Dm – Patiënten met een (niet-chirurgische) wond die
advertisement

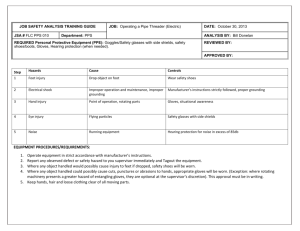
Sterile gloves: do we really need them in wound repair at the Emergency Department? M. Been, pre-registration house officer, S.J.P.G. Aller MD, Emergency physician St. Antonius Hospital Nieuwegein ABSTRACT Background – Sterile gloves are commonly used in wound management at the Emergency Department in order to prevent transmission of microorganisms as well as to protect the operator. However, it remains unclear whether sterile gloves provide an actual benefit compared to inexpensive non-sterile clean boxed gloves in the prevention of wound infections. Aim – To explore the best available evidence concerning the infection risk of wounds in the Emergency Department with either the use of sterile or non-sterile surgical gloves. Methods – A systematic search in Pubmed, Embase and Cochrane was performed. Based on title, abstract and full text relevant articles were selected. Using predefined criteria selected articles were critically appraised for relevance and validity. Results – The study of Perelman et al. was considered the most relevant. They included and randomized 816 immunocompentent patients with uncomplicated lacerations and found no significant difference in wound infection between sterile (6.1%) and non-sterile (4.1%) gloves (RR 1.37; 95%-CI 0.75-2.52). Conclusion – The best available evidence suggests that sterile gloves do not reduce the risk of infection when compared to non-sterile gloves in wound repair at the Emergency Department. However, further research is needed to confirm the findings of Perelman et al. Until then, we advise clinicians to carefully balance the risk factors that increase an individual’s risk. Clinical scenario . A 22-year-old man visits the Emergency Department after he fell off his bike. The fall resulted in a superficial laceration on his arm that requires suturing. Although it is common practise to use sterile gloves for this procedure, his doctor questions whether these costly sterile gloves actually improve wound healing, i.e. whether they reduce the risk of infection. 105 organisms/mL are needed to cause a wound infection.3 Previous research has shown that, although the bacterial load on clean gloves was significantly greater than that of sterile ones, the extent of this contamination was clinically irrelevant when compared to the bacterial load needed to cause an infection.4 In the case of wound irrigation, several studies have revealed that tap water instead of sterile saline can be safely used for cleansing wounds in the emergency setting.5,6,7 This evidence based case report aims to explore the clinical evidence for the benefit of sterile gloves in wound repair in the Emergency Department. Background . Current practise of using sterile techniques in small surgical procedures is the result of a longterm development with gradually increased knowledge about transmission of microorganisms and subsequent infections. The use of sterile gloves as part of this approach, motivated by the assumption that many bacteria on our hands cannot be sufficiently removed by soap or disinfectant, goes back to the nineteenth century.1 However, as evidence based medical practise is gaining ground against that of common sense, the question arises whether these sterile and costly gloves have actually proven their benefit in the healing process of lacerations repaired at the Emergency Department. Although current guidelines still favour sterile gloves, Dutch general practitioners are increasingly breaking the habit of using the expensive ones en use the inexpensive, non-sterile but clean gloves instead.2 Besides the economic issue, using nonsterile gloves is likely to save time and requires less assistance. It has been demonstrated that > FIGURE 1. Flowchart Clinical question . Does the use of sterile gloves in the treatment of patients with wounds requiring small surgery at the Emergency Department reduce the risk of infection, compared to the use of non-sterile gloves? Methods . Search strategy A systematic search in Pubmed, Embase and Cochrane Library was performed. Synonyms for the domain and determinant were combined (see appendix 1). Duplicates were removed using Refworks®. Title and abstract of all identified publications were independently screened by both reviewers, using in- and exclusion criteria as presented in the flowchart (figure 1). Subsequently, full texts of remaining publications were screened using the same 1 criteria. Cross reference checking in Web of Science was used to identify additional studies. setting.11,12,13 Eventually, two studies were excluded because sterile gloves were compared to no gloves at all.8,9 Critical appraisal Relevance and validity of the remaining studies were appraised using predefined criteria (table 1). Consensus about applicability was reached by all authors. Study results Results of the selected study can be found in table 2. Details are discussed briefly. Perelman et al.10 performed a multicenter randomized controlled trial to evaluate infection risk when using sterile or non-sterile gloves for the repair of uncomplicated lacerations in the Emergency Department. They included 816 immunocompetent patients with any type of uncomplicated