REVISION_NOS1_Final
advertisement

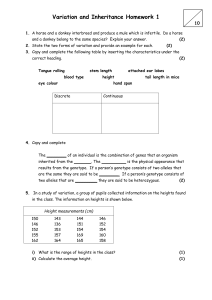
NOS1 Influences Verbal Intelligence And Working Memory In Both Patients With Schizophrenia And Healthy Controls. Authors Gary Donohoe D.Clin.Psych, Ph.D.1,2, James Walters MRCPsych, BM3, Derek W. Morris Ph.D.1, Emma M. Quinn M.Sc.1, Róisín Judge B.A.1, Nadine Norton Ph.D.3, Ina Giegling Ph.D.4, Annette M. Hartmann Ph.D.4, Hans-Jürgen Möller M.D.5, Pierandrea Muglia M.D.6, Hywel Williams Ph.D.3, Valentina Moskvina Ph.D.3, Rosemary Peel M.Sc.1, Therese O’Donoghue M.Sc.1,2, Michael J Owen FRCPsych, Ph.D.3, Michael C. O’Donovan FRCPsych, Ph.D.3, Michael Gill MRCPsych., M.D. 1,2 , Dan Rujescu M.D.4, Aiden Corvin MRCPsych., Ph.D.1,2. Affiliations 1 Neuropsychiatric Genetics Research Group, Dept of Psychiatry & Institute of Molecular Medicine, Trinity College Dublin, Ireland. 2 Trinity Institute of Neuroscience, Trinity College Dublin 3 Department of Psychological Medicine, School of Medicine, Cardiff University, Heath Park, Cardiff, UK. 4 Molecular and Clinical Neurobiology, Ludwig-Maximilians-University, Munich, Germany. 5 Department of Psychiatry, Ludwig-Maximilians-University, Munich, Germany. 6 Medical Genetics, GlaxoSmithKline R&D, Verona, Italy. Address for correspondence Dr. Gary Donohoe. Neuropsychiatric Genetics Research Group, Dept of Psychiatry, Trinity Health Sciences Building, St. James’s Hospital, Dublin 8. Telephone +353 1 896 2467 Fax +353 1 896 3405 E-mail Gary.Donohoe@tcd.ie Word count: 4485 Number of Tables: 2 Number of Figures: 2 Supplemental Files: 1 ABSTRACT Background: Human and animal studies have implicated the gene NOS1 in both cognition and schizophrenia susceptibility. Objectives: To investigate whether a potential schizophrenia risk SNP (rs6490121) identified in a recent genome-wide association study (O’Donovan et al., PMID 18677311) negatively influences cognition in patients with schizophrenia and healthy controls. Design: A comparison of both cases and controls grouped according to NOS1 genotype (GG v AG v AA) on selected measures of cognition in two independent samples. Setting: Unrelated patients from general adult psychiatric inpatient and outpatient services and unrelated healthy volunteers from the general population were ascertained. Participants: Patients with DSM-IV diagnosed schizophrenia and healthy controls from independent samples of Irish (n=349 cases and n=230 controls) and German (n=232 cases and n=1344 controls) nationality. Method: We tested for association between NOS1 rs6490121 and cognitive functions known to be impaired in schizophrenia (IQ, episodic memory, working memory, and attentional control) in the Irish sample. We then sought to replicate significant results in the German sample. Results: A main effect of NOS1 genotype on verbal IQ and working memory was observed in Irish samples where the homozygous carriers of the schizophrenia risk ‘G’ risk allele performed poorly compared with the other genotype groups. These findings replicated in the German sample, again with the GG genotype carriers performing below other genotype groups. Post-hoc Analysis of additional IQ measures (Full scale and Performance IQ) in the German sample revealed that NOS1 GG carriers underperformed on these measures also. Discussion: NOS1 is associated with clinically significant variation in cognitive. Whether this is a mechanism by which SZ risk is increased (e.g. via an influence on cognitive reserve) is yet to be confirmed. Introduction Schizophrenia (SZ) is a disorder of substantial heritability (~80%), but uncertain underlying pathophysiology (1). Despite some progress, most of the variance in SZ susceptibility attributable to genetic factors remains to be identified (2). A number of recent studies, exploiting high-throughput technologies investigating structural and genomic sequence variation in large SZ samples, have identified more consistent support for several susceptibility loci (3-5). As genomic data emerges, an important question is how these variants increase disease liability, and whether they are only relevant to the neurobiology of schizophrenia, or to neurodevelopment more generally (6-7). One putative schizophrenia risk gene is Nitric Oxide Synthase (NOS1, also known as neuronal NOS or nNOS; OMIM:163731), which maps to chromosome 12q24 and synthesises nitric oxide (NO) in both the central and peripheral nervous system. NO is a highly reactive messenger molecule, which diffuses freely across membranes stimulating guanylyl cyclase and modifying protein structure with multiple roles in immune, cardiac and neurological function. NO is