Supplementary Information (doc 458K)
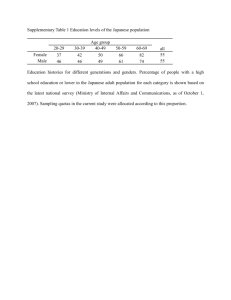
advertisement

Weight Maintenance and Additional Weight Loss with Liraglutide after Low-calorie Dietinduced Weight Loss: the SCALE™ Maintenance Randomized Study Thomas Wadden, Priscilla Hollander, Samuel Klein, Kevin Niswender, Vincent Woo, Paula M. Hale, and Louis Aronne, on behalf of the NN8022-1923 Investigators Non-thyroid related neoplasms reported during the trial Three non-thyroid malignant neoplasms (reported as AEs) occurred in participants treated with liraglutide 3.0 mg; two cases of breast cancer (ductal carcinoma in situ and bilateral breast cancer), and one case of ovarian cancer. Benign neoplasms in 6 liraglutide-treated participants included benign breast neoplasm, fibroma, lipoma, papilloma, prolactinoma and a uterine leiomyoma. Four participants in the placebo-treated group exhibited neoplasms. Two malignancies were reported; one basal cell carcinoma and one case of metastases to the lung. Two benign neoplasms were reported; one case of pseudolymphoma that had been a recurrence, and one report of a benign skin papilloma. 1 Supplementary Table 1 Complete list of inclusion and exclusion criteria Inclusion criteria 1. Informed consent obtained before any trial-related activities. (Trial-related activities are any procedure that would not have been performed during the normal management of the participant). 2. BMI 30 kgm-2, or BMI 27 kgm-2 with presence of co-morbidities of treated or untreated dyslipidemia and/or hypertension. Untreated dyslipidemia was defined as low-density lipoprotein (LDL) ≥160 mgdl-1, or triglycerides ≥150 mgdl-1, or high-density lipoprotein (HDL) < 40 mgdl-1 for men and < 50 mgdl-1 for women. Untreated hypertension was defined as systolic blood pressure ≥140 and/or diastolic blood pressure ≥90 mmHg. 3. Stable body weight during the previous 3 months (<5 kg self-reported weight change) 4. Age 18 years 5. Previously undergone dietary weight loss and not able to maintain reduced weight Exclusion criteria 1. Any clinically significant disease which in the Investigators’ opinion could interfere with the safety of trial participants or with the results of the trial 2. Diagnosis of type 1 or type 2 diabetes per the judgment of the Investigator 3. FPG 126 mgdl-1 (7 mmoll-1) at start of run-in period 4. Previous treatment with GLP-1 receptor agonists (including liraglutide or exenatide) within the last 3 months 5. Visit 1 thyroid-stimulatory hormone outside of the range of 0.4-6.0 mIUl-1. 6. History of chronic pancreatitis or idiopathic acute pancreatitis 7. Obesity induced by other endocrinological disorders (e.g., Cushing syndrome) 8. Current or history of treatment with medications that may cause significant weight gain within 3 months prior to screening visit, including systemic corticosteroids (except for a short course of treatment, i.e., 7-10 days), tri-cyclic antidepressants, atypical antipsychotic and mood stabilisers (e.g., imipramine, amitriptyline, mirtazapin, phenelzine, chlorpromazine, thioridazine, clozapine, olanzapine, valproic acid and its derivatives, and lithium) 9. Current participation in an organized diet reduction program (or within the last 3 months) 10. Currently using or have used within the last 3 months before screening for this trial: pramlintide, sibutramine, orlistat, zonisamide, topiramate, phentermine, or metformin (either by prescription or as part of a clinical trial) 11. Diet attempts using herbal supplements or over-the-counter medications within 3 months before screening for this trial 12. Participation in a clinical trial of weight control within the last 3 months prior to screening for this trial 13. Previous surgical treatment for obesity (excluding liposuction if performed >1 year before study entry) 2 14. History of major depressive disorder or a PHQ-9 >15 within the last 2 years (completed at visit 1) or history of other severe psychiatric disorders (e.g., schizophrenia or bipolar disorder) or diagnosis of an eating disorder such as restrained eating, binge eating, or bulimia (based on Questionnaire for Diagnosing Binge Eating Disorder and Bulimia Nervosa completed at visit 1) 15. Participants with a lifetime history of a suicide