, or "replace" symptoms of dystonia. Such findings may include stiffness (rigidity), slowness of movement (bradykinesia), a shuffling manner of walking (gait), and/or postural instability (although resting tremor is rarely present). Less commonly, patients may develop progressive parkinsonism as an isolated manifestation of the disorder. The gene for X-linked dystonia-parkinsonism (DYT3) has been mapped to chromosome Xq13.1. Neuroimaging studies may reveal neurodegenerative changes (e.g., gliosis and neuronal loss) within substructures of the basal ganglia (i.e., striatum). Parkinsonism symptoms may slightly improve with L-dopa or dopamine agonist therapy, and dystonic features may have only a partial response to anticholinergics or benzodiazepines, such as clonazepam (Klonopin®). (For further information, please see the section entitled "Treatment.") Huntington's Disease Huntington's disease (HD) is a genetic, progressive, neurodegenerative disorder that usually becomes apparent during the fourth or fifth decades of life. However, the age at onset is variable and ranges from early childhood to late adulthood. HD is primarily characterized by the development of emotional, behavioral, and psychiatric abnormalities; loss of previously acquired intellectual or cognitive functioning; and movement abnormalities (motor disturbances). The classic signs of HD include the development of chorea—or involuntary, rapid, irregular, jerky movements—as well as the gradual loss of thought processing and acquired intellectual abilities (dementia). Dementia may be associated with impairment of memory, abstract thinking, and judgment; improper perceptions of time, place, or identity (disorientation); increased agitation; and personality changes (personality disintegration). In patients with HD, the chorea may originally be limited to the fingers or toes but may eventually extend to involve the arms, legs, face, and trunk. As the disease advances, choreic movements tend to become generalized and essentially blend or flow into one another, causing them to appear relatively slow and writhing in nature (athetosis). Late in the disease course, the involuntary movements may develop a dystonic quality in which there may be unusual twisting motions and alternating or fixed postures resulting from sustained muscle contractions. In addition, dystonia may occur as a complication of therapy with dopamine receptor blockers (antagonists). In patients who develop symptoms before age 20 (juvenile HD), motor disturbances may be characterized by muscle stiffness and resistance to movement (rigidity), relative slowness of movement (bradykinesia), tremors, and dystonia. HD may be inherited as an autosomal dominant trait or, less commonly, occur as the result of a new (sporadic) mutation of the disease gene. The disorder results from abnormally long sequences or "repeats" of certain basic chemical "building blocks" of DNA known as cytosine, adenine, and guanine (i.e., unstable expanded CAG trinucleotide repeats) within the disease gene's coded instructions. The disease gene, known as IT15, is located on chromosome 4p16.3. The IT15 gene regulates or encodes production of a protein known as huntingtin that is found in nerve cells (neurons) throughout the brain. Progressive nervous system dysfunction associated with HD results from loss of neurons in certain areas of the brain, including the basal ganglia and cerebral cortex. Wilson Disease Wilson's disease is a genetic disorder of copper metabolism, leading to an excessive accumulation of copper in certain tissues and organs, including the liver, brain, kidneys, and/or corneas of the eyes. Without prompt, appropriate treatment, the disorder may result in progressive liver disease, degenerative changes of the brain, psychiatric abnormalities, and other findings. Generally, the younger the age at symptom onset, the greater the degree of liver (hepatic) involvement. Associated findings may include enlargement of the liver (hepatomegaly), acute or chronic liver inflammation (hepatitis), scarring and impaired functioning of the liver (cirrhosis), and other complications. Neurologic signs of Wilson's disease appear to predominate in those with symptom onset after age 20. Such neurologic signs typically become apparent in the second or third decade of life, although they may appear as late as the sixth decade. These findings may include dystonia; muscle stiffness (rigidity); tremor; impaired coordination of certain voluntary movements (ataxia); "swaying" of the head (head titubation); increasingly impaired articulation of speech (dysarthria); and/or other findings. Dystonia involving muscles of the face, tongue, and throat (pharynx) may cause or contribute to dysarthria and may lead to additional findings, such as an unusual whispering quality to the voice ("whispering" dysphonia), drooling, and/or a fixed grinning expression (risus sardonicus). In addition, dystonic movements and abnormal postures may affect muscles of the arms, legs, and trunk. Some patients may also develop cognitive changes, resulting in increasing irritability, anxiety, severe depression, unusual behaviors, or other psychiatric problems. Additional findings associated with Wilson's disease may include the presence of distinctive, golden brown rings at the outer margins of the corneas (Kayser-Fleischer rings); premature destruction of red blood cells, leading to decreased levels of the oxygen-carrying component of the blood (hemolytic anemia); and/or progressive kidney failure. Wilson's disease is inherited as an autosomal recessive trait. The disorder results from changes (mutations) in a gene, known as ATP7B, located on chromosome 13 (13q14.3). The ATP7B gene regulates production of a protein that plays a role in the transport of copper (copper-transporting ATPase). Although the specific underlying defect in Wilson's disease is unknown, some researchers suggest that it may be related to the body's inability to produce sufficient levels of ceruloplasmin, an enzyme in the fluid portion of the blood that binds to copper and is involved in its transport and regulation. In patients with neurologic signs of the disease, such findings are thought to result from progressive involvement of certain regions of the basal ganglia. Neuroacanthocytosis Also known as choreoacanthocytosis, this neurodegenerative disorder is usually inherited as an autosomal recessive trait. Symptoms typically become apparent between the ages of 25 to 45 years. The disorder may be characterized by dystonia; chorea; tics, including lip "smacking" and "hissing" vocalizations; personality changes and cognitive decline; seizures; parkinsonism; and/or atrophy of muscle tissue (amyotrophy) with an abnormally high length-wise arch of the foot (pes cavus). The dystonia may affect muscles of the face, mouth, and tongue and may often be provoked by eating (i.e., action dystonia), leading to potentially mutilating lipand tongue-biting. Neuroacanthocytosis is associated with atrophy and neuronal loss within substructures of the basal ganglia, including the caudate nuclei and putamen (collectively known as the striatum) and the globus pallidus. There may also be neurodegenerative changes within the thalamus and certain regions of the spinal cord (i.e., anterior horns). The disorder may be confirmed by blood tests indicating that over 15 percent of red blood cells are acanthocytes or abnormal circulating red blood cells that have spur-like or thorny projections (i.e., acanthocytosis). Rett Syndrome Rett syndrome (RS) is a progressive neurodevelopmental disorder of childhood onset that occurs almost exclusively in females. Infants and children with RS usually appear to develop normally until about 6 to 18 months of age. They may then cease to acquire new skills and gradually or suddenly lose previously obtained skills (developmental regression), such as conscious control of the hands and the ability to vocalize most sounds or words. Acquired hand and finger use is gradually replaced by repetitive, distinctive, uncontrolled hand movements, such as hand clapping, clenching, grasping and releasing, patting, mouthing, or "washing" and wringing. In addition, the tongue may repeatedly twist or contort in ineffective chewing movements, and there may be involuntary grinding, gnashing, or clenching of the teeth (bruxism). Affected children may also develop autistic-like behaviors; an impaired ability to perform the motor movements required for coordinating walking (gait apraxia) and trunk movements; breathing irregularities during waking hours; seizures; feeding and swallowing difficulties; and growth retardation. Over time, some patients may develop increasing motor difficulties, whereas other associated symptoms may tend to stabilize or improve over time. Increasing motor difficulties may include loss of the ability to walk (although some may never have gained this ability); increasing muscle weakness; spasticity; dystonia, most often involving the legs; and/or other involuntary movements, such as myoclonus or athetosis. RS usually appears to occur randomly for unknown reasons (sporadically) in the absence of a family history. Yet there have been some instances in which the disorder has affected more than one family member, particularly sisters or identical twins. In such cases, the disorder's mode of inheritance remains uncertain, although some researchers suggest that RS may be transmitted as an X-linked dominant trait or be due to germline mosaicism in a parent. In some females, RS is caused by mutations of a gene known as MECP2 on chromosome X (Xq28) that is thought to be critical in brain development. The protein regulated by this gene (methyl-CpG-binding protein 2 [MeCP2]) helps to control the expression of other genes or essentially "silence" other genes at certain critical times in development. Some researchers have speculated that RS may also result from mutations of DNA within mitochondria (mtDNA)—i.e., the relatively small, rod-like structures outside the nuclei of cells that serve as a major source of cellular energy. Although the basic underlying defect in RS is unknown, defective maturation of several neurotransmitter systems is thought to play some role. Researchers have demonstrated reduced activity of several neurotransmitters, including dopamine, norepinephrine, acetylcholine, and serotonin, in certain regions of the basal ganglia and cerebral cortex. Parkinson's Disease Parkinson's disease (PD) is a progressive neurodegenerative disorder with a mean age of onset of approximately 55 years. Symptom onset before age 20 is known as juvenile parkinsonism (see below). PD is characterized by slowness or poverty of movement (bradykinesia); muscle stiffness and resistance to movement (rigidity); postural instability; and tremor primarily while at rest. Additional characteristic findings may include a shuffling, unbalanced manner of walking; forward bending or flexion of the trunk; decreased blinking and a fixed or "mask-like" facial expression; an unusually soft, weak voice; abnormally small, cramped handwriting (micrographia); depression; or other symptoms and findings. Dystonia may occur in association with untreated PD, such as action-induced bending (flexion) of the foot that worsens with walking. More specifically, there may be inward turning of the heel and upward bending (flexion) of the sole of the foot (equinovarus deformity), with flexion of the second to fifth toes and backward flexion (i.e., upward bending or dorsiflexion) of the great toes. As mentioned earlier, adult-onset lower limb dystonia suggests the possibility of PD or other parkinsonism syndromes. Many PD patients also may develop dystonic flexion of the trunk during the disease course. Less commonly, untreated PD patients may be affected by dystonia of the upper limbs. In addition, there have been a few reports in which untreated individuals developed hemidystonia or focal dystonia of muscles of the eyelids (blepharospasm); jaw, mouth, and lower face (oromandibular dystonia); or neck (cervical dystonia). However, some researchers have questioned the significance of such findings, indicating that the frequency of focal dystonia in PD is similar to its expected frequency in the same age group. As mentioned earlier, dystonia may also develop as a complication of therapy for PD, occurring secondary to the administration of L-dopa. The specific cause of PD remains unknown. Ongoing research has focused on the role that various genes, exposure to certain chemicals, and other mechanisms may play in potentially causing the disorder. The symptoms and findings associated with PD are thought to primarily result from progressive loss of nerve cells within a certain region of the substantia nigra and the striatum (nigrostriatal system) of the brain and associated deficient production of the neurotransmitter Juvenile Parkinsonism Juvenile parkinsonism is a general term that refers to progressive neurodegenerative disorders in which signs of parkinsonism develop before approximately age 20. Juvenile parkinsonism may be primary and familial or may occur secondary to other heredodegenerative disorders, such as Huntington's disease. Families have been reported in which primary juvenile parkinsonism appears to be transmitted as an autosomal dominant or autosomal recessive trait. Initial findings may include lower limb dystonia or signs of parkinsonism, such as slowness of movement (bradykinesia), rigidity, and tremor. Additional findings may include postural instability and balance difficulties, mask-like facial expression, difficulties speaking (dysarthria), and/or other features. As with PD, reports suggest that most patients respond to therapy with L-dopa. Other Heredodegenerative Dystonias In addition to those described above, there are numerous additional disorders that are classified as heredodegenerative dystonias. These include... Other autosomal recessive disorders, such as ataxia-telangiectasia, Hallervorden-Spatz disease, and homocystinuria Certain mitochondrial disorders, such as Leigh disease Other parkinsonism disorders, including progressive supranuclear palsy (PSP) and cortical-basal degeneration (CBD) Other Movement Disorders and "Pseudodystonias" Dystonia may also occur in association with other neurologic movement disorders that are not normally classified as forms of dystonia. These may include the following: Dystonic tics, which are often classified with other tic disorders Paroxysmal dyskinesias (PD). These neurologic movement disorders are characterized by abrupt, transient episodes of excessive or disorganized (hyperkinetic or dyskinetic) movements, including any combination of chorea; relatively slow, writhing motions that appear to flow into one another (athetosis); dystonia; and/or uncontrollable flinging movements of an arm, leg, or both (ballismus). Various forms of PD have been described in which paroxysmal episodes may... o Be provoked by sudden voluntary movement or unexpected stimuli (paroxysmal kinesigenic dyskinesia [PKD]) o Occur spontaneously or be triggered or exacerbated by caffeine or alcohol consumption, stress, fatigue, or other factors (paroxysmal non-kinesigenic dyskinesia [PNKD]) o Be precipitated by prolonged exertion (paroxysmal exertion-induced dyskinesia [PED]) or sleep (paroxysmal hypnogenic dyskinesia [PHD]) Pseudodystonias There are also a number of disorders that have been described as "pseudodystonias." Such disorders may be associated with sustained muscle contractions, unusual twisting movements, and/or abnormal postures yet are not typically considered true dystonias since they occur secondary to reflex mechanisms or various other underlying abnormalities. Examples include... Juvenile rheumatoid arthritis (JRA). JRA refers to a group of inflammatory joint disorders of childhood onset resulting from inflammation of the connective tissue membranes that line the spaces between joints and bones (synovitis). These disorders are characterized by inflammation, abnormal warmth, pain, and swelling of one or more joints, potentially leading to stiffness, limitation of movements, and fixed bending or extension of involved joints in various positions or postures (contractures). Additional symptoms and findings may also be apparent. Seizures that may result in unusual, twisting, sustained postures Arnold-Chiari malformation. This refers to developmental abnormalities in which there is protrusion (herniation) of the lower cerebellum and the lowest region of the brainstem through the opening in the base of the skull (foramen magnum) into the upper spinal canal (cervical vertebral canal). In some cases, there may also be herniation of a region of the spinal cord and its surrounding membrane through an opening in the spinal column (myelomeningocele). In some cases, associated symptoms may include certain findings seen in various forms of dystonia, such as neck pain, rigidity, and/or gait abnormalities. Isaac's syndrome. This condition is characterized by progressive, generalized muscle stiffness, twitching, spasms, and "rippling waves" of muscle contraction due to excessive activity (hyperexcitability) of the end regions of nerve fibers that supply muscle fibers (motor neurons). Stiff-man syndrome. This disorder, which typically becomes apparent during middle age, is initially characterized by periodic muscle stiffness and spasms. With disease progression that may occur over months or years, spasms and stiffness gradually become persistent in muscles of the limbs and trunk. In more advanced cases, muscles of the face and those involved in swallowing and breathing may become involved. Late in the disease course, painful spasms may be precipitated by sudden noises, emotions, or attempted movement. The muscle spasms may eventually lead to joint deformities. Sandifer syndrome. This disorder of childhood is characterized by periodic tilting of the head to the side in an apparent effort to reduce stomach (gastric) contractions associated with gastroesophageal reflux--or the backward flow of stomach contents into the esophagus. Klippel-Feil syndrome (KFS). KFS is characterized by abnormal fusion of two or more bones of the spinal column in the neck (cervical vertebrae). Associated findings may include an unusually short neck, limited movements of the neck and head, and a low hairline at the back of the head. Genetic Designations for the Dystonias As mentioned throughout, several forms of dystonia have been given specific "genetic designations" (genetic nomenclature). Following is a summarized listing of such genetic dystonias and their designations: DYT1: This designation refers to the gene responsible for most cases of early-onset and limb-onset primary dystonia. Also known as Oppenheim dystonia, DYT1 dystonia is an autosomal dominant disorder with reduced penetrance and variable expressivity. The DYT1 gene, which has been mapped to chromosome 9q34.1, regulates production of the torsinA protein. DYT1 dystonia is most common among individuals of European Ashkenazi Jewish descent. (For further information, please see the section entitled "Etiology/Primary Dystonia.") DYT2: This genetic designation was reserved for a possible autosomal recessive primary dystonia. However, no such form has yet been confirmed. DYT3: This refers to the gene for a neurodegenerative, X-linked recessive disorder that may be characterized by dystonia and parkinsonism. Known as X-linked dystonia-parkinsonism or Lubag, the disorder has been reported primarily in young adult Filipino men. The DYT3 gene has been mapped to chromosome Xq13.1. (For further information, please see the section entitled " Heredodegenerative dystonia.") DYT4: This genetic designation is for an autosomal dominant primary dystonia in a multigenerational Australian family. DYT4 dystonia is primarily characterized by abductor ("whispering") spasmodic dysphonia (laryngeal dystonia). DYT5: This refers to the gene known as GTP cyclohydrolase I (GCH1), which has been mapped to chromosome 14q22.1. Mutations of the GCHI gene may result in the dystonia-plus syndrome called dopa-responsive dystonia (Segawa syndrome), which is transmitted as an autosomal dominant trait. (For further information, please see the section entitled "Dystonia-plus syndromes.") DYT6: This is for an autosomal dominant primary dystonia mapped to chromosome 8 (8p21q22). Described in 2 Mennonite families (kindreds), this form of dystonia may be of childhood- or adult-onset; initially affects limb, cranial, or neck muscles; and typically extends to involve multiple body regions. (For further information, please see the section entitled "Etiology/Primary Dystonia.") DYT7: This genetic designation is for an autosomal dominant, adult-onset, primary dystonia of the neck region (familial torticollis) that has been mapped to chromosome 18p in a German kindred. (For further information, please see the section entitled "Etiology/Primary Dystonia.") DYT8: This designation is for a neurologic movement disorder known as paroxysmal non-kinesigenic dyskinesia (PNKD) that may be inherited as an autosomal dominant trait. PNKD is characterized by sudden, transient episodes of excessive or disorganized (hyperkinetic or dyskinetic) movements that may occur spontaneously or be triggered or worsened by stress, fatigue, or other factors. Abnormal movements may include any combination of dystonia, chorea, athetosis, and/or