Running Head: MINORITY CHILDREN AND PES
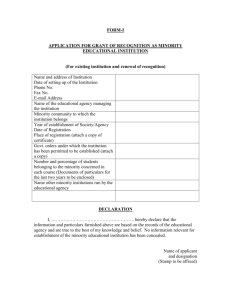
advertisement

Ethnic Minority Children Running Head: MINORITY CHILDREN AND PES Ethnic Minority Children's Use of Psychiatric Emergency Care In California's Public Mental Health System Lonnie R. Snowden Ph.D. Mary C. Masland Ph.D. Kya Fawley MSW Anne M. Libby Ph.D. Neal Wallace Ph.D. Drs. Snowden and Masland and Ms. Fawley are with the Center for Mental Health Services Research, School of Social Welfare, University of California, Berkeley. Dr. Libby is with the School of Medicine, Departments of Pediatrics and Psychiatry, University of Colorado. Dr. Wallace with the Mark O. Hatfield School of Government, Portland State University. Supported by National Institute of Mental Health award R01 MH067871. Address correspondence to Lonnie R. Snowden, 120 Haviland Hall, University of California, Berkeley, CA, 94720-7400. email: snowden@berkeley.edu. 1 Ethnic Minority Children 2 Abstract This study used fixed-effects regression for a controlled assessment of ethnic disparities in children and youth’s use of hospital-based services for the most serious mental health crises (‘crisis stabilization services”) and community-based services for other crises (“crisis intervention services”). The sample consisted of Medicaid claims for 351,174 African American, Asian American, Latino, Native American and White children and youth who received specialty mental health care from California’s 57 county public mental health systems between July 1998 and June 2001. African American children and youth were more likely than Whites to use both kinds of crisis care and made more visits to hospital-based crisis stabilization services after initial use. Asian and Native American children and youth were more likely than Whites to use hospital-based crisis stabilization services but, along with Latinos, made fewer hospital-based crisis stabilization visits after an initial visit. African American children and youth use both kinds of crisis services more than Whites and Asians and Native Americans make episodic crisis visits only when experiencing the most disruptive and troubling kind of crisis. Ethnic Minority Children 3 Ethnic Minority Children's Use of Psychiatric Emergency Care In California's Public Mental Health System While research on ethnic and cultural disparities in children and youth’s mental health treatment has grown and become ever more rigorous (Kataoka, Zhang & Wells, 2002; Yeh, McCabe, Hurlburt, Hough, Hazen, Culver et al., 2002), little attention has been paid to services that attempt to stabilize children and youth in crisis. If it occurs, excess minority use of emergency care is important to document and understand because emergency services do not promote monitoring of troubling conditions, access to all necessary treatments, or continuity of care (U.S. Department of Health and Human Services, 2001, p. 68). Minority youth are at increased risk for factors that lead to psychiatric emergency services use. Adversity increases youth’s chances of experiencing a crisis (Joffe, Offord, & Boyle, 1988; Morano, Cisler, & Lemerond 1993) and minority youth are more likely to face adversity of certain kinds: Socioeconomic disadvantage (U.S. Department of Health and Human Services, 2001), residence in poverty neighborhoods (Brody et al., 2003), racism (Clark, Anderson, Clark, & Williams, 1999), acculturative stress (Hovey & King, 1996), and care by distressed and pressured family members (Repetti, Taylor, & Seeman, 2002). Moreover, minority children and youth are underrepresented in alternative sources of specialized mental health assistance that might avert a crisis, including outpatient treatment (Buda and Tsuang, 1990; Schwab-Stone et al., 1995). These factors contribute to suicidal ideation and suicide attempts, which are the most frequent reason children and youth use emergency services (Halamandaris & Anderson, 1999; Breslow, Erickson, & Cavanaugh, 2000). Rates of suicidal behavior are higher among Latino, Asian, and Native