attempt or history of any suicidal behavior within the past month before entry into the trial 16. Surgery scheduled for the trial duration period, except for minor surgical procedures, at the discretion of the Investigator 17. Impaired liver function, defined as screening aspartate aminotransferase or alanine aminotransferase 2.5 times upper normal range (one re-test analyzed at the central laboratory within 1 week is permitted with the last sample being conclusive) 18. Impaired renal function defined as serum creatinine 152 moll-1 ( 1.72 mgdl-1) (one retest within one week through the central laboratory is permitted with the result of the last sample conclusive) 19. Known clinically significant active cardiovascular disease, including history of unstable angina, acute coronary event, other significant cardiac events (including history of arrhythmias, myocardial infarction (MI), or conduction delays on electrocardiogram [ECG]), or cerebral stroke within the past 6 months and/or heart failure (New York Heart Association [NYHA] Class III or IV) at the discretion of the Investigator 20. Uncontrolled treated/untreated hypertension (systolic blood pressure 160 mmHg and/or diastolic blood pressure 100 mmHg). If white-coat hypertension is suspected at the screening visit a repeated measurement at run-in prior to other trial-related activities is allowed 21. Cancer (past or present, except basal cell skin cancer or squamous cell skin cancer), which in the Investigator’s opinion could interfere with the results of the trial 22. Known or suspected allergy to trial product(s) or related products 23. Previous participation in the run-in or randomized phase of this trial. Re-screening is allowed once within the limit of the recruitment period 24. Known or suspected abuse of alcohol or narcotics 25. Language barrier, mental incapacity, unwillingness or ability to understand and being able to complete the mental health questionnaire in the provided language 26. Participants from the same household participating in the trial 27. Women of childbearing potential who are pregnant, breast-feeding or intend to become pregnant or are not using adequate contraceptive methods (abstinence and/or the following methods: diaphragm with spermicide, condom 3 with spermicide (by male partner), intrauterine device, sponge, spermicide, Norplant, Depo-Provera or oral contraceptives) 28. Positive screening for hepatitis B antigen, hepatitis C antibodies, positive human immunodeficiency virus (HIV) antibodies 29. The receipt of any investigational drug within four weeks prior to screening for this trial. 4 Supplementary Table 2 Supportive analyses for co-primary endpoints Change from randomization to week 56 Estimated treatment differences (ETD) or odds ratios (OR) for liraglutide vs. placebo (95% CI), P value Liraglutide 3.0 mg Placebo n=148 n=141 -6.7 (7.7) -0.1 (7.6) ETD = -6.8 (-8.5, -5.0), P<0.0001 80.4% 48.2% OR = 4.9 (2.8, 8.5), P<0.0001 Proportion with >5% weight loss 52.7% 22.7% OR = 4.2 (2.4, 7.0), P<0.0001 Repeated measures analysis n=156 n=144 -6.8 (7.8) 0.0 (7.5) ETD = -6.1 (-7.7, -4.6), P<0.0001 73.4% 42.7% OR = 3.3 (2.2, 5.0), P<0.0001 Proportion with >5% weight loss 42.5% 18.0% OR = 3·9 (2.4, 6.3), P<0.0001 Analysis with fasting and non-fasting n=212 n=208 -5.2 (7.5) 0.1 (7.3) ETD = -5.4 (-6.8, -3.9), P<0.0001 77.4% 47.1% OR = 3.8 (2.5, 5.8), P<0.0001 42.9% 20.5% OR = 3.0 (1.9, 4.7), P<0.0001 Per-protocol (completer) analysis Body weight (% change) Proportion maintaining ≥5% run-in weight loss Body weight (% change) Proportion maintaining ≥5% run-in weight loss observations* Body weight (% change) Proportion maintaining ≥5% run-in weight loss Proportion with >5% weight loss Changes from randomization to week 56 are observed means (SD). Estimated treatment differences are from an analysis of covariance, and odds ratios are from a logistic regression analysis. The per-protocol analysis set included all participants from the full analysis set who did not significantly violate inclusion, exclusion or randomization criteria, who had a valid assessment at week 56, where week 56 was at least 52 weeks (365 days) after first drug date, but who were allowed to be off drug for a total of 4 weeks during the trial, but at most 2 consecutive weeks. No imputation was performed on the data. Body weight was measured in the fasting state. The repeated measures analysis (linear mixed-effect model) was done using the full analysis set with no imputation. Body weight was measured in the fasting state. *This sensitivity analysis also included observations off drug, and was performed using the last observation carried forward. 