ballismus. DYT8 has been mapped to chromosome 2q33-q35. (For further information, please see the section entitled "Other movement disorders and 'pseudodystonias.'") DYT9: This genetic designation is for a family affected by an autosomal dominant disorder known as "choreoathetosis spasticity, episodic" or CSE. It is characterized by sudden, transient (paroxysmal) attacks of dyskinesia—such as chorea, athetosis, limb dystonia, imbalance, and difficulties speaking (dysarthria)—that, in some cases, may be associated with constant weakness and stiffness of the legs (spastic paraplegia). Paroxysmal episodes may be precipitated by physical exercise, lack of sleep, alcohol consumption, stress, or other factors. DYT9 has been mapped to chromosome 1p. DYT10: This designation is for paroxysmal kinesigenic dyskinesia (PKD), a neurologic movement disorder that may be transmitted as an autosomal dominant trait. In patients with PKD, sudden episodes of dyskinesia, including dystonic movements, may be triggered by sudden voluntary movement or unexpected stimuli (startle). DYT10 has been mapped to chromosome 16p11.2-q12.1. (For further information, please see the section entitled "Other movement disorders and 'pseudodystonias.'") DYT11: This refers to an autosomal dominant disorder known as myoclonus-dystonia resulting from mutations of a gene that regulates production of the D2 dopamine receptor (DRD2) protein. Genetic analysis of a family with 8 affected members demonstrated mutations of the DRD2 gene, which has been mapped to chromosome 11q23. Evidence suggests that this may be the same disorder as hereditary essential myoclonus. (For further information, please see the section entitled "Dystonia-plus syndromes.") DYT12: This designation is for the gene responsible for rapid-onset dystonia-parkinsonism (RDP), an autosomal dominant disorder. The DYT12 gene has been mapped to chromosome 19q. (For further information, please see the section entitled "Dystonia-plus syndromes.") As mentioned earlier, investigators expect that additional genetic forms of dystonia—particularly familial primary dystonias—will be identified that may be provided with genetic designations in the future (e.g., DYT13, etc.). In addition, some experts indicate that traditional classifications of dystonia (i.e., clinical and etiologic classifications) may gradually be revised or replaced by genetic classifications as more is learned about the specific underlying genetic mechanisms of dystonia. Epidemiology Due to the variability of associated symptoms and disease severity and the fact that some patients with mild cases may remain undiagnosed, it is difficult to determine the specific frequency of primary dystonia in the general population. However, according to a 1998 study conducted in Rochester, Minnesota, the frequency was estimated to be 29.5 individuals per 100,000 for focal dystonias and 3.4 per 100,000 for generalized dystonias. As mentioned earlier, early-onset primary dystonia is most common among individuals of European Ashkenazi Jewish descent. It has been estimated that the frequency is approximately 0.5 to 4 individuals per 100,000 in the non-Jewish population, with some experts suggesting that individuals of Ashkenazi Jewish ancestry may be affected about 3 to 5 times as frequently. However, a recent investigation has reported an even higher frequency of approximately 20 to 30 individuals per 100,000 in the Ashkenazi Jewish population. Evidence indicates that the late-onset primary dystonias do not appear to have a higher frequency among those of Ashkenazi Jewish descent as compared with the non-Jewish population. There are few epidemiological studies on dystonia and its various forms. A large European study, reported in the literature in 2000, estimated the crude annual period prevalence rate for primary dystonia (for 1996-1997) at 152 per million. Of the primary dystonias, focal dystonia had the highest relative rate at 117 per million. The prevalence rates for the other dystonias were estimated as follows: 57 per million for cervical dystonia; 36 per million for blepharospasm; and 14 per million for writer's cramp. The relative rates, adjusted for age, were substantially higher in women than in men for the segmental and focal dystonias. The exception to this was writer's cramp. The authors (Warner T et al.) point out that these estimates should be viewed as "under-estimates" of the true prevalence of dystonia. Their estimates are seen as conservative due, in part, to under-ascertainment of cases. Pathophysiology No consistent or specific changes in brain tissue or function have been seen in individuals with primary dystonias, and the basic underlying defect or defects in these disorders remain unknown. However, investigators suggest that the primary dystonias as well as dystonia-plus syndromes probably result from abnormalities in the activity of chemicals in the brain known as neurotransmitters, such as an imbalance of dopamine transmission, within the basal ganglia. (As mentioned earlier, neurotransmitters are naturally produced chemicals that may transfer nerve impulses across the spaces between neurons, enabling nerve cells to communicate. The basal ganglia consist of specialized nerve cell clusters deep within the brain that organize motor behavior.) Thus, these disorders may be considered neurochemical in origin—i.e., neurochemical disorders that do not appear to result in structural neurodegenerative changes. (In contrast, heredodegenerative disorders are usually hereditary disorders in which structural neuronal degeneration may be associated with neurochemical abnormalities.) An underlying neurochemical basis for many dystonias may be suggested by multiple factors, including evidence that secondary dystonia may result from treatment with the dopamine precursor L-dopa (such as used for treatment of Parkinson's disease) or therapy with dopamine receptor blockers (antagonists). As mentioned earlier, the dystonia-plus syndromes also are nondegenerative, neurochemical disorders that are distinguished from primary dystonias due to the presence of neurologic features in addition to dystonia (e.g., myoclonus or parkinsonism). Specifically, dopa-responsive dystonia (DRD) and several DRD variants have been shown to result from reduced production of dopamine and/or other neurotransmitters in the basal ganglia. Abnormalities in the activities of certain neurotransmitters have also been demonstrated in heredodegenerative disorders (e.g., Parkinson's disease, Rett syndrome, etc.). In addition, anatomic studies of focal brain lesions associated with certain secondary dystonias and specific neurodegenerative changes found in heredodegenerative dystonias (e.g., Wilson's disease, Huntington's disease, neuroacanthocytosis, etc.) implicate dysfunction of the basal ganglia and its connections (e.g., thalamus, cerebral cortex, or, rarely, the brainstem) as a cause of such dystonias--and further support the theory that primary dystonias may result from abnormalities of the basal ganglia. Electrophysiology Electromyography (EMG) is a diagnostic test in which the electrical activity of voluntary (skeletal) muscles are measured at rest and during voluntary action. In patients with dystonia, EMG may reveal little or no activity at rest or prolonged bursts of electrical activity with overflow to muscles that are not normally involved. More specifically, abnormal EMG patterns at rest may include any of the following: Relatively long spasms that result in abnormal, sustained postures Repetitive bursts of electrical activity that are of "mid range" in length (i.e., approximately 200 to 500 milliseconds). (Note: EMG bursts usually do not last longer than approximately 100 milliseconds.) Irregular bursts or jerks that are short (i.e., less than 100 ms), resembling those associated with myoclonus. In addition, any of the above EMG patterns may also occur with voluntary movements. Patients with dystonia usually have difficulty selectively initiating movement of appropriate muscles required for certain voluntary actions and experience simultaneous contraction of antagonist muscles. In addition, there is a decrease in or loss of the active inhibition of antagonist muscles that normally occurs with voluntary contraction of agonist muscles. Some researchers suggest that this finding—i.e., decreased inhibition leading to an "overflow" of movement—may result from loss of inhibition at the level of the cerebral cortex, brainstem, and spinal cord via the basal ganglia and its pathways. (The basal ganglia cells of origin of the inhibitory pathways are under the control of the activities of the neurotransmitter dopamine.) Such a theory may potentially explain how dystonia may result from or be triggered by different mechanisms. For example, according to such a theory, significant loss of inhibition potentially leading to dystonia may result from lesions of certain areas of the brain; specific genetic abnormalities; or a genetic predisposition that may be triggered by environmental factors, such as abnormal sensory input resulting from repeated use and/or trauma of the affected body part. Concerning sensory input, there is some evidence suggesting that certain abnormalities in the brain's ability to process sensory information may also play some role in causing dystonia by altering brain motor control. According to researchers, this possibility is supported by various factors, including the "sensory tricks" seen in many patients with dystonia and the fact that some patients may develop certain sensory symptoms prior to the development of dystonia. For example, such sensory symptoms have included a gritty feeling in the eye and increased sensitivity to light (photophobia) prior to onset of blepharospasm. In addition, repeated use or peripheral trauma of a body part may result in abnormal sensory input, potentially triggering the onset of dystonia. Further research is needed to learn more about the potential causative role of loss of inhibition, sensory dysfunction, peripheral trauma, and/or other mechanisms in dystonia. Diagnosis The diagnostic evaluation of dystonia may include the following: General physical and neurologic examinations Evaluation of the nature of the dystonia, including... o Apparent age at symptom onset o Bodily distribution o Disease progression o Whether dystonia occurs with specific actions o If it is characterized by "overflow" o If it is present at rest o Whether certain "sensory tricks" temporarily suppress dystonic movements For example, the presence of hemidystonia—or rest dystonia rather than action dystonia at symptom onset—is strongly suggestive of secondary dystonia. Identification of certain