soft tissue lacerations. Open fractures, vascular, nerve or tendon injury, bite wounds and patients with delayed presentation (>12 hours) were excluded. A wound infection was considered to be significant if the follow-up physician’s impression was that antibiotics or referral for wound care was needed. They found an absolute risk of wound infection of 6.1% in the sterile glove group and 4.4% in the clean glove group. This difference was not statistically significant (RR 1.37; 95%-CI 0.75-2.52). Data extraction From all included studies absolute risks, relative risks, risk differences and number needed to treat or data to compute these outcomes were extracted. Also, 95%-confidence intervals were calculated. Results . Search and selection The search was performed on August 18th 2013. The search retrieved 1267 unique articles. By applying in- and exclusion criteria on title and abstract, 13 articles remained. After full text screening additionally seven articles were excluded, because the article did not meet inclusion criteria (see figure 1). Discussion . It is commonplace to wear gloves in the management of wound care, not only in order to prevent transmission of microorganisms to the patient, but also to protect the operator from possible infections such as hepatitis. Although current guidelines encourage the use of Critical appraisal An overview of the articles8,9,10,11,12,13 that were critically appraised is presented in table 1. The study of Perelman et al.10 was considered the most relevant to answer our clinical question. Three studies were excluded because their domains were not applicable to the emergency 2 Rogues et al.12 (2007) Xia et al.13 ( 2011) Analysis Applicability Chiu et al.11 (2005) Blinding Standardization of treatment Standardization of outcome Selection Missing data bias Loss to follow up Confounding Randomization Baseline data Concealed allocation Intention to treat analysis Perelman et al.10 (2004) Validity Domain Determinant Outcome Study design Information bias Maitra et al.9 (1986) Relevance Bodiwala et al.8 (1982) TABEL 1. Critical appraisal + + + + + + + + + + + NS NS + - + + + + + + + + + + NS NS + - + + + + + + + + + + + + NS + + + + + + + + + + + + NS + - + + + ± + + + NS + - + + + + + + + + + + + NS + - Domain: patients with traumatic skin injury requiring suturing: +, patients with elective non-traumatic surgery or patients referred to operation room for complex surgery: -; determinant: comparison between sterile and nonsterile gloves: +, comparison between sterile gloves and no gloves -; outcome: risk of infection: yes +, no -; study design: randomized controlled trial: yes +, no -; blinding: blinding of physician who evaluates outcome: yes +, no -; standardization of treatment: clear description of standardized procedure: yes +, no -; standardization of outcome: clear description of standardized outcome: yes +, no -; missing data: <10% or no risk of selection bias +, 10-20% with risk of selection bias ±, >20% with risk of selection bias -; loss to follow up: <10% or no risk of selection bias +, 10-20% with risk of selection bias ±, >20% with risk of selection bias -; randomization: yes +, no -; baseline data: available: yes +, no -; concealed allocation: yes +, no -; intention to treat analysis: yes +, no –; analysis: AR, RR, RD, NNT and CI mentioned or extractable from data: yes +, no -; NS: not specified. sterile gloves, this evidence based case report questions their benefit in wound management in the Emergency Department to prevent infections. gloves, the so-called Hawthorne effect. Considering the high occurrence of traumatic wounds in the Emergency Department, the authors suggest that implementing the use of non-sterile gloves could be expected to have a modest positive economic impact, as sterile gloves can be up to ten times as expensive, and in addition, may be timesaving as well.10 Our findings suggest that, when compared to non-sterile gloves, the use of sterile gloves in repairing wounds does not lead to reduced infection risk and hence does not necessarily contribute to a better healing of the wound. It should be noted that Perelman et al. studied immunocompetent patients with uncomplicated lacerations, hence these results account only for this population. Interestingly, they found even a lower, although non-significant, infection rate in the non-sterile group. The authors suggest this might be the result of the operating physicians (who were not blinded for the type of gloves) being more careful when using non-sterile A few limitations should be taken into account when interpreting our findings. First, a systematic search in three databases revealed only one article that compared sterile to clean gloves in the context of traumatic lacerations in the Emergency Department. Nevertheless, noninferiority of clean gloves was also found in studies of patients who underwent minor procedures in both general practices, dermatology clinics and dental care.2,11,13 3 TABLE 2. Results Perelman et al.10 (2004) Definition of infection Intervention Antibiotics or referral for wound care was required Sterilized latexfree gloves (Allegiance; Cardinal Health Co.; IL) vs. standard cleanboxed nonsterile, latexfree gloves Infection rate Sterile (%) Control (%) RR (95%-CI) RD