produced by different nitric oxidase synthetase (NOS) enzymes including neuronal NOS and transported to different cellular compartments by adaptor proteins to minimize non-specific interactions. Transcription of NOS1 involves 12 alternate untranslated first exons and coding regions consisting of 28 exons covering 240KB. Following modest linkage support to the NOS1 region (8-11), four of five published NOS1 candidate gene association studies suggest evidence of association with SZ (12-15) with the exception being Liou et al (16). Moreover, in their SZ genome wide association study (GWAS) of 479 cases and 2937 controls, O’Donovan and colleagues (4) identified a single nucleotide polymorphism (SNP) at the NOS1 locus (rs6490121) as being one of twelve SNPs with strong initial statistical evidence for association (p=9.82 X 10-6). The same allele at this SNP was significantly associated in a replication sample of 1664 cases and 3541 controls of European Ancestry, but not in a sample of mixed European and Asian ancestry (4). Functional evidence for involvement of NO in SZ comes from studies showing abnormal distribution of nitrinergic neurons in frontal and temporal lobes in SZ (2324); increased NO metabolites in the serum of SZ patients (25-27); and post mortem increased NOS1 mRNA in prefrontal cortex of patients (28). Neurally generated NO displays many of the properties of a neurotransmitter and is involved in processes of potential relevance to SZ including synaptogenesis, long term potentiation, neurotransmitter release, synaptic plasticity, blood flow and cell death (21-22). These functions are dependent on the delivery and localization of NOS1 to multiple intracellular locations by specific adaptor proteins. Presynaptically, NOS1 is linked to Nitric oxide synthase 1 (neuronal) adaptor protein (NOS1AP) (OMIM: 605551) and forms a complex with Synapsin, which is involved in the assembly of synaptic vesicle clusters and synaptogenesis. The genes NOS1AP and SYN2 (OMIM: 600755) have both been implicated in SZ by genetic association studies (17-19; 88-89). Postsynaptically, NOS1 is coupled to N-methyl-D-aspartate (NMDA) receptors through Post Synaptic Density-95 (PSD95), representing another potential mechanism for involvement in SZ susceptibility. Molecular pathway analysis of structural variants implicated in SZ by Walsh et al (20) identified a significant excess of disrupted genes involving the NO signalling pathway. Taken together, these studies provide support for the involvement of NO signalling in SZ. In mouse models, NOS1 knock-outs have repeatedly been associated with variance in cognition (29-30). Notably, the PCP-induced cognitive and behavioural deficits that model SZ symptoms (including pre-pulse inhibition, habituation of acoustic startle, latent inhibition, spatial learning, spatial reference memory, and working memory), can all be prevented by interfering with the production of NO (31-40). In patients with SZ, Reif et al. (41) report that two of four genetic markers tested at the NOS1 loci, were associated with variance in performance on a measure of pre-frontal function (the Continuous Performance Task) in terms of behavioural performance, P300 peak amplitude and response latency. Whether this represents a specific or more general effect on cognition, or impacts cognition in the general population is unknown. The purpose of this study was to investigate the impact of NOS1 on cognition in SZ and control populations. We selected a single SNP at NOS1 (rs6490121) from the initial GWAS study by O’Donovan et al. (4) to which our cases had contributed as replication samples. We chose this SNP alone as the only SNP in O’Donovan et al. (4) that surpassed a significance threshold of p<10-5, and replicated with the same allele “G” in the European sample. We hypothesised that the genotypes carrying the risk allele would be associated with poorer performance on a selected set of cognitive domains typically impaired in SZ, namely IQ, episodic and working memory, and attentional control (42). Method Sample characteristics Irish patient and control samples (Discovery samples): This sample consisted of 349 cases and 230 controls. Ninety one of the case participants were genotyped as part of the prior GWAS study (4), the remaining case participants and all control samples were independent of that study. Cases consisted of clinically stable patients with a DSM-IV diagnosis of SZ (n=294) or schizoaffective disorder (n=55) recruited from five sites across Ireland. Inclusion criteria required that participants were aged 18 to 65 years, had no history of co-morbid