features may suggest that symptoms have an emotional rather than an organic origin [psychogenic disease], such as abrupt onset, changing characteristics over time, spontaneous remissions, etc. And early limb-onset dystonia in the absence of other findings may suggest primary dystonia possibly due to DYT1 gene mutation [Oppenheim dystonia].) During clinical evaluation to assess the nature of the dystonia, patients may be examined and videotaped while performing various actions, such as sitting, standing, lying down, or walking. In addition, if the dystonia is not always present, the examiner may use various methods to help "trigger" dystonic spasms to aid in diagnosis, such as requesting that a patient with suspected blepharospasm repeatedly open and shut his or her eyes. The examiner may also conduct passive movements of the affected bodily region, carefully feel (palpate) contracting muscles, and/or request that a patient adapt various positions or postures with the affected area. Such methods may be necessary for accurate diagnosis, appropriate assessment of the nature of dystonia, and localization of involved muscles (e.g., for those who may be appropriate candidates for therapy with botulinum toxin). Such evaluation may be documented by videotaped recordings. For those patients with suspected laryngeal dystonia, voice assessment is typically documented on voice recordings. Additional evaluations may include assessment by a speech-language pathologists, when appropriate, physical or occupational therapists, or genetic counselors. A thorough patient history to help determine or exclude causative factors potentially associated with secondary dystonia, such as exposure to certain medications, particularly dopamine antagonists; exposure to certain toxins; peripheral, head, or spinal trauma; certain infections or inflammatory conditions of the brain; etc. A careful family history Laboratory studies, such as blood and urine tests, analysis of cerebrospinal fluid (CSF), and/or other studies. Blood tests may include erythrocyte sedimentation rate (ESR), antinuclear antibodies (ANA) studies, tests to detect the presence of acanthocytes or abnormal red blood cells that have spur-like projections (i.e., a finding that may be suggestive of neuroacanthocytosis), and/or other studies. (ESR measures the rate at which red blood cells settle in a tube of unclotted blood, potentially serving as a nonspecific indicator of inflammation. ANAs, which are antibodies that act against certain of the body's own cells [autoantibodies], are commonly seen in patients with certain autoimmune disorders.) If diagnosing physicians suspect certain heredodegenerative dystonias due to specific metabolic defects, laboratory studies may also be conducted to detect the levels of certain enzymes (e.g., lysosomal enzymes, etc.). In addition, particularly for children, adolescents, and adults younger than approximately age 40, studies may be recommended to measure levels of the enzyme ceruloplasmin in the fluid portion of the blood (serum). Abnormally low ceruloplasmin serum levels may suggest a diagnosis of Wilson's disease. For some patients, other laboratory studies may also be appropriate. Electrical recording techniques, such as electromyography (EMG); nerve conduction velocity tests; or other methods (e.g., reflex studies). In addition, in some instances, diagnostic evaluation may include electroretinography, which measures the retina's electrical response to light stimulation; electroencephalography (EEG) to detect or rule out potential seizure activity (such as in some individuals with paroxysmal dyskinesias); or other techniques. Biopsies. In selected patients, diagnostic assessment may include surgical removal and microscopic evaluation (biopsy) of small samples of skin, muscle, and/or nerve tissue. Ophthalmologic examination, including examination of internal structures at the front of the eyes with an illuminated microscope (slit lamp examination). Such examination may be recommended for children, adolescents, and adults under approximately age 40 to help confirm or rule out the presence of Kayser-Fleischer rings. As mentioned earlier, these are gold-like, brownishrings around the corneas of the eyes that are present in many patients with Wilson disease. They are typically present in patients who manifest neurologic and psychiatric abnormalities associated with this heredodegenerative disease. Thorough neurologic evaluations to help confirm or exclude the presence of other neurologic signs that may suggest secondary dystonias, dystonia-plus syndromes, or heredodegenerative disorders. Such neurologic signs may include certain eye (ocular) abnormalities (e.g., optic atrophy, retinal abnormalities); parkinsonism; myoclonus; impaired coordination of voluntary movements (ataxia); spasticity; muscle weakness; dementia; seizures; and/or other findings. Neuroimaging studies, such as computerized tomography (CT) scanning or magnetic resonance imaging (MRI), to create detailed, cross-sectional images of the brain and spinal cord. Such studies may be recommended for those in whom patient history and clinical examination suggest the possibility of structural lesions that may be responsible for secondary or heredodegenerative dystonias. According to experts, individuals with early-onset apparently isolated dystonia should undergo specific tests to help exclude Wilson disease (e.g., slit lamp examination, serum ceruloplasmin). If patient and family history and physical examination reveal certain symptoms, signs, and physical findings suggestive of secondary or heredodegenerative dystonias, more extensive diagnostic testing may be recommended, such as enzymatic studies (assays), neuroimaging studies, etc. For those with primary dystonias, dystonia is typically the only sign upon examination (i.e., with the possible exception of tremor or brief myoclonic jerks). In such cases, most diagnostic studies may not provide any revealing findings. However, for individuals with early-onset or limb-onset dystonia, regardless of their family history or ancestry (i.e., whether of Ashkenazi Jewish or non-Jewish descent), DNA testing is now available to help confirm or exclude primary dystonia due to mutation of the DYT1 gene. During such testing, blood samples are taken from patients and DNA is directly analyzed for the presence of the GAG (guanine, adenine, guanine) deletion in the DYT1 gene's coded instructions. In addition to confirming or ruling out DYT1 dystonia in patients with symptoms, such testing may also help to detect or exclude the DYT1 gene mutation in family members of diagnosed individuals and may be conducted prenatally. As mentioned earlier, however, evidence indicates that only 30 to 40 percent of those who carry a mutated DYT1 gene for the disease manifest symptoms (reduced penetrance). Therefore, a majority of those with the mutated gene do not develop the disorder. There currently is no way to predict whether an individual with the disease gene will develop dystonia. Because the disorder has reduced penetrance as well as variable expressivity among those who do develop symptoms, experts recommend that genetic counseling should be provided for individuals who are considering diagnostic, carrier, or prenatal DYT1 DNA testing. For patients with early-onset generalized or segmental limb dystonia who test negative for the DYT1 gene mutation, physicians may recommend a diagnostic trial with the agent levodopa (L-dopa). The dystonia-plus syndrome known as dopamine-responsive dystonia (DRD) is suggested in young patients with dystonia who have significant improvement with low-dose L-dopa therapy. In contrast, most dystonia patients who do not have DRD do not have a response to treatment with L-dopa or dopamine agonists. Thus, if no improvement is noted after approximately 3 months of L-dopa therapy, a diagnosis of DRD is considered unlikely and such treatment may be stopped. For some patients with adult-onset focal dystonias that are presumed to be primary—e.g., based upon thorough clinical examination, a complete patient and family history, nature of the dystonia, absence of certain signs upon examination, etc.—experts indicate that extensive laboratory or neuroimaging studies may not be necessary. As discussed above, if patients are under 40 years of age, they should receive specific tests to help exclude Wilson disease. In addition, the presence of certain unusual (atypical) signs may suggest the need for additional testing. For example, as mentioned previously, adult-onset lower limb dystonia is extremely rare; therefore, such patients should receive diagnostic evaluations to determine whether the condition has occurred secondary to Parkinson's disease or other parkinsonism syndromes. However, individuals with typical adult-onset focal dystonias, particularly those who have been affected for several months or more, may not require further diagnostic evaluations unless new signs or unusual symptoms develop. It is possible that DNA analysis may assist in diagnosing other forms of dystonia caused by known mutations of specific genes in certain families. However, such testing may be considered investigational and/or may not be widely available. As more is learned about the genetic causes of the different forms of dystonia, it is hoped that such information will lead to additional laboratory studies and greater availability of such testing to help confirm the diagnoses. Approaches to Treatment The first step in treatment is attempting to determine the cause of the dystonia. For secondary dystonias, treating the underlying cause may improve the dystonia. For instance, treatments for neurological conditions such as multiple sclerosis or Parkinson's disease may reduce dystonic symptoms. Withdrawing or reducing neuroleptic drugs leads to slow improvement in some cases. There are three main approaches to the treatment of dystonia: oral medications, injections of therapeutic agents directly into dystonic muscle, and surgery. Physical therapy may play a role for some patients, most often as a supplement to other therapies such as botulinum toxin. Supportive therapy provides an important adjunct to medical treatment for many patients. There are currently no known treatments that can reverse the course of primary dystonia. However, symptoms may usually be managed well with a combination of treatments. For example, patients with dopa-responsive dystonia (DRD) improve significantly with small doses of levodopa. Neurologists often try a course of levodopa therapy for patients with limb-onset dystonia in order to determine if DRD is the cause. Most patients who do not have DRD will not have a strong response to