Case5 - University of California, Berkeley
advertisement

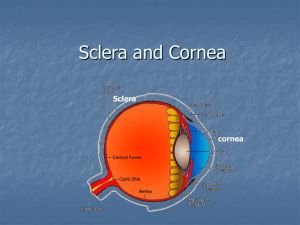
VS206C: Anatomy and Physiology of the Eye CASE 5: CORNEA TROUBLE (IMMUNOLOGY CASE 2) PART 1 Episode 1 Jill, a 32 year-old nurse, presents complaining of a painful watery right eye. She also notes that her vision in that eye is blurry and that she has photophobia. Jill has been a patient at this clinic for 8 years and has worn rigid gas permeable contact lenses for the past 5 years. Her previous records suggest that she is a compliant lens wearer, and that her most recent contact lens Rx (15 months ago) was -2.00 OD, -1.75 OS. Otherwise, her history is unremarkable. There is no history of eye disease in her family. She has not worn her contact lenses since the onset of symptoms 2 days ago. Vision with her spectacles is 20/30 OD, 20/25 OS. Slit lamp exam reveals conjunctival hyperemia and a 2 mm dendritic nasal corneal ulcer that borders the center of the cornea. The lesion stains positively for fluorescein. Rose bengal is taken up at the borders only. Treatment: Debridement and topical 1% trifluridine (Viroptic) eye drops. Culture results return confirming the suspicion of Herpes Simplex virus (HSV). Follow-up: The lesion stains negatively for fluorescein after 2 weeks, yet the epithelium appears abnormal in the area of the ulcer until 4 weeks after initiation of treatment. Examination after 8 weeks reveals that the cornea has completely healed. Visual acuity is 20/20 in that eye with no visible signs of previous infection. Episode 2 Eleven months later Jill returns with the same symptoms, which are even more severe. Slit lamp exam reveals a large geographic ulcer of 5 mm that covers the central cornea. Vision is 20/400 with difficulty. With antiviral therapy the cornea heals within 3 weeks. When she is examined 6 months later she is asymptomatic, the epithelium is intact, but a large dense stromal scar remains and the cornea has thinned in that area. Visual acuity is 20/200 O/D, 20/20 OS. Most important subjects to cover (in order of importance) Normal immune function - cellular immunity • T-cells (CD4+, CD8+) • MHC • Antigen presenting cells The immune response to viruses Latency Tolerance Wound healing Memory © Copyright 1998 by the School of Optometry, University of California, Berkeley. Written by S. Fleiszig, OD, PhD. GUIDING QUESTIONS Clinical Is contact lens wear involved? Is it surprising that someone who is a compliant lens wearer can have a corneal infection? Why is the vision blurry? Why is her vision 20/30 OD with her spectacles, does this necessarily mean that visual acuity is reduced? Would you expect this patient to have normal corneal sensitivity? Is it surprising that neither she nor her family has had any eye pathology? Is the other eye at risk? Where would you expect to find living virus particles in the cornea during infection? What is debridement and why is it done? Immunology How does the immune system respond to a viral infection (or other infections caused by intracellular pathogens)? Compare and contrast this to the immune response to extracellular bacteria, which occurred in the last case. Considering immunological memory, how can you have repeated episodes of infection with the same virus? Was the virus gone after the first episode? If not, where were the virus particles and why was there no active disease? Does the virus enter the stroma? Why, or why not? Why does the infection recur? What is the pathology behind all of the signs and symptoms of infection? How does the cornea heal after injury? Compare the healing responses after the two separate infectious episodes. (Why is the stroma scarred after the second episode and not after the first?) Why does it take so long for the epithelium to heal in these infections? Would you expect to find viable virus particles in the cornea for the entire 4 weeks that it took for the cornea to heal? How does antiviral drug therapy affect wound healing? References Books that you already have. Immunology Sunshine, Coico: (2 copies on reserve) • Biology of the T-lymphocyte • The role of MHC in the immune response •Activation of T and B cells by antigen • Control mechanisms in the immune response (includes tolerance