psychiatric disorder, substance abuse in the preceding six months, or prior head injury with loss of consciousness or a history of seizures. Diagnosis was confirmed by trained psychiatrists using the Structured Clinical Interview for DSM-IV Axis 1 Diagnoses (SCID; 43). Additional diagnostic details and clinical sample characteristics ascertained at time of interview including symptom severity (SANS/SANS; 44-45) and medication dosage are detailed elsewhere (46). The healthy control sample was recruited on the basis of responses to local media advertisements. Control participants were only included if they were aged between 18 and 65 and satisfied, based on clinical interview, the criteria of having no history of major mental health problems, intellectual disability or acquired brain injury, and no history of substance misuse in the preceding six months based on self report. Control participants were also excluded from the study if they reported having a 1st degree relative with a history of psychosis. All patients and control assessments were conducted in accordance with the relevant ethics committees’ approval from each participating site. All patients and controls were of Irish ancestry (i.e. four grandparents born in Ireland) and all provided written informed consent. German patient and control samples (Replication sample) The German sample consisted of 240 clinically stable patients with a DSM-IV diagnosis of SZ and 1344 healthy controls, all of whom were genotyped as part of the previous study (4). Patients were ascertained from mental health services in the Munich area and all participants provided written informed consent. Inclusion criteria were a diagnosis of SZ (over 6 month symptom duration) and age 18-65. Exclusion criteria included a history of head injury or neurological diseases. Detailed medical and psychiatric histories were collected, including a clinical interview using the Structured Clinical Interview for DSM-IV (SCID; 43), to evaluate lifetime Axis I and II diagnoses. Four physicians and one psychologist rated the SCID interviews and all measurements were double-rated by a senior researcher. In cases, 68% were of strict German descent (all 4 grandparents born in Germany) and the other 32% were German Caucasian. Of the 240 participants 216 completed the full WAIS-R assessment and 232 a further comprehensive neuropsychological battery. Healthy control participants of German descent (all 4 grandparents German) were randomly selected from the general population of Munich, Germany, and contacted by mail. Control patients for this study were only included if aged between 18 and 65. To exclude subjects with central neurological diseases and psychotic disorders or subjects who had first-degree relatives with psychotic disorders, several screenings were conducted before the volunteers were enrolled in the study. First, subjects who responded were initially screened by phone for the absence of neuropsychiatric disorders. Second, detailed medical and psychiatric histories were assessed for both themselves and their first-degree relatives by using a semi-structured interview. Third, if no exclusion criteria were fulfilled, they were invited to a comprehensive interview including the Structured Clinical Interview for DSM-IV (SCID I and SCID II; 43,47) to validate the absence of any lifetime psychotic disorder. Additionally, the Family History Assessment Module (48) was conducted to exclude psychotic disorders among their first-degree relatives. A neurological examination was also conducted to exclude subjects with current CNS impairment. In the case of volunteers older than 60 years, the Mini Mental Status Test (49) was performed to exclude subjects with possible cognitive impairment. All of the 1344 control participants completed the full WAIS-R assessment and 364 completed tests from a further extensive neuropsychological battery. Cognitive assessment This study was designed so that identical, or near identical, tests of the phenotypes of general cognitive function (IQ), episodic memory, working memory, and attention were used for both the Irish discovery samples and the German replication samples. Only one verbal and one visuo-spatial measure for each cognitive function was tested in the Irish samples. Replication in the German sample was then sought for the cognitive functions showing significant association in the discovery sample. General cognitive functioning (IQ) was measured in the Irish sample using selected subtests (Vocabulary, Similarities, Block Design and Matrix Reasoning) from the Wechsler Adult Intelligence Scale, 3rd