American than among White children and youth. Among African Americans, suicide-related problems occur at a lower but increasing rate. Ethnic Minority Children 4 (Joe & Marcus, 2003). The limited research available to date indicates that minority children and youth are increasingly using emergency services (Blitz, Solomon, & Feinberg, 2001) but the evidence is mixed as to whether they are over represented. Along with sample size and statistical power differentials, differences between treatment programs, services, and systems might explain discrepant findings. To resolve this uncertainty the present study examined ethnic disparities in psychiatric emergency services (PES) use in a large, ethnically diverse, multiyear sample, of children and youth participants in California’s public mental health care services system. Services were funded by Medi-Cal, California’s version of the Medicaid insurance program for the poor (incomes below $19,350 for a family of four in 2005, American Academy of Pediatrics, 2005). Under Medi-Cal, children and youth’s psychiatric emergency services are divided into two categories, crisis stabilization and crisis intervention. Crisis stabilization services are based in a 24-hour facility, usually a hospital; they are designed for the most serious crises and aim to alleviate the need for inpatient care. Crisis intervention services are provided in the community, include assessment, evaluation, collateral care, and therapy, and are for clients needing urgent assistance but whose crisis is not severe enough to warrant removal from the community. We hypothesized that minority children and youth and would be more likely than Whites to use crisis stabilization and crisis intervention services initially, and that they would use them more frequently after initial use. We expected greater minority children and youth’s crisis services use because of the greater stress facing minorities and their lesser access to nonemergency care. Ethnic Minority Children 5 Methods Participants and Procedures We obtained Medi-Cal paid claims for mental health services delivered to youth under age 18, between July 1, 1998 and June 30, 2001, from the California Department of Mental Health. The service record listed the child’s age, gender, ethnicity, primary diagnosis, as well as the date/s, cost and type of the service. Children and youth with marked and severe functional limitations due to mental illness or other disabling conditions qualify for Supplemental Social Security payments. This qualification is included in the Medi-Cal claims file, and youth so adjudicated were considered disabled. To obtain child welfare participation data we merged Medi-Cal claims data with child welfare records obtained from The California Department of Social Services via probabilistic matching techniques, resulting in child welfare participation data for each child welfare-involved mental health client in our data set. Unique encrypted identifiers allowed tracking of each child throughout all three years. Approval to use these data for research purposes was obtained from the University of California Berkeley’s Institutional Review Board and the California Health and Human Services Agency’s Committee for the Protection of Human Subjects. Analysis Our final sample included 351,174 children and youth under age 18. This represents nearly all children receiving Medi-Cal specialty mental health care between July 1998 and June 2001. We followed a standard “two-part model” econometric approach (Mullahy, 1998), permitting us to address our two central questions—whether services were used and if they were used, how much they were used. We first used the entire sample to estimate differences in the odds that a Ethnic Minority Children 6 child or youth in the public mental health system used any crisis stabilization or crisis intervention services within the year (part 1). We used logistic regression to estimate part 1 equations. We then isolated sub samples of persons who used crisis stabilization or crisis