and corticosteroids) Clinical Yanoff and Duker. Ophthalmology. (1 copy on reserve) • Viral keratitis Other References you may want to consult: 1. Forrester: The Eye (2000) (1 copy on reserve) • Antigen recognition, MHC and T-cell activation • Tolerance 2. Krachmer. Cornea. (3 volume set on reserve) • Herpes Simplex Keratitis • Corneal responses to infection • Modulation of corneal wound healing 3. Roitt’s essential immunology (1 copy on reserve) • Memory, acquired • Cell mediated immunity and intracellular organisms • Hypersensitivity • Memory Cells 4. Mim's Pathogenesis of Infectious Disease. Ch. 10. Failure to eliminate microbe (latency). (1 copy on reserve) © Copyright 1998 by the School of Optometry, University of California, Berkeley. Written by S. Fleiszig, OD, PhD. CORNEA TROUBLE - PART 2 Episode 3 Jill returns 3 months later complaining that her vision is getting worse and that her eye is very uncomfortable. Her visual acuity is now 20/800 OD. Slit lamp exam reveals interstitial keratitis and neovascularization of the stroma with an intact overlying epithelium. There is an anterior chamber reaction and ciliary flush. The eye is treated with a combined antiviral and corticosteroid ointment. Two weeks later all signs of inflammation and discomfort are gone except for a dense corneal scar and remnant ghost vessels. Her visual acuity in that eye has not improved, remaining at 20/800. Although she is relieved that her eye is now comfortable, she is extremely upset about her vision in that eye; particularly since it is interfering with her ability to fulfill her duties at work. Surgery Jill undergoes a penetrating keratoplasty 8 months later. Topics to cover Type II and III hypersensitivity reactions Autoimmunity Inflammation Principles of antiinflammatory agents Guiding questions What is the cause of episode 3? What does a corticosteroid do? Would it have been wise to use a corticosteroid during the earlier episodes (episodes 1 and/or 2)? Why is the use of both antiviral agents and corticosteroids controversial in this type of condition? At what point would you consider penetrating keratoplasty? What are the risks of this surgery? Could she return to contact lens wear after a graft? References Immunology Sunshine, Coico: Hypersensitivity reactions (type II and III), Autoimmunity, Inflammation (2 copies on reserve) Clinical Yanoff and Duker Other references you may want to consult: 1. Krachmer. Cornea. Type II and type III hypersensitivity reactions in the cornea. 2. Forrester: The Eye. (2002) (1 copy on reserve) Anti-inflammatory drugs 3. Pepose. Ocular infection and immunity. (1 copy on reserve) Chemical mediators of inflammation 4. Parslow, Stites, et al. Medical immunology. (1 copy on reserve) Inflammation © Copyright 1998 by the School of Optometry, University of California, Berkeley. Written by S. Fleiszig, OD, PhD. 5. http://nic.sav.sk/logos/books/scientific/node4.html © Copyright 1998 by the School of Optometry, University of California, Berkeley. Written by S. Fleiszig, OD, PhD. CORNEA TROUBLE - PART 3 Episode 4 Within a few months it becomes clear that the corneal graft is being rejected. She develops pronounced neovascularization, and the entire cornea becomes densely opaque. Topics to cover Transplant rejection Immunoprivilege of the eye and why corneal transplants are usually successful ACAID (Anterior Chamber Associated Immune Deviation) Guiding questions What is the mechanism for graft rejection? Why are corneal grafts generally more successful than other organ transplants? Are there any special risks in patients who have had HSV keratitis? How about this particular patient? Would it be wise to consider a second graft? References Sunshine, Coico: Transplant immunology (2 copies on reserve) http://www.karger.com/gazette/64/streilein/index.htm Other material you may want to consult: 1. Pepose. Ocular infection and immunity. (1 copy on reserve) • Corneal allograft rejection • ACAID (Anterior chamber associated immune deviation) • Regional immunology of the eye. 2. Kanski: Clinical Ophthalmology. (2 copies on reserve) • Penetrating keratoplasy © Copyright 1998 by the School of Optometry, University of California, Berkeley. Written by S. Fleiszig, OD, PhD.