edition (WAIS-III; 50), yielding a full scale, verbal and performance IQ. For the German sample, IQ was indexed by the German version of the Wechsler Adult Intelligence Scale, revised edition (51) using all available 11 verbal/performance subtests (Vocabulary, comprehension, information, digit span, arithmetic, similarities, block design, picture completion, picture arrangement, object assembly, digit symbol coding). Verbal and visual Episodic memory was assessed in the Irish samples using the Logical memory and Faces subtests respectively from the Wechsler Memory Scale, 3rd edition (WMS-III; 52) and in the German sample using the Logical memory and Visual memory score from the German version of the Wechsler Memory Scale- Revised (53, 54). Verbal and spatial Working memory was assessed in the Irish samples using the Wechsler Letter Number Sequencing task (WMS-III; 52) and the Spatial working memory task from the Cambridge Automated Neuropsychological Test Battery (CANTAB SWM; 55). In the German samples, working memory was measured using the composite Digit Span and Spatial Span score from the WMS-R and the N-back task (NIMH-version, 56). Attentional control was assessed in the Irish sample using the Continuous performance task, identical pair’s version (CPT-IP, 57) and in the German sample using the Continuous performance task 3-7 version (58). Full descriptions of all memory and attention tasks are provided in Supplemental file 3. Genotyping of samples The SNP rs6490121 was genotyped in the German sample and a proportion of the Irish sample using the Sequenom iPLEX Gold system (further details are provided in (4)). The call rate for the iPLEX genotyping was >99% and all Irish and German case and control samples were in Hardy-Weinberg Equilibrium (HWE; p>0.05). The remainder of the Irish sample (n=529) was genotyped using a Taqman® SNP Genotyping Assay on a 7900HT Sequence Detection System (Applied Biosystems). The call rate for the Taqman genotyping was >95% and both case and control samples were in HWE (p>0.05). Along with the Irish samples, a number of HapMap CEU DNA samples (www.hapmap.org) were genotyped for rs6490121 for quality control purposes and were all found to be concordant with available online HapMap data for this SNP. Statistical analyses Association between NOS1 rs6490121 and the cognitive intermediate phenotypes of general cognitive function, episodic memory, working memory, and attentional control was tested using a general factorial design in SPSS 14 (SPSS, 2005). In the original paper identifying this variant there was no difference in genotypic versus allelic model; as there was no evidence on which to test a specific dominant or recessive model, and as sample sizes allowed, our analysis was based on a comparison of all three genotype groups. NOS1 genotype (GG versus AG versus AA) and diagnosis (cases versus controls) were entered as fixed effects. Scores for each neuropsychological subtest were entered as the dependent variables, with age and gender included as covariates as appropriate. Results Clinical and demographic characteristics by genotype for each sample appear in table 1. For the Discovery control sample, NOS1 genotypes were not associated with age, gender, or years in education. For the patient group, AA genotype carriers were observed to be older than the AG by an average of four years (t=-2.94; uncorrected p=.026); the GG group did not differ significantly in age from the other genotype groups. To investigate whether possible differences in symptom severity rating between genotype groups might influence cognitive performance in cases we conducted a principal components analysis with varimax rotation of all SAPS and SANS yielding three factors of positive, negative and disorganised symptoms (see table 1 and supplemental table 1). We did not observe any differences on any of the symptom factors associated with genotype. Neither did we observe difference in medication dosage associated with NOS1 genotype (all p values >0.05). A similar analysis of PANSS scores in the German sample also failed to identify any differences in symptom severity associated with NOS1; medication dosage was similarly non-significant (all p values >.05). TABLE 1 HERE NOS1 and general cognitive ability Analysis of verbal IQ in the Irish sample revealed a significant overall effect of genotype (see table 2). Tukey post hoc analysis revealed that this effect was driven by differences between GG and AA groups (t=-6.36; p=.04). An effect size estimate (partial ή2) suggests that genotype explains ~2% in cases and ~3.5% in controls. In clinical