intervention services, and estimated how many times during the year the child or youth used crisis stabilization and/or crisis intervention services (part 2). We used ordinary least squares (OLS) regressions estimated with robust standard errors after first transforming dependent variables into logarithmic form to adjust for skewed response distributions. We controlled for variables that have been shown to correlate with ethnicity or PES use and therefore possibly are correlated with both: age, gender, diagnosis, if the child was disabled, if the child was in regular foster care, kinship care, or had no child welfare involvement, county of residence, and year of observation. We included presence of a disability and child welfare involvement in the control variables because disabled youth (Witt, Kasper, & Riley, 2003; DosReis, Zito, Saefer & Soeken, 2001; Harman, Childs, & Kellcher, 2000) and children in foster care (Hurlburt, Leslie, Landsverk, Barth, Burns, Gibbons Slymen, Zhang, 2004) are more likely to receive mental health treatment. Additionally, African and Native American youth are more likely to reside in foster care of all kinds including in kinship care (Hines, Lemon, Wyatt, & Merdinger, 2004). We controlled for the type of foster care because children in kinship care receive less mental health treatment than other foster care children (Leslie, et al., 2000). We also employed a cross-sectional fixed effect dummy variable for each person’s county of residence because in California, mental health services are decentralized to the county level and county systems vary greatly in how they organize their mental health care including per-capita numbers and types of crisis services. Finally, we included a longitudinal fixed effect variable Ethnic Minority Children 7 indicating year of observation because policy-related developments and underlying state-wide trends are associated with emergency services use (Snowden, Masland, Wallace & Evans Cuellar, 2006). Results Descriptive Statistics The demographics for each ethnic group are shown in Table 1 and the diagnoses are shown in Table 2. In Table 3, the raw percentage of youth in the public mental health system who received crisis intervention and stabilization services, and the unadjusted mean number of visits per user, are shown by the child's race/ethnicity. Whereas 10.7% of children and youth used the less-intensive community-based crisis intervention service, only 1.6% used the more intensive hospital-based crisis stabilization service. Logistic Regression Results –Likelihood of Crisis Use The results from the logistic regression estimating likelihood of emergency services use are presented in Table 4. Analysis of the more intensive hospital-based crisis stabilization service showed that, controlling for covariates, African American (OR=1.11, p<.01), Asian American (OR= 1.20, p<.01), and Native American (OR=1.94, p<.01) children and youth had greater odds than White children and youth of using the service. Differences between Latinos (OR=1.06, p<.14) and White youth were not significant. Analysis of the less intensive community-based crisis intervention service showed that, controlling for covariates, only African American children and youth (OR=1.09, p<.01) had greater odds than White children and youth of using the service, while Latinos (OR=0.94, p<.01) and Asians (OR=0.90, p<.01) had lesser odds than White of using the service. Differences between Native Americans and Whites (OR=1.08 p<.19) were not significant. Ethnic Minority Children 8 Ordinary Least Squares Regression Results – Level of Crisis Use The results from the regression estimating number of crisis visits per client are presented in Table 5. Looking only at the children and youth who received any hospital-based crisis stabilization, our analysis showed that African Americans (β=.035, p<.05) used a greater number of crisis stabilization visits per child than Whites while Latinos (β=-.031, p<.05), Asians (β=.078, p<.01) and Native Americans (β=-.093, p<.05) children and