Many cases presented for evaluation of vague symptoms end up
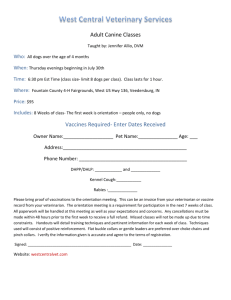
advertisement

Could it be Addison’s? Linda E. Luther, DVM, DACVIM (SAIM) Small Animal Track 2012 ISVMA Annual Conference Proceeding Many cases presented for evaluation of vague symptoms end up having hypoadrenocorticism. Can you spot the classic cases? Can you spot the not-so-classic cases? Hypoadrenocorticism, or “Addison’s” disease, results from atrophy of the adrenal cortex, and often presents as a diagnostic challenge. Clinical signs can vary from subtle signs to acute collapse, and the clinical course is often waxing and waning. Untreated collapsed dogs may die, so identifying dogs affected with this disease early is optimal. Types of hypoadrenocorticism include the ‘classic’ glucocorticoid & mineralocorticoid deficient patient, and the more subtle, glucocorticoid deficient patient. Clinical signs of classic hypoadrenocorticism may include vomiting, diarrhea, lethargy, collapse, bradycardia, abdominal pain, polyuria, polydipsia, or being “just not right”. Physical examination findings are often nonspecific. Laboratory findings in a classic case may include hyponatremia, hyperkalemia, decreased Na/K ratio, azotemia (with or without an inappropriate specific gravity), hypoalbuminemia, hypoglycemia, hypercalcemia, nonregenerative anemia. The lack of a stress leukogram is common; a normal to elevated lymphocyte count, and normal to elevated eosinophil count in a sick dog are frequent, subtle findings. ECG findings in hyperkalemic dogs can include bradycardia, a prolonged P-R interval, a lack of P waves, spiked T waves and wide, bizarre QRS complexes. THE NOT-SO-CLASSIC CASE WILL OFTEN PRESENT WITH MORE SUBTLE CLINICAL SIGNS. They will have normal electrolytes, and will often have a lack of a stress leukogram. They may also have a low normal hematocrit or a non-regenerative anemia, a low to borderline albumin, hypoglycemia and hypercalcemia. These cases are commonly missed. How can you ensure that you spot these? Look at the CBC carefully. Is there a stress leukogram? Look at the albumin level. Is it decreased or in the low normal range? Consider the history. Consider the lack of other obvious disease, and don’t forget to IGNORE the normal electrolytes. If there are enough consistent findings in a dog with vague symptoms, test for hypoadrenocorticism! Once you suspect hypoadrenocorticism, confirmation historically has been done with an ACTH stimulation test. However, a recent study showed that if a dog had a baseline cortisol level that was greater than 2.0 ug/dL, he was very unlikely to have hypoadrenocorticism. If the baseline cortisol is less than 2.0 ug/dL, hypoadrenocorticism is not ruled out, and an ACTH stimulation test should be done. But I thought she was in renal failure… Cases of hypoadrenocorticism can mimic acute renal failure in that clinical signs are similar, and azotemia with an inappropriate urine specific gravity may exist. How does the astute clinician differentiate the two? Questions to ask include: Is there a stress leukogram? Was the resolution of severe azotemia very rapid? Did the patient act like a ‘brand-new dog’ after just a day of fluids? Let’s compare “Maggie”, a 7-year-old Fs Collie that presented with vomiting and lethargy, to “Bailey”, a 12-yr-old Mn Cocker that presented in lateral recumbancy (see Table 1). Both dogs had severe azotemia with an inappropriate urine specific gravity. “Maggie” lacked a stress leukogram. The electrolyte findings in both dogs were suggestive of hypoadrenocorticism, but this finding is not pathognomonic for the disease. “Maggie” turned out to have hypoadrenocorticism. “Bailey”, did not, and he was diagnosed with renal failure (see Table 3). Because “Maggie” had an abnormal ACTH stimulation test as well as abnormal electrolytes, she had glucocorticoid and mineralocorticoid deficient hypoadrenocorticism. Therapy for “Maggie” started with intravenous fluid therapy. The hyperkalemia was treated with the fluids, as well as intravenous sodium bicarbonate therapy (1 mEq/kg, slow IV). Glucocorticoids were given, initially using dexamethasone sodium phosphate (0.1-2 mg/kg IV). Chronic glucocorticoid therapy with physiologic dose of prednisone (0.1-0.2 mg/kg/day, doubled