levodopa or to other dopaminergic drugs, such as dopamine agonists. Support and advocacy organizations are important resources for individuals with dystonia and their families. Newsletters, group meetings, and Internet-based discussion groups offer opportunities for sharing of information, exchanging psychological support, and becoming involved in promoting research on dystonia and its treatments. A full list of international support and advocacy groups is available here. Pharmacologic Treatment of Dystonia There are a number of treatment options available to treat dystonia. Drugs may be used alone or in combination. In addition, they may be combined with other forms of treatment. Botulinum toxin (BTX) Botulinum toxin (BTX) is a biological therapeutic agent that acts against dystonia. Botulinum toxin is a toxic protein that is produced by the bacterium Clostridium botulinum. The use of botulinum toxin (BTX) represents a significant advance in the treatment of dystonia. This toxin is known to cause botulism, a deadly form of food poisoning that is contracted through the ingestion of contaminated food products. However, when a minute amount of commercially prepared BTX is injected directly into an overactive muscle, it relaxes the muscle. BTX blocks the release of acetylcholine, a neurotransmitter responsible for activation of muscle contraction. Thus, BTX decreases inappropriate or excessive muscle contractions, allowing the affected area (e.g., arm, neck, leg, eyelid, etc.) to assume a more normal position or posture. There are seven forms (serotypes) of botulinum toxin; namely, types A, B, C, D, E, F, and G. Each serotype of has a distinct structure and mechanism of action. In the United States, only two BTX products have been approved by the U.S. Food and Drug Administration (FDA). They are BOTOX® (a BTX-A product produced by Allergan, Inc.) and Myobloc™ (a BTX-B product produced by Solstice Neurosciences). Another BTX-A product–Dysport® (Ipsen, Ltd.)–is available, but has not been approved by the FDA for use in the United States. Each BTX product is unique, with its own safety, efficacy, and immunogenicity profile. Botulinum Toxin Type A for Dystonia Injections of botulinum toxin type A have been used in the management of dystonia since the late 1980s. BOTOX® (Allergan, Inc.) was approved in the United States by the FDA in 1989 for use in patients ages 12 and above who were affected by strabismus, blepharospasm associated with dystonia, including benign essential blepharospasm–or disorders of the seventh cranial nerve. Since then, BTX-A has been used widely in the management of focal dystonia, as well as other disorders characterized by excessive muscle spasms. On December 27, 2000, the FDA approved the use of BOTOX® for the treatment of cervical dystonia (CD). Injections of this product decrease the severity of abnormal head positioning and postures as well as associated neck pain. Another botulinum toxin type A product, Dysport®, is produced and distributed by Ipsen, Ltd., but has not been approved for use within the United States. The appropriateness of BTX-A or of any dystonia therapy–relies on its ability to meet the goals of patients and caregivers as outlined in their comprehensive treatment plan. Administration of BTX-A for the treatment of dystonia A solution of BTX-A is injected directly into several sites in the overactive, dystonic muscle. These sites are near the nerve terminals or that part of the nerve cell that actually stimulates the muscle to contract. BTX-A works inside the nerve terminals to block the release of the neurotransmitter acetylcholine. This neurotransmitter serves to initiate or elicit muscle contractions. Some nerve terminals remain unaffected by BTX-A; therefore, the injected muscle may still contract but with less force. One important benefit of BTX-A is that the dose may be adjusted to provide the precise degree of weakness needed to overcome dystonia; however, some strength for normal function is preserved. BTX-A temporarily weakens dystonic muscles, thereby allowing for a more normal posture and function. The benefits that BTX-A conveys to a particular patient depend on the location and relative degree of severity of the dystonic muscles being injected. In general, BTX-A cannot be used alone to treat widespread or extremely severe generalized dystonia, as the drug dose required for this type of treatment would be too high. In these patients, BTX-A may be used to target specific dystonic muscles, thereby improving particular aspects of care and function or relieving discomfort or pain. Many patients with painful muscle spasms report a reduction in pain after injection with BTX-A. Duration of BTX-A effects The effects of treatment with BTX-A are usually greatest for a two- to six- week period following injection. In most patients treated with BTX-A (BOTOX® or Dysport®) these treatment effects typically fade approximately three to six months after injection administration. If necessary, reinjection of the drug is possible at that time. In order to decrease the possibility of antibody formation, reinjections are not administered before three months after the last injection. Side effects of BTX-A During the dose regulation process, physicians work closely with patients to optimize their therapy. Some patients may experience temporary, muscle weakness. This weakness is temporary and wears off. If patients experience muscle weakness, it is important to discuss this finding with their physicians as it may be a signal for a modification of the treatment approach. For example, muscle weakness may be lessened by reducing the dose of BTX-A during the next injection. BTX-A should be used with extreme caution in patients with neuromuscular disease such as myasthenia gravis or amyotrophic lateral sclerosis (ALS or motor neuron disease), or in those who receive therapy with drugs that thin the blood (anticoagulants), or certain antibiotics (aminoglycosides such as gentamicin [Garamycin®], kanamycin [Kantrex®], neomycin [Mycifradin®, Myciguent®, or NeoTab®], streptomycin [Streptomycin], or tobramycin [Tobrex® or Nebcin®]). The decision to combine injections of BTX-A with other forms of treatment for dystonia is an individual decision and based on many factors. This decision is reached after thorough clinical evaluation and consultation with the treating physician. In some patients receiving injections of BTX-A, the dosage of other medications may be reduced. Certain oral medications as well as baclofen, which may be delivered directly next to the spinal column (intrathecally), may provide global muscle tone reduction, whereas BTX-A injections may provide graded focal relief in selected muscles. Injection of BTX-A During the administration of BTX-A, a relatively small needle is placed into the target muscle. In large or accessible muscles, confirmation of appropriate placement of the injection into the target muscle may be achieved by feeling the muscle. In small or deep muscle groups, electromyography (EMG) or electrical stimulation may be required to confirm appropriate placement. Small muscles may be injected in only one or two sites. Larger muscles may require three to four injection sites. Most individuals are able to tolerate these small needle punctures; however, if necessary, local anesthetic cream or sedation may help ease discomfort or anxiety associated with injection. This may be particularly useful for children who are receiving injections. Antibodies and BTX therapy Antibodies are proteins produced by the immune system to help fight infections or dispose of other foreign agents that enter the body. In some individuals treated with BTX-A, antibodies may develop, bind to the drug, and inactivate it. This renders BTX ineffective in weakening muscle contractions associated with dystonia. It is estimated that approximately five percent of individuals with cervical dystonia who have been treated regularly with relatively higher doses of BTX-A develop antibodies. Once a patient forms antibodies to a particular serotype of BTX (immunoresistance), further injections of that particular serotype of BTX are typically ineffective. Physicians should, therefore, use the smallest amount of BTX-A necessary to achieve therapeutic benefit; extend the time interval between treatment sessions as long as possible (with at least three months between treatments); and, if possible, avoid the use of "booster" injections. A new, lower protein form of BOTOX® is available. It is theorized that lower protein may lead to lower rates of antibody formation (reduced immunogenicity). See E-MOVE Article: BTX-A current bulk toxin vs. original (AAN report). On occasion, a patient may not respond to therapy with BTX-A. So-called "primary non-responders" are patients who do not respond to their first injection of BTX. Secondary non-response may occur as the result of a technical problem, such as an inappropriate site of injection into the wrong muscle, a dose that is inadequate to provide a clinical effect, or disease progression. The toxin may weaken the muscle; however, the degree of relaxation may not provide symptomatic relief for the patient. In addition, some patients on combination therapies for segmental or generalized dystonias may fail to take their oral medications, leading to a general increase in symptoms (masking the local effects of BTX-A). If failure to respond continues, it is possible that the patient has antibody-mediated resistance (immunoresistance). It is important that patients work with their physicians to set appropriate treatment goals and tailor the course of treatment to meet these goals. There is no formal "recipe" that works for every patient. Each individual is unique and responds differently to BTX-A therapy. Botulinum Toxin Type B for Dystonia On December 11, 2000, a botulinum toxin type B product (Myobloc™) was approved by the FDA in the United States as a treatment for patients with cervical dystonia. Myobloc™ is the U.S. trade name for Solstice Neurosciences' botulinum toxin type B product. This product also received marketing authorization from the European Union's Committee for Proprietary Medicinal Products and is available there as Neurobloc®. Safety and efficacy were demonstrated in double-blind clinical trials in patients who had responded to BTX-A and in patients who had developed resistance to BTX-A. BTX-A and BTX-B have slightly different chemical structures and their primary mechanisms of action on acetylcholine also differ. Please refer to E-MOVE Article: BTX-B for cervical dystonia (AAN report) Please see: Toxins '99 Meeting Reports Other Medications Used to Treat Dystonia Benzodiazepines Benzodiazepines are a class