youth had a fewer number of crisis stabilization visits than White children and youth. Looking only at the children and youth who received any community-based crisis intervention, our analysis showed that African Americans (β= -.051, p<.01), Latinos (β= -.061, p<.01) and Asians (β=-.107, p<.01) had fewer crisis intervention visits per client than Caucasians. The differences between Native Americans (β=.036, p<.23) and Whites were not significant. Discussion African American children and youth were more likely to use crisis care targeting both more and less severe crises, and for services targeting the most serious crises they showed more repeat use. Our hypotheses were largely confirmed for African American children and youth who proved, like African American adults (Snowden, Catalano, & Shumway, 2006), to use emergency services disproportionately. Asian Americans and Native Americans also proved more likely to require emergency intervention of the most serious kind. These findings are consistent with studies that report high rates of suicidal behavior (U.S. Department of Health and Human Services, 1999) and alcohol abuse (Lamarine, 1988) among some Native American groups, and high rates of suicidal ideation and suicide attempts among Asian youth (Halamandaris & Anderson, 1999; Breslow et al., Ethnic Minority Children 9 2000). Otherwise, and contrary to our hypotheses, Asian, Native, and Latino children and youth did not participate more than Whites in crisis-related mental health services. They were not repeat users of crisis stabilization and did not make greater use of less severe community based crisis intervention. Asian Americans children and youth’s sporadic use of only the most serious kind of crisis care resembles that of Asian American adults, who appear in treatment only when suffering from the most serious mental health problems (U.S. Department of Health and Human Services, 2001). We cannot fully explain disparities uncovered in the present study. It is possible that African American children and youth are more likely to use psychiatric emergency services because they have less access to outpatient treatments, but more research is needed to evaluate this hypothesis. For Latino, Asian and Native American children and youth cultural factors believed to act as barriers to mental health treatment--differing definitions of what constitutes a mental health problem and what is considered an appropriate form of intervention (Roberts, Alegria, Roberts & Chen, 2005), high levels of stigma associated with mental illness in minority communities (Pumariega, Rogers & Rothe, 2005), mistrust of the mental health system (Thompson, Bazile, & Akbar, 2004), and limited proficiency in English (Fiscella, Franks, Doescher, & Saver, 2002)--appear to apply to crisis care except for isolated instances where need is great and possibly unmanageable. One limitation of our study is that crisis stabilization users may also have used crisis intervention services and vice versa. We cannot determine this because we did not divide our sample into mutually exclusive groups based on use. Such an analysis is beyond the scope of the present study but should be carried out in future research. Ethnic Minority Children 10 Another limitation is that the R2 for model of crisis intervention use intensity is fairly low suggesting that the model omitted many determinants of emergency services use. These variables are especially important to identify and include if they relate to ethnicity as well as emergency services use and therefore represent possible confounds. Community outreach interventionists and clinical crisis care workers (Snowden, Masland, Ma, & Ciemens, 2006) should seek to inform minority youth and their caregivers about how to recognize signs of an impending crisis and, when possible, deescalate these situations before they become dangerous enough to warrant emergency intervention. Furthermore, crisis service workers who work with children and families who seek their help for non-urgent problems should