terms, carriers of the risk GG allele performed on average 5-6 standard score verbal IQ points below carriers of AG and AA genotypes (see Figure 1). No genotype by diagnostic group interaction was observed (even though, as expected, cases performed significantly below controls on this and all other cognitive tests, see Table 2). Although the same general pattern of results were observed for performance and full scale IQ scores, these differences were not significant (p>.05). TABLE 2 HERE Analysis of Verbal IQ in the German sample also revealed a significant overall effect of genotype (see table 2), with carriers of the risk GG allele performing significantly below AA and AG carriers. Based on post hoc analysis, the largest difference was between the GG and AG genotype groups (2.87; p=.012), with the difference between GG and AA groups just failing to achieve significance (t=2.34; p=.051). In this sample an interaction effect with affected status was also observed (F=11.51; p<.00001); as illustrated in Figure 1, the association with genotype appears to be strongest in cases. An effect size estimate (partial ή2) suggests that genotype explains ~5% of variance in Verbal IQ in cases and 0.2% in controls. FIGURE 1 HERE Following this replication of association between NOS1 genotype and Verbal IQ, we investigated post-hoc whether NOS1 was also associated with the two other indices of IQ in the German sample – Performance and Full scale IQ. A similar pattern of differences associated with genotype was observed (see Table 2). Genotype by diagnosis interactions were observed for both scores (Performance IQ: F=11.52; p<.0001; Full scale IQ: 8.95; p=.0002), such that the effect of genotype was apparent in cases only (see Figure 1). For cases the estimate of effect size was 6.9% for Performance IQ and 6.4% for Full scale IQ. As an additional secondary analysis, we further sought to determine whether the overall effect of genotype was comparable when cases and controls were considered separately. For the Irish samples, Verbal IQ was not significantly associated with NOS1 when cases and controls were considered individually (P>.05), suggesting insufficient power to analyse these samples separately. In the German sample, the GG genotype was associated with significantly poorer verbal IQ in patients (F=5.54; p=.005) but not controls; this pattern of association in patients but not controls was also observed for Performance IQ in patients (F=7.84; p=.001) and Full scale IQ in patients (F=7.26; p=.001). NOS1 and working memory performance For working memory, we observed a significant difference associated with genotype in verbal working memory as measured in the Irish samples by scores on the WMS Letter number sequencing task (see Table 2). While the association was significant as a main effect (F=4.02; 0=.02), as figure 2 illustrates, and a statistical interaction of genotype by diagnosis confirms, this association is clearly been driven by differences in the control group. For the control group, the GG risk allele carriers performed 3 scaled score points (1 standard deviation based on norms for the test) lower than AA on this measure of verbal working memory, with the between group difference significant between GG carriers and both other genotype groups (GG<AG: t=-2.21; 0=.013; GG<AA: t=-3.05; p=.0002). A significant, main effect of genotype was also observed with the spatial working memory task used (see Table 2), in the absence of an interaction with diagnosis. Post hoc analysis reveals the difference as largest between the AG and AA groups (t=.31; p=.02); this is illustrated in Figure 3. Using two different measures of working memory in the German sample, the GG risk allele was again associated with poorer performance on both measures (see Table 2). While association with genotype was observed as a main effect, in the absence of a statistical interaction with diagnosis, the effect size appeared slightly larger in cases than controls (N-back partial ή2 =2.2% versus 1.1%). We again sought to determine whether the overall effect of genotype was comparable when cases and controls were considered separately. For the Irish samples, differences on both working memory tasks were associated with NOS1 genotype in controls (LN sequence: F2,163=9.02; p=.0002; SWM task F2,163=4.99; p=.008) but not patients (P>.05). When the German case and control samples were considered separately, the association was seen in the patient group but not the control group on the Wechsler working memory score (F=5.49; p=.005); for the N-back task the effects of genotype were no longer apparent when