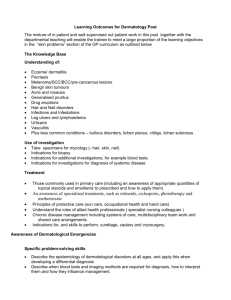
ResidentLearningObje..
advertisement

I. INTENSIVE CARE UNIT TRAINING PROGRAM LEARNING OBJECTIVES FOR ROTATING ICU RESIDENT An 8 week rotation in the ICU is intended to provide residents in Medicine, Surgery, Anesthesia, Emergency Medicine, and Family Medicine with experience in the evaluation and initial management of critically ill patients. We encourage you to identify specific learning objectives for yourself, and bring them to our attention. We expect that you will achieve the following specific educational objectives. At the end of this rotation you will be able to: 1. Use a question/hypothesis testing approach in diagnosis and management of patients. Use knowledge of pathophysiology as a foundation for understanding clinical presentation and management of patients. 2. Recognize the patient who is in shock or who has significant cardiopulmonary compromise. Demonstrate the appropriate use of clinical information: history, physical examination, basic laboratory and radiographic investigations to develop a reasonable differential diagnosis and management plan for such a patient. List the indications and contraindication for invasive hemodynamic monitoring. Provide central venous access from the internal jugular, subclavian and femoral veins, and arterial access from the radial and femoral arteries. Place and use a pulmonary arterial catheter to obtain cardiac output, intracardiac pressures, and venous oxygen content analysis. Demonstrate the use of this information to modify hemodynamic function and treat shock states using appropriate fluids and vasoactive drugs (including dopamine, dobutamine, nitroglycerin, nitroprusside and noradrenaline). 3. Identify the patient who has respiratory failure. Demonstrate the appropriate use of clinical information: history, physical, radiographic and laboratory to develop a reasonable differential diagnosis and initial management plan for such a patient. Use and recommend oxygen delivery devices appropriately (nasal prongs, low and high-flow masks). Provide effective bag-mask ventilation. Describe and identify the indications for intubation and mechanical ventilation. Describe and contrast basic modes of ventilation (assist control ventilation, pressure support ventilation, continuous positive airway pressure, PRVC), and select ventilator settings (rate, tidal volume, Fi02, PEEP) appropriate for specific patients. 10 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. Evaluate a patient's potential for weaning and initiate a weaning program. Demonstrate correct placement of a chest tube and evaluate its function using a closed drainage system. Utilize radiographs to identify the correct placement of a venous and pulmonary arterial catheter, chest tube, pacer wire, feeding tube and endotracheal tube. Recognize major abberations in chest radiographs including pneumothorax, lobar collapse, consolidation or pleural effusion, and have a practical differential of common radiographic abnormalities. Demonstrate the management of patients after major vascular, abdominal, and cardiac surgery in discussion with the surgical services. Demonstrate the evaluation of a patient with reduced level of consciousness, list a differential diagnosis of coma, and outline a plan to investigate it. Describe the principles of monitoring and manipulation of intracranial pressure and demonstrate the application of this knowledge to the patient's care. List the criteria for the diagnosis of brain death. Identify and differentiate common coagulopathies including those due to factor deficiency, liver disease, platelet deficit or dysfunction, DIC, fibrinolysis, and consequences of massive transfusion. Use of blood products, protamine, and vitamin K appropriately. List the common sites and organisms responsible for infections in critically ill patients. Identify and investigate patients with suspected sepsis and select appropriate initial antibiotic therapy. Describe the nutritional needs of critically ill patients, recommend and monitor appropriate nutritional support. Correctly place and monitor venous access for TPN and feeding tubes for enteral feeds. Describe the basic pharmacology of common sedatives, analgesics, and neuromuscular blocking agents. Select and monitor the use of these drugs appropriately. Describe the normal distribution of fluids and electrolytes. Demonstrate an appropriate choice of fluid therapy for patients who have shock, cardiac, or renal failure, and after major surgery. Identify the patient who has significant renal dysfunction. Monitor and manage anticipated disturbances of fluids and electrolytes, including identifying the need for urgent dialysis. Identify, anticipate, and demonstrate the appropriate management of common electrolyte disturbances. Identify the patient who has a significant acid-base disturbance, and describe a reasonable differential diagnosis and management plan.Plan the transport of a critically ill person and demonstrate this ability in arranging the transport of such a patient to or from this centre. Discuss the factors determining the prognosis of critically ill patients. Demonstrate this knowledge in arriving at and discussing patient care decisions with fellow caregivers and family members. Describe the condition of a critically ill patient to his/her family and address their concerns in a compassionate and therapeutic manner. Demonstrate interacting with other physicians and health care workers in a collaborative way to arrive at a plan for patient care. Demonstrate knowledge of ethical principles in decision making. Accurately communicate your diagnostic and therapeutic plans verbally and in writing in the medical record. Identify your own strengths and limitations, and appropriately seek guidance and consultation. The following is a list of topics that will be addressed during the Housestaff rotation through the MRICU. Teaching methods will include bedside teaching and discussion on teaching rounds, didactic instruction of an informal (freeform or chalkboard) or more formal (PowerPoint slides) nature, discussion of important medical literature, demonstration, supervision, and performance of procedures, textbook review, and self-study using PowerPoint slide sets, reprints of key articles, other written and instructional materials on the computer. 