encourage their clients to use more appropriate forms of treatment, and provide referrals to less-intensive services. Through mass-media, community health workers and other intermediaries, and culturally aware clinician can help to craft such messages to suit cultural lenses for viewing minority youth mental health problems and responding to them in culturally sensitive ways. Ethnic Minority Children 11 References American Academy of Pediatrics. (2005). California Medicaid Facts. Retrieved June 29, 2006, from http://www.aap.org/advocacy/washing/elections/mfs_ca.pdf. Blitz, C. L., Solomon, P. L., & Feinberg, M. (2001). Establishing a new research agenda for studying psychiatric emergency room treatment decisions. Mental Health Services Research, 3, 25-34. Breslow, R. E., Erickson, B. J., & Cavanaugh, K. C. (2000). The psychiatric emergency service: Where we’ve been and where we are going. Psychiatric Quarterly, 71, 101-121. Brody, G. H., Ge, X., Kim, S.Y., Murray, V., Simons, R. L., Gibbons, F. X., et al. (2003). Neighborhood disadvantage moderates associations of parenting and older sibling problem attitudes and behavior with conduct disorders in African American children. Journal of Consulting and Clinical Psychology, 71, 211-222. Buda, M., & Tsuang, M. T. (1990). The epidemiology of suicide: Implications for clinical practice. In S.I. Blumenthal & D. J. Kupfer (Eds.), Suicide over the life cycle: Risk factors, assessment, and treatment of suicidal patients (pp. 17-37). Washington D.C.: American Psychiatric Press Inc. Clark, R., Anderson, N.B., Clark, V.R., & Williams, D.R. (1999). Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist, 54, 805-816. DosReis, S., Zito, J.M., Safer, D.J. & Soeken, K.L. (2001). Mental health services for youths in foster care and disabled youths. American Journal of Public Health, 91(7) 1094-1099 Fiscella, K., Franks, P., Doescher, M.P. & Saver, B.G. (2002). Disparities in health care by race, ethnicity and language among the insured: Findings from a national sample. Medical Care, 40, 52-59. Ethnic Minority Children 12 Halamandaris, P.V., & Anderson, T. R. (1999). Child and adolescents in the psychiatric emergency setting. The Psychiatric Clinics of North America, 22, 865-876. Harman, J.S., Childs, G. E., & Kellcher, K. J. (2000). Mental health care utilization and expenditures by children in foster care. Archives of Pediatrics and Adolescent Medicine, 154(11), 1114-1117. Hines, A. M., Lemon, K., Wyatt, P., & Merdinger, J. (2004). Factors related to the disproportionate involvement of children of color in the child welfare system: A review and emerging themes. Children and Youth Services Review, 26, 507-527. Hovey, J., & King, C.A. (1996). Acculturative stress, depression, and suicidal ideation among immigrant and second-generation Latino adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 1183-1192. Hurlburt, M. S., Leslie, L.K., Landsverk, J., Barth, R. P., Burns, B. J., Gibbons, R. D. et al. (2004). Contextual predictors of mental health service use among children open to child welfare. Archives of General Psychiatry, 61, 1217-1224. Joe, S., & Marcus, S. (2003). Trends by race and gender in suicide attempts among US adolescents, 1991-2001. Psychiatric Services, 54, 454. Joffe, R. T., Offord, D. R., & Boyle M. H. (1988). Ontario child health study: Suicidal behavior in youth age 12-16 years. American Journal of Psychiatry, 145, 1420-1423. Kataoka, S.H., Zhang, L., Wells, K. B. (2002). Unmet need for mental health care among U.S. children: Variation by ethnicity and insurance status. American Journal of Psychiatry, 159, 1548-1555. Lamarine, R. (1988). Alcohol abuse among Native Americans. Journal of Community Health, Ethnic Minority Children 13 13, 143-155. Leslie, L.K., Landsverk, J., Ezzet-Lofstrom, R., Tschann, J.M., Slyman, D.J., & Garland, A.F. (2000). Children in foster care: Factors influencing outpatient mental health service use. Child Abuse & Neglect, 24, 465-476. Morano, C. D., Cisler, R. A., & Lemerond, J. (1993). Risk factors for