Unit 9 Wound Care and Sterile Technique
advertisement
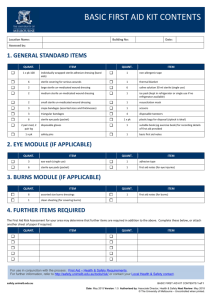
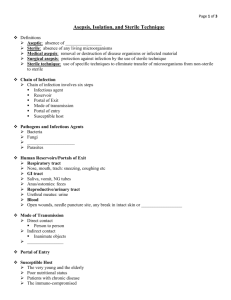
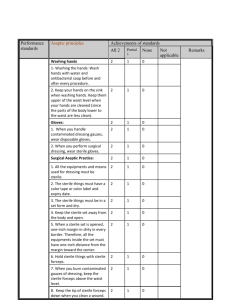
Metro Community College Nursing Program Nancy Pares, RN, MSN Age ◦ Elders: less elastic, drier, circulation impairment longer regeneration Mobility ◦ Increased pressure leads to breakdown Nutrition ◦ Poor nutrition, less regeneration, dehydration leads to poor turgor, increase risk of infection • Sensation level – Increased risk for pressure and breakdown • Impaired circulation – Decreased O2 supply impacts healing ability, vessel disease, smoking • Medications – Side effects: itching, rashes • Diabetes – Impairs inflammatory response from hypoglycemia; must maintain control of BS • Moisture – Leads to maceration • Obesity – Less blood supply in adipose tissue • Fever – Affects moisture and metabolic rate • Infection – Impedes healing • Lifestyle – Tanning, bathing, piercings • • Based on length of time wound existed and the condition of the wound Open/closed – No breaks in skin vs. true break in skin • Acute/chronic – Short vs. prolonged healing • Clean/contaminated/infected – Uninfected vs. open traumatic vs. evidence of infection Superficial ◦ Epidermis: friction, shearing, burns Partial ◦ Extend into dermis Full ◦ Extend into subcutaneous tissue Penetrating ◦ Involves internal organs Serous: clear-straw colored, watery ◦ Clean wounds Sanguinous: bloody ◦ Deep wounds Serosanguinous: pale pink (mixed) ◦ New wounds Purulent: yellow or green tinged pus Purosanguinous: red tinged pus Regeneration ◦ Same process regardless of injury or tissues ◦ When wound involves only epidermis ◦ No scar Primary intention ◦ Minimal scarring ◦ Clean, surgical incision; edges well approximated Secondary intention ◦ Extensive tissue loss ◦ Wound not well approximated; heals from inner surface to outer; epithelial tissue may look like sign of infection Tertiary intention (delayed closure) ◦ Granulating tissue is brought together; initially wound heals by secondary intention then is sutured; moderate scarring • Inflammatory: cleansing stage lasts 1-5 days – Hemostasis; vasoconstriction, platelets arrive at site, clotting occurs – Inflammation: vasodilatation, phagocytosis, scab formation • Proliferative: granulation stage lasts 5-21 days – Fibroblasts form a bed of collagen – Fills defects and produces new capillaries • Maturation: epitheliazation, begins 2nd or 3rd wk – Contraction of wound edges; scar tissue formation; scar tissue is 80% strong as original tissue. • • Hemorrhage Infection – 2-3 days in contaminated wound; 4-5 days post op • • • Hematoma Dehiscence: likely during inflammatory phase Evisceration – Place sterile saline soaked 4x4 over area – Call MD or notify charge/ surgical emergency • Fistula: abnormal passageway often from infection • Location – Anatomic terms • Size – Length and width • Appearance – Type, color (Red, yellow black), condition, • • • Skin around the wound Drainage Patient pain Cleansing and irrigation ◦ Use saline, dilute antimicrobial or commercially prepared cleansers—no hydrogen peroxide, alcohol or iodine; gentle is best; hydrotherapy=debridement Caring for drainage devices : Vol 2 Sharp ◦ MD or PT at bedside or OR Mechanical ◦ Wet to dry dressing-used less ◦ Hydrotherapy Enzymatic ◦ Topical agent Autolysis ◦ Uses body out mechanisms Gauze Transparent ◦ Clear, semi permeable, non absorbent, often used for IV sites Hydrocolloids/hydrogels ◦ Water loving particles that form a gel with exudate Absorption See page 840 table • Securing dressings – Tape, Montgomery straps • Binders • Important Nursing interventions – See 34-6,7 Vol 2 – Inspect skin, assess and change dressings as ordered – Always ACE wrap distal to proximal – Assess for circulatory impairment • Clients at risk – Very old or very young – Sensory impairment – Body areas: highly vascular—fingers, hands, face • Moist heat • Dry heat – Moisture amplifies the treatment; vasodilates, reduces muscle tension – Use with great caution • Vasoconstriction – Decreases edema and inflammation – Acts as a local anesthetic – Slows bacterial growth – Used in the first 24 hrs following injury – R-est – I-ce – C-ompress – E-levate Surgical asepsis ◦ Absence of all microorganisms ◦ Slightest break in technique=contamination ◦ Sterile object is only sterile when touched by another sterile object ◦ When in doubt….throw it out…. ◦ Place only sterile objects on a sterile field ◦ Sterile object or field that is out of visual range is contaminated If exposed to air for a prolonged time=contaminated Sterile border =field plus 1 inch Do not reach over a sterile field Keep hands in front and above waist in field of vision Procedures which require sterile technique ◦ Injection preparation , catherizations