1. Ethics—understand principles of advanced directives, terminal care and conflict resolution in the context of the ICU 2. Assessment of severity of illness: understand the rationale, applications, and limitations of severity of illness scoring systems 3. Hemodynamic monitoring: know indications, contraindications, techniques, and potential complications for arterial catheterization, central venous catheterization, and pulmonary artery catheterization. Be able to interpret hemodynamic data and analyze waveforms. 4. Pharmacology in the ICU: understand the basic principles of pharmacokinetics and how organ dysfunction and critical illness can influence it. Understand the indications and potential complications of vasopressors, ionotropes, sedatives and paralytic agents. 5. Airway management: know principles of airway management including the indications, contraindications, techniques, and potential complications for orotracheal and nasotracheal intubation as well as the alternatives to endotracheal intubation. 6. Mechanical ventilation including principles of positive pressure ventilation; resistance and compliance, common modes, settings, alarms and monitors; application in ARDS; mechanisms, risk factors, recognition and management of barotrauma and pneumothorax; principles of weaning; indication, contraindications, techniques and potential complications of noninvasive ventilation. 7. Arterial blood gas and pulse oximetry interpretation including techniques, limitations, and principles of acid-base physiology and interpretation. 8. Hypoxemia and Respiratory failure—causes pathophysiology, and management of various forms including hypoxemic and hypercapneic respiratory failure. Understands the pathophysioligical differential diagnoses of hypoxemia and application of A-a gradient 9. ARDS—defining characteristics, causes, pathophysiology, and management. 10. Pneumonia—agents and antibiotics for severe community acquired pneumonia; pathophysiology, manifestations, prevention, diagnostic testing and management of ventilator-associated pneumonia. 11. Life-threatening asthma—principles of mechanical ventilation and pharmacologic management options. 12. Shock—mechanisms of hypovolemic, maldistributive, cardiogenic and obstructive; principles of resuscitation and monitoring; indications and characteristics for common vasopressors and ionotropic agents. 13. Hypertensive crisis—criteria for hypertensive urgency and emergency; treatment agents including indications, contraindications and potential adverse effects. 14. Acute renal failure—differential diagnosis, management principles, indications for dialysis. 15. Fluid and electrolyte disorders—understand pathophysiology, manifestations of disorders; advantages and disadvantages of crystalloid vs. colloid fluids 16. Endocrine disorders in the ICU—manifestations, diagnostic tests and management of adrenal insufficiency, thyroid storm, hypothyroidism, and DKA. 17. Principles of enteral and parental nutrition. 18. Gastrointestinal disorders—differential diagnosis, evaluation and management of upper and lower GI bleeding, acute pancreatitis, cirrhosis and its complications, and fulminant hepatic failure. 19. Hematology/oncology—causes and management of bleeding disorders, including proper use of blood products; management of neutropenic and immunocompromised patient; complications of bone marrow transplantation and their management. 20. Nervous system disorders—causes, evaluation and management of coma, cerebrovascular accidents, status epilepticus, delirium and other psychiatric disorders, weakness and neuromuscular disorders. Criteria and testing for brain death. Understand the application of post-arrest hypothermia. 21. Infectious diseases in the ICU—including principles of infection control and prevention of nosocomial infection; spectrum of activity and potential adverse effects of antimicrobial agents; causes and evaluation of fever in the ICU; criteria, causes, evaluation and management of septic shock. 22. Manifestations, evaluation and management of poisoning and drug overdose. 23. Disorders of temperature control including evaluation and management of hypo- and hyperthermia. 24. Recognition and management of acute allergic reactions, anaphylaxis, and immunecompromise disorders How Learning Objectives are met: 1. 2. 3. 4. 5. One-on-one interaction with ward attending during teaching and work rounds. Direct patient care Interaction with consultants and support staff Participation in regularly scheduled MRICU core conference Literature searches to answer clinical questions that arise on rounds or during patient care. 6. Interaction with the interdisciplinary health care team 7. Participation in daily radiology rounds