adolescent suicidal behavior: Loss, insufficient familial support, and hopelessness. Adolescence, 28, 851-865. Mullahy, J. (1998). Much ado about two: reconsidering retransformation and the two-part model in health economics. Journal of Health Economics, 17, 247-281. Pumariega, A.J., Rogers, K., & Rothe, E. (2005). Culturally competent systems of care for children’s mental health: Advances and challenges. Community Mental Health Journal, 41, 539-555). Repetti, R.L., Taylor, S. E., & Seeman, T. E. (2002). Risky families: family social environments and the mental and physical health of offspring. Psychological Bulletin, 128, 330-366. Roberts, R.E., Alegria, M., Roberts, C.R., & Chen, I.G. (2005). Mental health problems as reported by their caregivers: A comparison of European, African, and Latino Americans. Journal of Behavioral Health Services & Research, 32, 1-13. Schwab-Stone, M. E., Ayers, T. S., Kasprow, W. Voyce, C. Barone, C. Shriver, T., et al. (1995). No safe haven: A study of violence exposure in an urban community. Journal of the American Academy of Child and Adolescent Psychiatry, 34, 1343-1352. Snowden, L. R., Catalano, R. F., & Shumway, M. (2006). Emergency mental health treatment and African American populations. Manuscript under review. Snowden, L. R., Masland, M., Ma, Y, & Ciemens, E. (2006). Strategies to improve minority access to public mental health services in California: Description and preliminary evaluation. Ethnic Minority Children 14 Journal of Community Psychology, 34, 225-235. Snowden, L. R, Masland, M., Wallace, N., & Evans-Cuellar, A. (2006). Strict Medicaid EPSDT Enforcement: Effect on Outpatient and Emergency Mental Health Care. Manuscript under review. Thompson, V.L., Bazile, A., & Akbar, M. (2004). African Americans’ perceptions of psychotherapy and psychotherapists. Professional Psychology- Research and Practice, 35, 19-26. U.S. Department of Health and Human Services. (1999). The Surgeon General’s call to action to prevent suicide: At a glance, suicide in the United States. Retrieved August 29, 2005 from http://www.surgeongeneral.gov/library/calltoaction/default.htm. U.S. Department of Health and Human Services. (2001). Mental Health: Culture, Race, and Ethnicity—A Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: Public Health Service, Office of the Surgeon General. Witt, W. P.,Kasper, J.D., & Riley, A. W. (2003). Mental health services use among school-aged children with disabilities: The role of sociodemographics, functional limitations, family burdens, and care coordination. Health Services Research, 38, 1441-1466. Yeh, M., McCabe, K., Hurlburt, M., Hough, R., Hazen, A., Culver, S. et al. (2002). Referral sources, diagnoses, and service types of youth in public outpatient mental health care: A focus on ethnic minorities. Journal of Behavioral Health Services & Research, 29, 45-60. Ethnic Minority Children 15 Table 1 Description of Independent Variables: Percent Demographic Characteristics by Race/Ethnicity Caucasian African Latino Asian Native Total American American (n=171090) (n=69438) (n=92293) (n=15365) (n=2988) (n=351174) Independent Variables % % % % % % Male 59.1 61.1 59.4 62.1 55.5 Not in Foster Care 89.1 89.6 89.4 91.1 87.0 Kinship Foster Care 3.2 2.4 3.4 1.9 3.4 Non-Kinship Foster Care 7.7 7.0 7.2 7.0 9.6 Disabled 9.8 22.0 4.2 30.0 11.4 Age 0-3 3.1 2.7 3.1 2.4 2.2 Age 4-5 7.2 6.4 7.4 4.8 7.0 Age 6-11 42.6 45.6 43.2 34.5 40.9 Age 12-17 47.2 45.3 46.4 57.8 49.9 Note: Percents add up to more than 100 because subjects can be in multiple categories. 