of drugs that interfere with chemical activities in the nervous system and brain, serving to reduce communication between nerve cells. Consequently, such medications may relax muscles and ease symptoms associated with dystonia. Benzodiazepines are oral medications that may be used to treat focal, segmental, and generalized dystonias. Diazepam (Valium®) and clonazepam (Klonopin®) are two types of benzodiazepines that are most commonly used to treat dystonia. The major side effect of these drugs is drowsiness, which may be controlled by lowering the dose. At relatively high doses, side effects may include depression, personality changes, or, in severe cases, psychosis. Baclofen Baclofen (Lioresal®) is a drug that is used to treat individuals with spasticity. In addition, this drug has been administered to some patients with dystonia. Baclofen's primary site of action is the spinal cord where it reduces the release of neurotransmitters that stimulate muscle activity (GABA agonist stimulating GABAB autoreceptor). Baclofen has been used to treat both primary and secondary dystonias. This drug may be administered orally or via a surgically implanted pump that delivers the drug directly to the spinal cord (intrathecal baclofen). Anticholinergics Anticholinergic drugs block the action of the neurotransmitter acetylcholine, thereby deactivating muscle contractions. These drugs are administered orally and used to treat focal, segmental, and generalized dystonias. Trihexyphenidyl (Artane®) and diphenhydramine (Benadryl®) are the most common anticholinergic agents used to treat dystonia. This form of therapy may be more beneficial in children, as they are frequently able to tolerate higher doses of trihexphenidyl than adults. Greater therapeutic benefits may also occur in those patients who initiate drug therapy early during the course of their disease. Side effects may be severe, particularly at higher doses. These may include confusion, drowsiness, hallucinations, forgetfulness, personality changes, dry mouth, blurred vision, and urinary retention. Dopamine-blocking agents/Dopamine-depleting agents Dopamine-blocking or dopamine-depleting agents may be used to treat some patients with dystonia. The possible positive effect of these agents is a paradox since dopamine blockers may also cause dystonia. Nonetheless, these agents have been shown to be effective in some patients. Although not available in the United States, tetrabenazine is the most widely used dopamine-blocking agent. In some patients, tetrabenazine may be combined with lithium, which may help to lessen side effects such as slowed movements and depression. Other dopamine blockers are not as commonly used, since they may be more likely to evoke tardive dystonia. The neuroleptic drugs clozapine and olanzapine may be useful for the treatment of dystonia and may be less likely to cause tardive dystonia. See E-MOVE Article: Cervical dystonia: mixed results for clozapine. Surgical Treatment of Dystonia Thalamotomy and Pallidotomy Surgical intervention may be considered in those patients with severe dystonia who have not responded or become non-responders to drug therapy. Thalamotomy and pallidotomy, which are surgeries used to treat individuals with Parkinson's disease, are now used to treat those with dystonia. During these two forms of surgery, specific areas deep within the brain that are involved with the initiation and generation of movement are targeted for destruction. During a stereotaxic thalamotomy, a selected portion of the thalamus is surgically destroyed (ablated). The thalamus is a paired structure deep within the brain that is involved in the control of movement. In this procedure, neurosurgeons use specialized equipment, enabling them to use three-dimensional coordinates to precisely locate an area of the thalamus. Extreme care is exercised this structure is deep within the brain and located near other important structures. The possible complications of thalamotomy include contralateral weakness (hemiparesis), confusion, or dysarthria. Although these symptoms are relatively common during the postoperative period, they are usually short-lived and recede within a short period. A pallidotomy involves destruction of part of the globus pallidus (GPi), a region of the brain involved with the control of movement. Destroying part of the GPi may help to restore the balance that normal movement requires. Pallidotomy is performed by insertion of a wire probe into the GPi. Once its placement has been confirmed by electrical tests, the probe heats surrounding tissue by emission of radio waves. The heat destroys nearby tissue. This procedure does involve risk and complications occur in about 10 percent of patients. For example, the surgical probe may strike a blood vessel during insertion, causing a slight stroke. Damage to non-target brain areas is also possible. The goal of surgery for individuals with dystonia is to attempt to "rebalance" movement and posture control by destroying one or the other of these regions deep within the brain. These procedures have been performed in relatively few patients with dystonia as compared to their widespread use in those with Parkinson's disease. However, studies have shown these surgeries to be effective in most patients. Adverse effects may be considerable and include swallowing and speech difficulties as well as bleeding into the brain (cerebral hemorrhage). Deep Brain Stimulation Deep Brain Stimulation (DBS) is an invasive surgical procedure that seems to mimic the positive effects of surgical ablation performed during a thalamotomy or pallidotomy. During this procedure, electrodes are implanted in a specific area of the brain (i.e., thalamus or, more recently, globus pallidus). In addition, a device known as an implantable pulse generator (IPG) is placed under the skin in the area of the collarbone. After appropriate postoperative testing, leads from the implanted electrodes are connected to the pulse generator, which then delivers continuous high frequency electrical stimulation to the thalamus via the implanted electrodes. This form of stimulation helps the thalamus "rebalance" the control messages in the movement control centers of the brain. Patients may turn the pulse generator off and on by passing a hand-held magnet over the device. The batteries that power the pulse generator need to be surgically replaced every 3 to 5 years. Adverse events due to thalamic stimulation are generally mild. The severity of complications and side effects usually correlate with the intensity of stimulation. The possible complications of DBS include mild speech impairment (dysarthria), weakness on one or both sides of the body, or disturbance of normal balance (dysequilibrium). In most patients, unusual sensations (paresthesias) such as numbness or tingling in the head and hands may occur after surgery; however, these sensations typically resolve with ongoing adjustment of the stimulator settings. About six percent of patients experience marked speech impairment or permanent, though tolerable, paresthesias. To date, deep brain stimulation has been performed on very few patients with dystonia. Generally, moderate improvement has been reported. Several clinical centers are currently conducting studies on DBS of the pallidum in patients with dystonia. Another feasibility study is being performed in those patients with intractable dystonia. See E-MOVE Article: Surgery for Dystonia. Myectomy (Myotomy) Selective myectomy or myotomy is a surgical procedure during which a portion of an overactive muscle is removed. This procedure was a common treatment for blepharospasm; however, with the advent of botulinum toxin treatment, selective myectomies are only rarely performed. Ramisectomy and Rhizotomy Ramisectomy and rhizotomy are surgical procedures that involve the cutting of a nerve(s) that innervates an overactive muscle. These types of surgeries are rarely performed; however, they may be effective in certain, properly chosen patients. They are most commonly performed on patients with cervical dystonia who have developed resistance to BTX-A. Possible adverse effects include permanent muscle weakness as well as difficulty swallowing. See E-MOVE Article Dystonia surgery (AAN report). Peripheral Denervation During selective peripheral denervation (SPD) or the Bertrand Procedure, nerves are removed at the point where they enter the selected, hyperactive muscle. Nerve supply (innervation) to uninvolved muscles is maintained. This procedure may be an option for some patients who were not successfully treated or have not responded to toxin therapy. Other Approaches to Treatment Stretching exercises may be important for maintaining or recovering range of motion for affected joints (such as of the arms, legs, etc.). For example, a regular program of stretching exercises may assist affected individual in regaining full range of motion after a BTX injection has weakened a dystonic muscle. Some patients use so-called "sensory tricks" to temporarily relieve their symptoms. These frequently involve touching or stroking a particular spot on the skin. The exact mechanism of relief obtained by these "sensory tricks" is not understood. It is possible that skin stimulation may interrupt abnormal nerve impulses that cause muscle overactivity. In addition, in some patients, certain types of braces may provide the same stimulation and be equally effective. A number of clinical trials have studied the use of biofeedback techniques for the treatment of individuals with dystonia. Some patients have benefited; however, in most patients, no long term, clear-cut improvement has been demonstrated. Clinical trials have demonstrated that manipulation-based therapies (chiropractic, etc.) have not been effective for people with dystonia; however, some patients report that they obtain some benefit from these techniques. Practitioners are advised not to use force, but to assist their patients in using their own resources to compensate for postural abnormalities. Dystonia DYT1 Gene FAQ Summary of Nature Genetics article. Edited: June 3, 1999 (JEB) In the September 1997 issue of Nature Genetics, scientists announced the discovery of the gene responsible for most cases of early-onset dystonia, the most common form of hereditary dystonia. This type of dystonia, also known as generalized dystonia or idiopathic torsion dystonia (ITD), is a neurologic movement disorder characterized by twisting or turning movements and abnormal postures. The gene, called DYT1, encodes for a protein known as torsinA. The exact function of torsinA is not known. Frequently Asked Questions about the Discovery of the Early-onset Dystonia Gene. (These