when she was stressed) was initiated. She was also given mineralocorticoid therapy using Percorten®-V (Desoxycorticosterone pivalate or DOCP, 2.2 mg/kg IM or SQ q. 25 initially). Florinef ® (fludrocortisone acetate, 0.01-0.02 mg/kg/day initially), a mineralocorticoid which also has glucocorticoid effects, could have been used instead of Percorten®. Could he be an Addisonian? Some Addisonian dogs have very subtle symptoms. “Max” is a 7-yr-old Mn Labrador retriever that presented for a blood panel to monitor carprofen therapy that was being chronically administered to treat degenerative joint disease (see Table 2). “Max’s” blood panel revealed a significant, nonregenerative anemia. Upon further questioning, the owner thought that “Max” had been quieter lately. He was really not all that sick though. Besides the anemia, the blood work showed a lack of a stress leukogram, his electrolytes were normal, and there was no azotemia. An ACTH stimulation test was done (see Table 3), and “Max” indeed was an Addisonian! Since “Max” had normal electrolytes, he had glucocorticoid deficient hypoadrenocorticism, and he was not mineralocorticoid deficient. Chronic glucocorticoid therapy with a physiologic dose of prednisone (0.1-0.2 mg/kg/day, doubled when he was stressed), was started. Mineralocorticoid therapy was not indicated in this dog. Some glucocorticoid deficient cases eventually develop mineralocorticoid deficiency, thus periodic monitoring of electrolytes is indicated. In summary, hypoadrenocorticism can be a challenging disease to diagnose. Suspicion of the disease in dogs with vague symptoms is recommended, even in dogs that have normal electrolytes. Disclaimer: Please verify all drug dosages before administering. References: Scott-Moncrieff JCR. Hypoadrenocorticism. In Ettinger SJ, Feldman EC (eds.) Textbook of Veterinary Internal Medicine, 7th ed. Saunders Elsevier, St. Louis, 2010, 1847-1857. Lennon EM, Boyce TE, Hutchins RG et al. Use of basal serum or plasma cortisol concentrations to rule out a diagnosis of hypoadrenocorticism in dogs: 123 cases (20002005). J Am Vet Med Assoc 2007;231:413-416. Thompson AL, Scott-Moncrieff JC, Anderson JD. Comparison of classic hypoadrenocorticism with glucocorticoid-deficient hypoadrenocorticism in dogs: 46 cases (1985-2005). J Am Vet Med Assoc 2007;230:1190-1194. Table 1. “Maggie” “Bailey” White blood cells, #/μL Neutrophils, #/μL Lymphocytes, #/μL Monocytes, #/μL Eosinophils, #/μL Platelets, # x 103/μL BUN, mg/dL Creatinine, mg/dL Calcium, mg/dL Phosphorus, mg/dL Na, mmol/L K, mmol/L Cl, mmol/L Na/K Urine specific gravity 12,880 7,670 2,710 1,550 890 299 130 7.7 13.8 14.6 136 9.0 103 15.1 1.015 28,290 24,750 490 2,370 520 431 130 7.7 5.5 16.1 145 9.0 111 16.1 1.015 Table 2. “Max” Hematocrit, % White blood cells, #/μL Neutrophils, #/μL Lymphocytes, #/μL Monocytes, #/μL Eosinophils, #/μL Platelets, # x 103/μL BUN, mg/dL Creatinine, mg/dL Albumin, mg/dL Na, mmol/L K, mmol/L Cl, mmol/L Na/K 23.6 2,500 1,840 340 110 190 325 35 1.3 1.2 152 5.5 123 27.6 Table 3. “Maggie” Normal values 5,500-16,900 2,000-12,000 500-4,900 300-2,000 100-1,490 175-500 7-27 0.5-1.8 7.9-12 2.5-6.8 144-160 3.5-5.8 109-122 < 27 Normal values 37-55 5,500-16,900 2,000-12,000 500-4,900 300-2,000 100-1,490 175-500 7-27 0.5-1.8 2.3-4 144-160 3.5-5.8 109-122 < 27 “Bailey” “Max” Normal values Pre-ACTH cortisol, ug/dL < 0.5 8.0 < 0.5 > 2.0 Post-ACTH cortisol, ug/dL < 0.5 N/A < 0.5 > 8.0 * Note that “Bailey’s” baseline cortisol adequately ruled out hypoadrenocorticism. “Maggie” and “Max” had baseline cortisol values < 2.0 ug/dL, thus an ACTH stimulation was needed to confirm the disease. Quiz: Hypoadrenocorticism 1. What electrolyte changes are expected in a glucocorticoid-deficient Addisonian? E. Normal Na, normal K 2. Which describes a stress leukogram? 3. When would a baseline cortisol level rule out hypoadrenocorticism? A. When it is > 10 ug/dL B. When it is < 10 ug/dL C. When it is > 2.0 ug/dL D. When it is < 2.0 ug/dL E. Never 4. What ECG findings may be seen with hyperkalemia? (Select all correct replies) A. Bradycardia B. Tachycardia C. Spiked p waves D. Spiked t waves E. Wide bizarre QRS complexes 5. What is a physiologic dose of prednisone in a dog? A. 0.1-0.2 mg/kg/day B. 0.5-1 mg/kg/day C. 2-4 mg/kg/day D. 10 mg/kg/day