cases and controls were considered separately. NOS1 genotype and memory and attentional control In the Irish sample no differences associated with NOS1 genotype was observed on either the verbal or nonverbal memory tests used (the Logical memory and CANTAB PAL tests respectively). Similarly, when the effects of NOS1 on attention were investigated using the IDED task (scores for block 8) and the CPT-IP task (using d’ values for each of the three conditions) no significant associations were observed. As no association with NOS1 genotype was observed in the Irish sample (all P>.05) we did not investigate these aspects of cognition in the German samples. Discussion Variants at NOS1 have previously been associated with both increased SZ risk and variation in cognitive performance. The involvement of NOS1 in cognition is well established from animal models, with the NMDA-NO-cGMP signaling cascade being linked to neurotransmitter release and synaptic plasticity in multiple genetic and pharmacological studies (84). From the known biology of SZ, NOS-driven negative feedback on NMDA receptor function and inhibition of synaptic reuptake of dopamine positions it at the crossroads between two messenger systems whose mutual regulation is a leading hypothesis for SZ (21). This study shows that a NOS1 SNP, identified as a putative risk variant by a recent SZ GWAS study, is associated with variation in verbal intelligence and working memory in two large independent samples. Significant issues for studies addressing the cognitive effects of previously identified risk variants in SZ have included small sample size, lack of a suitable replication sample within the same study design, and a heavy multiple testing burden. One approach to the issue of multiple testing is statistical (e.g. Bonferroni) correction; however, the expected effects size based on previous molecular studies of cognition, and the non-independence of measures of cognition, serve to limit the value of these statistical approaches. Instead, our approach was to seek independent replication of significant results using two large independent case and control samples both of which contributed to the original identification of the NOS1 rs6490121 variant studied here (4). Secondly, only a tightly selected group of cognitive functions (IQ, memory, and attention), each measuring a core cognitive deficit in schizophrenia, were selected for analysis on the basis of their availability in both samples. Finally, this study was based on a single associated allele and results obtained were in the same expected direction in both samples, with homozygous G carriers - the associated allele in the original GWAS study performing more poorly. The utility of the cognitive intermediate phenotypes approach in schizophrenia has been well articulated as potentially representing less complex genetic architecture than the broader disease phenotype, often shared by unaffected relatives, and thus capable of increasing power to detect genetic effects (83). While verbal IQ and working memory are themselves complex processes, likely to be influenced by many genetic variants (e.g. DTNBP1; 60-62), the observed impact of NOS1 genotype on cognition is not simply statistically significant. In both samples the size of the association for verbal IQ in clinical terms is between 0.3 and 0.5 standard deviations. For WM memory the differences between genotype groups represent a difference of approximately 1 standard deviation. By comparison with findings of association between cognitive performance and other gene variants, the size of effect observed is considerably higher than that reported in the recent meta-analysis of COMT and IQ (82), but comparable to reports of the association between Dysbindin and ‘g’ in patients and controls (60) and spatial working memory in patients (61). While the overall pattern was the same across the Irish and German samples, the effect size varied between patients and healthy controls. Such differences may reflect differences related to sample size or ascertainment strategy (for example, the somewhat better than expected overall performance of German patients and Irish controls, respectively). That NOS1 genotype was associated with both verbal IQ and working memory but not attentional control is noteworthy. We have previously argued that deficits in working memory, unlike attentional control, correlate with the general cognitive decline apparent in schizophrenia (63). Working memory has been characterised as the common factor in Spearman’s ‘g’, a measure of general cognitive function derived from the statistical