59.7 89.4 3.1 7.5 11.7 3.0 7.0 43.0 47.1 Ethnic Minority Children Table 2 Description of Independent Variables: Percent Diagnosis by Race/Ethnicity Caucasian African Latino Asian American (n=171090) (n=69438) (n=92293) (n=15365) Diagnosis % % % % Mood Disorder 25.5 21.7 25.2 24.5 Adjustment Disorder 16.8 14.7 17.6 15.3 ADHD 15.4 17.1 12.1 13.0 Disruptive Behavior Disorder 11.7 15.9 15.4 15.1 Anxiety Disorder 10.9 8.9 10.6 7.8 Developmentally Disabled 3.2 3.5 2.6 4.7 Psychosis 1.4 2.4 1.3 3.7 Other 6.1 7.1 5.6 6.4 None or Missing 8.9 8.6 9.6 9.4 16 Native Total American (n=2988) (n=351174) % % 22.0 24.6 22.5 16.6 11.3 14.7 12.0 13.6 10.4 10.3 2.1 3.1 1.1 1.7 7.1 6.3 11.4 9.1 Ethnic Minority Children Table 3 Description of Dependent Variables: Probability and Level of Psychiatric emergency Use by Race/Ethnicity Psychiatric Number of visits Psychiatric Number of visits emergency among emergency among intervention psychiatric stabilization psychiatric use intervention use emergency users stabilization users % Mean SD % Mean SD Caucasian (n=171090) African American (n=69438) Latino (n=92293) Asian (n=15365) Native American (n=2988) Total (n=351174) 10.86 1.98 2.45 1.51 1.52 1.40 11.39 2.03 2.87 1.84 1.50 1.06 9.53 1.79 2.38 1.51 1.40 1.11 10.93 1.91 2.66 2.58 1.37 0.99 15.09 1.89 1.92 2.91 1.23 0.56 10.65 1.94 2.54 1.64 1.47 1.23 17 Ethnic Minority Children Table 4 Regression Results: Probability of Psychiatric emergency Use Among Ethnic Children Compared to Caucasian Children by Type of Psychiatric emergency Model Psychiatric Emergency Stabilization (n= 336,934) OR 95% CI Caucasiana African American Latino Asian Native American Femalea Male Kinship Foster Carea Nonkinship In Foster Carea Non Foster Age 12-17a Age 0-3 Age 4-5 Age 6-11 Not Disableda Disabled No Diagnosisa Developmentally Disabled ADHD Disruptive Adjustment Anxiety Psychotic Mood Personality Eating Substance Abuse Somatization 1.00 1.11*** 1.06 1.20*** 1.94*** 1.00 .81*** 1.00 2.65*** 1.00 2.03*** 1.00 0.15*** 0.10*** 0.34*** 1.00 1.31*** 1.00 0.77 1.24 1.94*** 3.54*** 2.16*** 24.61*** 11.90*** 8.96 9.96*** 36.12*** 4.39*** 1.03-1.21 .982-1.15 1.05-1.37 1.49-2.53 .763-.862 2.01-3.50 1.56-2.64 .095-.251 .069-.146 .312-.366 1.20-1.42 .445-1.34 .911-1.68 1.48-2.57 2.72-4.60 1.63-2.87 18.74-32.41 9.25-15.30 2.48-32.36 4.99-19.89 26.67-48.90 1.34-14.34 Psychiatric Emergency Intervention (n=336,894) OR 95% CI 1.00 1.09*** 0.94*** 0.90*** 1.08 1.00 0.84*** 1.00 1.62*** 1.00 0.70*** 1.00 0.26*** 0.41*** 0.68*** 1.00 1.25*** 1.00 0.90** 1.26*** 1.45*** 1.47*** 1.42*** 5.72*** 3.38*** 4.04*** 3.12*** 6.31*** 3.58*** 1.05-1.13 .912-.968 .846-.953 .962-1.22 .817-.857 1.51-1.74 .659-.749 .227-.289 .384-.438 .658-.693 1.21-1.30 .808-.999 1.19-1.34 1.38-1.54 1.39-1.55 1.34-1.51 5.31-6.17 3.23-3.54 2.52-6.49 2.32-4.20 5.60-7.11 2.50-5.14 Note: a indicates the comparison group. ***=p<.01, **=p<.05, * =p<.1. Dummy variables omitted for year and county. 18 Ethnic Minority Children Table 5 Regression Results: Number of Visits by Psychiatric Emergency Users Log level of use among Psychiatric Emergency Stabilization users (n=4,788) Variable Caucasiana African American Latino Asian Native American Femalea Male Kinship Foster Carea Nonkinship In Foster Carea Non Foster Age 12-17a Age 0-3 Age 4-5 Age 6-11 Not Disableda Disabled No Diagnosisa Developmentally Disabled ADHD Disruptive Adjustment Anxiety Psychotic Mood Personality Eating Substance Abuse Somatization Log level of use among Psychiatric Emergency Intervention users (n= 33,304) β SE β t β SE β t .035 -.031 -.078 -.093 .017 .015 .023 .038 2.08** 2.03** 3.38*** -2.43** -.051 -.061 -.107 .036 .009 .008 .015 .030 5.62*** 7.55*** 6.93*** 1.21 .008 .012 0.64 -.023 .007 3.39*** .145 .052 2.80*** .140 .016 8.66*** .049 .047 1.03 .020 .015 1.29 -.154 -.094 -.006 .040 .057 .017 -.150 -.100 -.028 .019 .014 .007 8.08*** 6.98*** 3.90*** .031 .017 1.87* .096 .010 9.56*** .257 .074 .040 .067 .169 .237 .194 .058 .539 .275 .451 .115 .041 .026 .023 .034 .028 .020 .033 .188 .043 .171 2.23** 1.80* 1.57 2.98*** 5.04*** 8.42*** 9.87*** 1.79* 2.87*** 6.46*** 2.64*** .083 .127 .171 .078 .200 .367 .310 .215 .370 .333 .135 .026 .015 .014 .013 .016 .021 .013 .132 .081 .030 .079 3.25*** 8.51*** 11.78*** 6.17*** 12.59*** 17.24*** 24.61*** 1.62 4.55*** 11.03*** 1.71* 3.89*** -1.65 -0.35 Note: Model 1: Psychiatric Intervention Use: F78,33225= 34.65, p<.000, R =.069. Model 2: Psychiatric Stabilization Use: F67,4715= p< , R2=.115. ***=p<.01, **=p<.05, * =p<.1 Dummy variables omitted for year and county 19