questions were answered by Dr. Mitchell F. Brin, Director Movement Disorder Center, Mount Sinai Medical Center, New York, NY, US) I am affected by dystonia, as are other members of my family. What does the discovery of the DYT1 gene mean to me? The discovery that the DYT1 gene encodes for torsinA has several important implications for those affected by early-onset dystonia. You and other members of your family may now be able to receive an accurate, direct genetic test to determine if you are a carrier of this gene. Such a test may benefit individuals who have symptoms associated with dystonia as well as those who do not have symptoms but have a relative with dystonia. For those individuals with symptoms, a positive test for the DYT1 gene may assist their neurologist in confirming the diagnosis. For relatives of affected individuals, this genetic test may provide important information as to whether or not they are also carriers of the DYT1 gene. This may help to establish their risk for developing symptoms associated with dystonia. The tendency or "predisposition" for developing any of the various types of dystonia is controlled or regulated by the interaction of many genes. Therefore, negative test results do not necessarily mean that individuals do not have another gene that may contribute to the development of dystonia. The discovery of the DYT1 gene will accelerate research into the causes of early-onset dystonia. When scientists understand more fully how defective genes work and interact to cause the symptoms of dystonia, they may be able to design treatments that directly address these problems. It is important to remember that finding the gene for a condition is only the first step in the long process of developing better treatments. However, with this information in hand, the logical direction for research into treatments becomes clearer. What is a genetic test? A genetic test is a particular kind of laboratory test, usually done on cells from the blood of the person being tested. The goal of the test is to determine the presence or absence of particular changes in the genes of the person being tested; aid in the diagnosis of a disease; or determine if a person is a carrier of a particular disease gene. A direct test looks for change(s) in the actual gene in question. This type of testing is more accurate than the linkage test, which tests for chromosome differences usually close in location to the disease gene. Until now, the only genetic test for early-onset dystonia was a linkage test. A direct test is now possible for one form of early-onset dystonia associated with the DYT1 gene. What are genes? Genes are long molecules composed of the chemical DNA and are found in the nucleus of each cell. Genes perform two important functions. Firstly, each gene is the recipe, blueprint, or code for building a particular protein within the cell. Because proteins do all their work inside a cell, a mistake in the blueprint for any one of these proteins may have serious consequences for the functioning of that cell. Early-onset dystonia is caused by a mistake in the gene that contains the code for the protein called torsinA. The exact role of torsinA in brain cells is not known. Secondly, genes are the material of inheritance–copied and passed from parent to child–they ensure that offspring arise from a combined set of blueprints from the parents. Genes are linked together to form even longer structures known as chromosomes. Almost every human cell contains exactly 46 chromosomes or 23 pairs. Each chromosome comprises hundreds or thousands of genes strung together. The DYT1 gene is located on the long arm of chromosome 9 (9q34). What is a genetic disorder? A genetic disorder is a condition that occurs as the result of mistakes or changes in the code or of a gene. These changes, called new mutations, occur before conception during sperm or egg production. When this mutation occurs, the parent is not affected by the disorder; however, the child who receives the genes in that sperm or egg may be affected. As the developing fetus grows, the mutated or altered gene is usually copied exactly (i.e., in its mutated or changed form). Therefore, each cell in the body carries the mutated gene. This includes the sperm or egg cells produced by this individual. This means that this individual may pass on the gene to his or her children. A disorder that occurs as the result of a mutated gene that can be "transmitted" is occasionally called a heritable disorder. Early-onset dystonia is one type of heritable dystonia. What is the DYT1 mutation and how did it arise? The DYT1 mutation that causes early-onset dystonia is a deletion of three nucleotides, called GAG. Nucleotides are the molecular building blocks of DNA. This relatively minute change in the torsinA blueprint apparently causes critical changes in the function of the protein, and in some cases, ultimately leads to the symptoms of dystonia. Therefore, individuals who have this mutation are carriers of the DYT1 GAG deletion. Most cases of early-onset dystonia are not due to new mutations, but rather to accurate or "faithful" copying and inheritance of a gene mutation that occurred many generations in the past. Many cases of this type of dystonia are found among the Ashkenazi Jewish population (Jews who trace their ancestry back to Central and Eastern Europe). In addition, non-Ashkenazic individuals with the disorder carry the same mutation. This mutation is also seen in non-Ashkenazic Caucasians, African Americans, Asians, and other populations. What are the other types of heritable dystonia? There are other types of heritable dystonia, each of which is distinguished by the gene responsible for the disorder. For example, the gene for dopa-responsive dystonia (DRD) has been identified and well characterized. The gene locations for several other dystonias have also been determined, including that for X-linked parkinsonism on the X chromosome. Another disease gene located on chromosome 8 codes for a type of dystonia observed predominantly in the Amish and Mennonite populations. Other genetic forms of dystonia are summarized in the table Dystonia: Molecular Classification. If a gene test is negative, it is possible that another genetic form is present but not the one tested. Do both parents need to pass on the gene mutation in order for a child to develop dystonia? No, not usually. Early-onset dystonia is known as a dominant disorder. This means that only one copy of the abnormal gene is needed in order for an individual to inherit the potential to show symptoms. Some other genetic disorders, but not heritable dystonias (except for rare cases of DRD) are termed recessive. This means that two abnormal copies of the abnormal gene are needed before a person develops the disorder. Early-onset dystonia is also an autosomal disorder, meaning the gene is not carried on the chromosomes that determine an individual gender or sex (i.e., the X or Y chromosomes). Consequently, individuals of both sexes may develop the disorder and either parent may pass on the gene to their offspring. In contrast, an X-linked recessive gene is more likely to be expressed in males. X-linked dominant genes are usually lethal in males. If I have a mutation in my DYT1 gene, does that mean that I will get dystonia? It is possible that you will get dystonia, but not necessarily. For reasons scientists do not yet understand, only 30 to 40% of those with the abnormal DYT1 gene develop dystonia. There is no way yet to predict whether a person with the abnormal gene will develop symptoms of the disorder. Should I be tested for the dystonia gene? The decision to get a genetic test is a personal decision and one that should not be made lightly. You may want to consider these factors while making your decision: Do you have symptoms of dystonia? Individuals who already have symptoms of dystonia, but who have not yet been definitively diagnosed, may benefit from genetic testing. A positive result may allow their physician to make a definitive diagnosis and allow individuals with dystonia to finally identify a cause of their symptoms. A negative test result does not mean that you do not have an inherited form of dystonia. It simply means that you do not carry the DYT1 gene abnormality. Does a family member have early-onset dystonia? If another member of your family has early-onset dystonia, you have probably asked yourself whether you will also develop symptoms. Your test results may provide you with the additional knowledge. A positive result only means that you may develop symptoms and most individuals who have the gene do not develop the symptoms of dystonia. Moreover, a negative result does not necessarily mean that you are "dystonia free." There are other forms of inherited dystonia. Are there professionals who can help me understand the issues that are involved in genetic testing? A genetic counselor is a person trained in both the science and the psychological issues involved in genetic testing. A genetic counselor can help you explore the benefits and downsides of getting tested, as well as help you understand what the results mean and do not mean. If you are thinking of undergoing a genetic test, you should plan to talk with a genetic counselor. In fact, most centers that do genetic testing require consultation with a genetic counselor before the test is performed. These centers have genetic counselors who are available for appointments. Where can I get a genetic test if I want one? Genetic testing is available at a number of laboratories. The Movement Disorders Program at Mount Sinai Medical Center in New York City sends its patients blood samples to the Massachusetts General Neurogenetics DNA Diagnostic Laboratory in Boston, MA. The telephone number for the laboratory is (617) 726-5721. For a listing of genetic counselors in your area, contact: National Society of Genetic Counselors (NSGC) www.nsgc.org For additional information on a variety of genetic issues, contact: The Genetic Alliance www.geneticalliance.org References Almasy L, Bressman SB, Raymond D, Kramer PL, Greene PE, Heiman GA, Ford B, Yount J, de Leon D, Chouinard S, Saunders-Pullman R, Brin MF, Kapoor RP, Jones AC, Shen H, Fahn S, Risch NJ, Nygaard TG (1997) Idiopathic torsion dystonia linked to chromosome 8 in two Mennonite families. Ann.Neurol. 42:670-673 Auburger G, Ratzlaff T, Lunkes A, Nelles HW, Leube B, Binkofski F, Kugel H, Heindel W, Seitz R, Benecke R, Witte OW, Voit T (1996) A gene for autosomal dominant paroxysmal choreoathetosis/spasticity (CSE) maps to the vicinity of a potassium channel gene cluster on chromosome 1p, probably within 2 cM between D1S443 and D1S197. Genomics 31:90-94 Bentivoglio AR, Del Grosso N, Albanese A, Cassetta E, Tonali P, Frontali M. Non-DYT1 dystonia in a large Italian family. J Neurol Neurosurg Psychiatry. 