NNT 24/396 (6.1) 17/384 (4.4) 1.37 (0.75-2.52) -0.017* (-0.046-0.017) -61* RR relative risk (%infectionssterile / %infectionscontrol); RD risk difference (%infectionssterile - %infectionscontrol); NNT number needed to treat (1/RD); 95%-CI 95%-confidence interval. * minus-symbol indicates that results favour the control group. Furthermore, two older randomized studies that compared sterile gloves to bare hands found no overall difference in the incidence of infections.8,9 Second, to estimate an individual’s risk of infection other risk factors should be taken into account. For example, the time between trauma and treatment, immune status of the patient and the complexity of the procedure. The latter two have shown to be independent risk factors that increase the risk of infection.3 compared to non-sterile gloves in wound repair at the Emergency Department. Recommendations . We recommend that non-sterile boxed gloves can be safely used at the Emergency Department for the repair of lacerations. However, further research is needed to confirm and extend the findings of Perelman et al. Until then, we advise clinicians to carefully balance the risk factors that increase an individual’s risk such as immunocompromised patients or a complex procedure, as this case report is limited to uncomplicated cases with immunocompetent patients. Conclusion . Although evidence on this topic is scarce, the best available evidence suggests that sterile gloves do not reduce the risk of infection when 4 References 1. 2. 3. 4. 5. 6. 7. . Broek van den, PJ. Steriele handschoenen wél nodig bij kleine chirurgie. Ned Tijdschr Geneeskd. 2011;155:A2954. Bruens ML, Keijman JMG, van den Berg PJ. Steriele handschoenen zijn niet nodig bij kleine chirurgie. Een kritische beschouwing van de NHG-Richtlijn Infectiepreventie. Huisarts Wet 2008;51:444-6. Raahave D, Friis-Møller A, Bjerre-Jepsen K, et al. The infective dose of aerobic and anaerobic bacteria in postoperative wound sepsis. Arch Surg. 1986;121:924 –9. Creamer J, Davis K, Rice W. Sterile gloves: do they make a difference? Am J Surg. 2012;204:976–980. Angeras MH, Brandberg A, Falk A, et al. Comparison between sterile saline and tap water for the cleaning of acute traumatic soft tissue wounds. Eur J Surg.1992;158:347-350. Valente JH, Forti RJ, Freundlich LF, et al. Wound irrigation: tap water or saline? [abstract] Acad Emerg Med. 8:539. Riyat MS, Quinton DN. Tap water as a wound cleansing agent in accident and emergency. J Accid Emerg Med. 1997;14:165-166. 8. 9. 10. 11. 12. 13. 5 Bodiwala GG, George TK. Surgical gloves during wound repair in the accident-and-emergency department. The Lancet. 1982;10:91-92. Maitra AK, Adams JC. Use of sterile gloves in the management of sutured hand wounds in the A&E department. Injury. 1986;17:193-195. Perelman VS, Francis GJ, Rutledge T, Foote J, Martino F, Dranitsaris G. Sterile versus nonsterile gloves for repair of uncomplicated lacerations in the emergency department: a randomized controlled trial. Ann Emerg Med. 2004;43:362-70. Chiu WK, Cheung LK, Chan HC, Chow LK. A comparison of post-operative complications following wisdom tooth surgery performed with sterile or clean gloves. Int J Oral Maxillofac Surg. 2006;35:174-179. Rogues AM, Lasheras A, Amici JM, et al. Infection control practices and infectious complications in dermatological surgery. J Hosp Infect. 2007;65:258-63. Xia Y, Cho S, Greenway HT, Zelac DE, Kelley B. Infection rates of wound repairs during mohs micrographic surgery using sterile versus nonsterile gloves: a prospective randomized pilot study. Dermatol Surg. 2011;37:651-656. APPENDIX 1. Search strategy performed on August 18th 2013 Pubmed Embase Cochrane Domain* (stitching[tiab] OR stitch[tiab] OR stitches[tiab] OR suturing[tiab] OR suture[tiab] OR sutures[tiab] OR wound[tiab] OR wounds[tiab] OR laceration[tiab] OR lacerations[tiab] OR cut[tiab] OR trauma[tiab]) (stitching:ab,ti OR stitch:ab,ti OR stitches:ab,ti OR suturing:ab,ti OR suture:ab,ti OR sutures:ab,ti OR wound:ab,ti OR wounds:ab,ti OR laceration:ab,ti OR lacerations:ab,ti OR cut:ab,ti OR trauma:ab,ti) (stitching OR stitch OR stitches OR suturing OR suture OR sutures OR wound OR wounds OR laceration OR lacerations OR cut OR trauma) Determinant (sterile[tiab] OR sterility[tiab] OR sterilized[tiab] OR nonsterile[tiab] OR nonsterility[tiab] OR nonsterilized[tiab] OR aseptic[tiab] OR antibacterial[tiab] OR antibacterial[tiab] OR antiseptic[tiab] OR clean[tiab]) AND (glove[tiab] OR gloves[tiab] OR equipment[tiab] OR material[tiab]) (sterile:ab,ti OR sterility:ab,ti OR sterilized:ab,ti OR non-sterile:ab,ti OR non-sterility:ab,ti OR nonsterilized:ab,ti OR aseptic:ab,ti OR antibacterial:ab,ti OR antibacterial:ab,ti OR antiseptic:ab,ti OR clean:ab,ti) AND (glove:ab,ti OR gloves:ab,ti OR equipment:ab,ti OR material:ab,ti) (sterile OR sterility OR sterilized OR non-sterile OR non-sterility OR nonsterilized OR aseptic OR antibacterial OR antibacterial OR antiseptic OR clean) AND (glove OR gloves OR equipment OR material) Total hits 619 894 183 Note: domain and determinant were combined by using “AND”. * For domain synonyms for suturing as well as for wound were used as we expected studies could either describe their domain as patients who need suturing or patients having wounds. 6