5 Supplementary Table 3 Additional measures of body weight maintenance Change from randomization to week 56 Proportion with ≥5% weight Estimated odds ratios for liraglutide vs. placebo (95% CI), P value Liraglutide 3.0 mg Placebo n=207 n=208 1.9% 17.5% 0.09 (0.03, 0.26), P<0.0001 0.0% 2.9% 0.0 (0.0, non-estimable), P=1.0 93.2% 70.9% 5.9 (3.1, 11.0), P<0.0001 87.4% 54.4% 6.0 (3.7, 9.9), P<0.0001 regain Proportion with ≥10% weight regain Proportion maintaining >50% run-in weight loss Proportion maintaining >75% run-in weight loss Changes from randomization to week 56 are observed means. Estimated odds ratios are from a logistic regression analysis, using the full analysis set with the last observation carried forward. 6 Supplementary Table 4 Summary of adverse events Liraglutide 3.0 mg (n=212) Placebo (n=210) N (%) E N (%) E 194 (91.5) 1375 186 (88.6) 1067 Total serious adverse events 9 (4.2) 9 5 (2.4) 6 Total withdrawals 53 (25) N/A 64 (30.5) N/A Total adverse events a Withdrawals due to adverse events 18 (8.5) 41 18 (8.6) 23b Withdrawals due to serious adverse events 5 (2.4) 5 1 (0.5) 1 N=Number of participants with adverse event. %=proportion of participants in analysis set having adverse event. E=number of adverse events. N/A=not applicable. a The 41 events that led to withdrawal in the 18 liraglutide-treated participants were: ovarian cancer; intermittent diarrhea; diarrhea/intestinal gas/eructation; elevated blood creatine phosphokinase; papillary thyroid carcinoma; breast cancer; nausea; diarrhea/nausea/vomiting; nausea/headache/constipation/blurred vision/dizziness; nausea/dizziness; adjustment disorder; nausea/headache; nausea/constipation/back pain/dizziness/feeling abnormal/ageusia/urine flow decreased; cholelithiasis; diarrhea; ischemic colitis; weight loss/general malaise/ hypoglycemia; and diarrhea/nausea/flatulence/ abdominal pain/eructation/dysgeusia. b The 23 events that led to withdrawal in the 18 placebo-treated participants were: pruritus; dry throat; type 2 diabetes (5 people); palpitations; fatigue/agitation/blurred vision/confusion/alopecia; nephrotic syndrome; non-cardiac chest pain/palpitations; lung metastases; diverticulum; drug intolerance; generalized anxiety disorder; stress; appendicitis; tension headache. 7 Supplementary Table 5 Psychiatric disorders (randomization to week 56) Category/Preferred Term Lira 3.0 mg Placebo n=212 n=210 N % E R N % E R 24 11.3 31 15.9 26 12.4 30 16.3 Insomnia 5 2.4 7 3.6 7 3.3 7 3.8 Middle insomnia 1 0.5 1 0.5 1 0.5 1 0.5 Sleep disorder – – – – 2 1.0 2 1.1 Anxiety 9 4.2 9 4.6 2 1.0 2 1.1 Agitation – – – – 1 0.5 1 0.5 Anger – – – – 1 0.5 1 0.5 Generalized anxiety disorder – – – – 1 0.5 1 0.5 Stress 5 2.4 5 2.6 6 2.9 6 3.3 Adjustment disorder 1 0.5 1 0.5 – – – – Adjustment disorder with 1 0.5 1 0.5 – – – – Bipolar disorder 1 0.5 1 0.5 – – – – Decreased interest 1 0.5 1 0.5 – – – – Depression 4 1.9 4 2.1 3 1.4 3 1.6 Dysthymic disorder – – – – 1 0.5 1 0.5 Libido decreased – – – – 1 0.5 1 0.5 Major depression – – – – 1 0.5 1 0.5 Mood swings – – – – 1 0.5 1 0.5 Attention deficit/hyperactivity disorder 1 0.5 1 0.5 1 0.5 1 0.5 Confusional state – – – – 1 0.5 1 0.5 TOTAL Sleep Disorders Anxiety Depression depressed mood Cognition N = Number of participants with adverse event. % = proportion of participants in analysis set having adverse event. E = number of adverse events. R = event rate per 100 exposure years. 8 Supplementary Figure 1 Trial design 9 Supplementary Figure 2 Proportion of individuals with nausea Observed mean data for the safety analysis set (n=422). 6 of the 7 events of nausea that led to participant withdrawal had onset in the first 4 weeks of the trial. 10 Supplementary Figure 3 Geometric mean changes in (a) calcitonin, (b) lipase and (c) amylase Observed mean data for the safety analysis set (n=422). a b c 11