1997;62:357-360. Brashear A, Butler IJ, Ozelius LJ, et al. Rapid-onset dystonia-parkinsonism: a report of clinical, biochemical, and genetic studies in two families. In: Fahn S, Marsden CD, DeLong M, eds. Dystonia 3: Advances in Neurology, Vol. 78. Philadelphia, Pa: Lippincott-Raven Publishers; 1998:335-339. Brashear, A., deLeon, D., Bressman, S. B., Thyagarajan, D., Farlow, M. R., and Dobyns, W. B. Rapid-onset dystonia-parkinsonism in a second family. Neurology 48(4), 1066-1069. 1997. (GENERIC) Ref Type: Journal (Full) Bressman SB, de Leon D, Kramer PL, et al. Dystonia in Ashkenazi Jews: clinical characterization of a founder mutation. Published erratum appears in Ann Neurol. 1995;37:140. Ann Neurol. 1994;36:771-777. Bressman SB, Heiman GA, Nygaard TG, et al. A study of idiopathic torsion dystonia in a non-Jewish family: evidence for genetic heterogeneity. Neurology. 1994;44:283-287. Bressman SB, Warner TT, Almasy L, et al. Exclusion of the DYT1 locus in familial torticollis. Ann Neurol. 1996;40:681-684. Brin MF, Blitzer A, Fahn S, Gould W, Lovelace RE. Adductor laryngeal dystonia (spastic dysphonia): treatment with local injections of botulinum toxin (Botox). Mov Disord. 1989;4:287-296. Crossman AR, Brotchie JM. Pathophysiology of dystonia. In: Fahn S, Marsden CD, DeLong M, eds. Dystonia 3: Advances in Neurology, Vol. 78. Philadelphia, Pa: Lippincott-Raven Publishers; 1998:19-25. Dedo HH, Izdebski K. Intermediate results of 306 recurrent laryngeal nerve sections for spastic dysphonia. Laryngoscope. 1983;93:9-16. Dobyns WB, Ozelius LJ, Kramer PL, et al. Rapid-onset dystonia-parkinsonism. Neurology. 1993;43: 2596-2602. Fahn S, Bressman SB. Dystonia. In: Rowland, LP, ed. Merritt's Neurology. 10th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2000:669-677. Fahn S, Bressman SB, Marsden CD. Classification of dystonia. In: Fahn S, Marsden CD, DeLong M, eds. Dystonia 3: Advances in Neurology, Vol. 78. Philadelphia, Pa: Lippincott-Raven Publishers; 1998:1-10. Fahn S, Greene PE, Ford B, Bressman SB, eds. Handbook of Movement Disorders. Philadelphia, Pa: Blackwell Science, Current Medicine, Inc.; 1998:51-71, 81-82, 128. Fink JK, Rainer S, Wilkowski J, Jones SM, Kume A, Hedera P, Albin R, Mathay J, Girbach L, Varvil T, Otterud B, Leppert M (1996) Paroxysmal dystonic choreoathetosis: tight linkage to chromosome 2q. Am.J.Hum.Genet. 59:140-145 Fletcher NA, Harding AE, Marsden CD. The relationship between trauma and idiopathic torsion dystonia. J Neurol Neurosurg Psychiatry. 1991;54:713-717. Ford B, Greene PE, Louis ED, et al. Intrathecal baclofen in the treatment of dystonia. In: Fahn S, Marsden CD, DeLong M, eds. Dystonia 3: Advances in Neurology, Vol. 78. Philadelphia, Pa: Lippincott-Raven Publishers; 1998:199-210. Fouad GT, Servidei S, Durcan S, Bertini E, Ptacek LJ (1996) A gene for familial paroxysmal dyskinesia (FPD1) maps to chromosome 2q. Am.J.Hum.Genet. 59:135-139 Furukawa Y, Lang AE, Trugman JM, et al. Gender-related penetrance and de novo GTP-cyclohydrolase I gene mutations in dopa-responsive dystonia. Neurology. 1998;50:1015-1020. Gasser T, Bereznai B, Muller B, Pruszak-Seel R, Damrich R, Deuschl G, Oertel WH (1996) Linkage studies in alcohol-responsive myoclonic dystonia. Mov.Disord. 11:363-370 Gasser T. Inherited myoclonus-dystonia syndrome. In: Fahn S, Marsden CD, DeLong M, eds. Dystonia 3: Advances in Neurology, Vol. 78. Philadelphia, Pa: Lippincott-Raven Publishers; 1998:325-334. Gimenez-Roldan S, Lopez-Fraile IP, Esteban A (1976) Dystonia in Spain: study of a Gypsy family and general survey. Adv.Neurol. 14:125-136 Goetz CG, Penn RD, Tanner CM. Efficacy of cervical cord stimulation in dystonia. Adv Neurol. 1988;50:645-649. Greene P. Baclofen in the treatment of dystonia. Clin Neuropharmacol. 1992;15:276-288. Haberhausen G, Schmitt I, Köhler A, Peters U, Rider S, Chelly J, Terwilliger JD, Monaco AP, Müller U (1995) Assignment of the dystonia-parkinsonism syndrome locus, DYT3, to a small region within a 1.8-Mb YAC contig of Xq13.1. Am.J.Hum.Genet. 57:644-650 Hallett M. Physiology of dystonia. In: Fahn S, Marsden CD, DeLong M, eds. Dystonia 3: Advances in Neurology, Vol. 78. Philadelphia, Pa: Lippincott-Raven Publishers; 1998:11-18. Holmgren G, Ozelius L, Forsgren L, et al. Adult onset idiopathic torsion dystonia is excluded from the DYT1 region (9q34) in a Swedish family. J Neurol Neurosurg Psychiatry. 1995;59:178-181. Ichinose H, Ohye T, Takahashi E, Seki N, Hori T, Segawa M, Nomura Y, Endo K, Tanaka H, Tsuji S, Fujita K, Nagatsu T (1994) Hereditary progressive dystonia with marked diurnal fluctuation caused by mutations in the GTP cyclohydolase I gene. Nat.Genet. 8:236-242 Iliceto G, Thompson PD, Day BL, Rothwell JC, Lees AJ, Marsden CD. Diaphragmatic flutter, the moving umbilicus syndrome, and "belly dancer's" dyskinesia. Mov Disord. 1990;5:15-22. Ishikawa A, Miyatake T (1995) A family with hereditary juvenile dystonia-parkinsonism. Mov.Disord. 10:482-488 Jankovic J. Medical therapy and botulinum toxin in dystonia. In: Fahn S, Marsden CD, DeLong M, eds. Dystonia 3: Advances in Neurology, Vol. 78. Philadelphia, Pa: Lippincott-Raven Publishers; 1998:169-183. Jun AS, Brown MD, Wallace DC (1994) A mitochondrial DNA mutation at np 14459 of the ND6 gene associated with maternally inherited Leber's Hereditary Optic Neuropathy and dystonia. Proc.Natl.Acad.Sci.U.S.A. 91:6206-6210 Kandil MR, Tohamy SA, Fattah MA, Ahmed HN, Farwiez HM (1994) Prevalence of chorea, dystonia and athetosis in Assiut, Egypt: a clinical and epidemiological study. Neuroepidemiology. 13:202-210 Kertesz A (1967) Paroxysmal kinesigenic choreoathetosis. An entity within the paroxysmal choreoathetosis syndrome. Description of 10 cases, including 1 autopsied. Neurology 17:680-690 Klein C, Brin MF, Kramer P, et al. Association of a missense change in the D2 dopamine receptor with myoclonus dystonia. Proc Natl Acad Sci U S A. 1999;96:5173-5176. Klein C, Kann M, Kis B, et al. Genetics of dystonia. Nervenarzt. 2000;71:431-441. Kramer PL, de Leon D, Ozelius L, et al. Dystonia gene in Ashkenazi Jewish population is located on chromosome 9q32-34. Ann Neurol. 1990;27:114-120. Kramer PL, Heiman GA, Gasser T, et al. The DYT1 gene on 9q34 is responsible for most cases of early limb-onset idiopathic torsion dystonia in non-Jews. Am J Hum Genet. 1994;55:468-475. Lance JW (1963) Sporadic and familial varieties of tonic seizures. J.Neurol.Neurosurg.Psychiatry 26:51-59 Lee LV, Kupke KG, Caballar-Gonzaga F, Hebron-Ortiz M, Muller U. The phenotype of the X-linked dystonia-parkinsonism syndrome. An assessment of 42 cases in the Philippines. Medicine (Baltimore). 1991;70:179-187. Leube B, Rudnicki D, Ratzlaff T, Kessler KR, Benecke R, Auburger G. Idiopathic torsion dystonia: assignment of a gene to chromosome 18p in a German family with adult onset, autosomal dominant inheritance and purely focal distribution. Hum Mol Genet. 1996;5:1673-1677. Novotny EJ, Jr., Singh G, Wallace DC, Dorfman LJ, Louis A, Sogg RL, Steinman L (1986) Leber's disease and dystonia: a mitochondrial disease. Neurology 36:1053-1060 Nutt JG, Muenter MD, Aronson A, Kurland LT, Melton LJ 3d. Epidemiology of focal and generalized dystonia in Rochester, Minnesota. Mov Disord. 1988;3:188-194. Online Mendelian Inheritance in Man (OMIM)™. National Center for Biotechnology Information Web site. John Hopkins University; McKusick VA, ed. 121800: Torsion dystonia 1, autosomal dominant; DYT1. Available at: http://www.ncbi.nlm.nih.gov/htbin-post/Omim/dispmim?121800. Last edit date August 8, 2000. Online Mendelian Inheritance in Man (OMIM)™. National Center for Biotechnology Information Web site. John Hopkins University; McKusick VA, ed. 314250: Dystonia 3, torsion, x-linked; DYT3; alternative titles: Torsion dystonia-parkinsonism, Filipino type. Available at: http://www.ncbi.nlm.nih.gov/htbin-post/Omim/dispmim?314250. Last edit date May 16, 1998. Online Mendelian Inheritance in Man (OMIM)™. National Center for Biotechnology Information Web site. John Hopkins University; McKusick VA, ed. 128230: Dystonia, progressive, with diurnal variation; alternative titles: Segawa syndrome, DYT5, Dopa-responsive dystonia (DRD). Available at: http://www.ncbi.nlm.nih.gov/htbin-post/Omim/dispmim?128230. Last edit date May 26, 1999. Online Mendelian Inheritance in Man (OMIM)™. National Center for Biotechnology Information Web site. John Hopkins University; McKusick VA, ed. 159900: Myoclonus, hereditary essential; alternative title: DYT11. Available at: http://www.ncbi.nlm.nih.gov/htbin-post/Omim/dispmim?159900. Last edit date March 16, 2000. Online Mendelian Inheritance in Man (OMIM)™. National Center for Biotechnology Information Web site. John Hopkins University; McKusick VA, ed. 128235: Dystonia 12; DYT12. Available at: http://www.ncbi.nlm.nih.gov/htbin-post/Omim/dispmim?128235. Last edit date October 2, 2000. Ozelius L, Kramer PL, Moskowitz CB, et al. Human gene for torsion dystonia located on chromosome 9q32-34. Neuron. 1989;2:1427-1434. Ozelius LJ, Hewett JW, Page CE, Bressman SB, Kramer PL, Shalish C, deLeon D, Brin MF, Raymond D, Corey DP, Fahn S, Risch NJ, Buckler AJ, Gusella JF, Breakefield XO (1997) The early-onset torsion dystonia gene (DYT1) encodes an ATP binding protein. Nat.Gen. Parker N (1985) Hereditary whispering dysphonia. J Neurol Neurosurg.Psychiatry 48:218-224 Raskind WH, Bolin T, Wolff J, Fink J, Matsushita M, Litt M, Lipe H, Bird TD (1998) Further localization of a gene for paroxysmal dystonic choreoathetosis to a 5-cM region on chromosome 2q34. Hum.Genet. 102:93-97 Risch N, de Leon D, Ozelius L, et al. Genetic analysis of idiopathic torsion dystonia in Ashkenazi Jews and their recent descent from a small founder population. Nat Genet. 1995;9:152-159. Robertson-Hoffman DE, Mark MH, Sage JI. Isolated lingual/palatal dystonia. Mov Disord. 1991;6:177-179. Smith LA, Heersema PH (1941) Periodic dystonia. Mayo Clin.Proc. 16:842-846 Vitek JL, Zhang J, Evatt M, et al. GPi pallidotomy for dystonia: clinical outcome and neuronal activity. In: Fahn S, Marsden CD, DeLong M, eds. Dystonia 3: Advances in Neurology, Vol. 78. Philadelphia, Pa: Lippincott-Raven Publishers; 1998:211-219. Walker ES (1981) Familial paroxysmal dystonic choreoathetosis: a neurologic disorder simulating psychiatric illness. Johns.Hopkins.Med.J. 148:108-113 Warner T, Camfield L, Marsden CD, et al. A prevalence study of primary dystonia in eight European countries. J Neurology 2000;247(10):787-792. Watts RL, Koller WC, eds. Movement Disorders: Neurologic Principles and Practice. New York, NY: McGraw-Hill Companies, Inc.; 1997:4-5, 419-475.