correlation between cognitive tasks. Alternatively, working memory may simply be another name for ‘g’ given the overlap between working memory and psychometric tests of ‘g’ (64). This is supported by the evidence that various measures of working memory correlate with ‘g’ at a level corresponding to the reliability of the measure used (65-67). Our association with indices of both (verbal) intelligence and working memory is consistent with this evidence, and suggests that for NOS1 verbal IQ and working memory may represent overlapping, or at least psychometrically similar, constructs. Providing empirical support for this point, co-varying for the influence of either cognitive variable resulted in the association of the other with NOS1 becoming non-significant (See supplementary table 2). These findings are consistent with cognitive studies in both animal and human models of NOS1 where a general rather than specific impact on cognition is suggested (29-30; 36-39; 41,41). NOS1 & Cognition: Molecular mechanism The implicated SNP (rs6490121), located in intron 10 of NOS1, has no obvious functional impact and may reflect a proxy association with another causal variant(s). Based on HapMap CEU data, rs6490121 is not in high LD (r2 >0.8) with any other common SNP at this locus. NOS1 is characterized by complex transcriptional regulation. Twelve alternative first exons have been identified (exon 1a – 1l; 68). Exon 1d and 1f, along with the exon 1g transcript, are the most commonly expressed NOS1 transcripts in the brain (69). A dinucleotide variable number tandem repeat (VNTR) is located in the core promoter region of exon 1f (70). The short alleles of this variant, termed NOS1 Ex1f VNTR, are associated with decreased transcriptional activity of the NOS1 exon 1f promoter, alterations in the neuronal transcriptome impacting on other putative SZ susceptibility genes (RGS4 and GRIN1) and affects electrocortical measures of prefrontal functions involved in cognitive control (81). Interestingly, data from our laboratory indicates that the risk G allele of rs6490121 is in LD (D = 0.70, r2 = 0.26, HapMap CEU) with the short alleles of NOS1 Ex1f VNTR, highlighting a putative functional mechanism of cognitive performance dysregulation at NOS1 for future study. To explore potential mechanisms by which NO could exert an effect on cognitive processes we screened experimentally validated Protein-Protein Interactions (PPI’s) of NOS1 using the PPI databases (STRING (85), DIP, Interact (86) and BIND (87)) and identified 19 confirmed human binary interactions. With potential relevance to SZ susceptibility are genes involved in pre-synaptic synaptogenesis (NOS1AP and Syntrophin (SNTA1) (OMIM: 601017)) and post-synaptically through the PSD-95NOS1 receptor complex including direct NOS1 interaction with GRIN1 and GRIN2b. Elements of PSD-95 signaling cascades have been targeted in SZ genetic association studies including erbB4/Neuregulin signaling and the NMDA receptor complex which is involved in long-term potentiation, memory and learning. There is some support from these studies for involvement of GRIN2B, GRM3, erbB4 and NRG1 in SZ susceptibility. Negative studies have been reported for PSD-95 (Kawashima et al, 2006; Tsai et al, 2006) and NOS1AP (Zheng et al, 2005; Puri et al, 2006a; Puri et al, 2006b; Fang et al, 2008). DeQuervain & Papassotiropoulus (2006) identified variation at GRIN2B and GRM3 as genes contributing to the memory formation signaling cascade involved in episodic memory performance. Additionally, NOS1 activators Calmodulin and PKCA (protein kinase C alpha type), although not directly associated with SZ risk, have also been associated with memory in humans (de Quervain & Papassotiropoulos, 2006; Huentelman et al, 2007). More systematic studies of genes involved in NOS1 regulation and adaptor proteins linked to synaptic function and plasticity are warranted and we plan to screen functional variants at genes from these pathways for additive and epistatic effects on cognition and SZ susceptibility. NOS1 and schizophrenia: functional implications The findings reported here raise interesting questions. Is NOS1 a SZ susceptibility gene? Or perhaps a modifier gene that influences cognitive deficits without altering disease liability (6; 71)? The present data do not provide evidence one way or another for association between NOS1 and SZ. Including the additional Irish samples into the meta-analysis of NOS1 by O’Donovan et al. (4) does not change the significance of the findings of that study (i.e. NOS1 remains moderately associated with SZ in the European only samples [p=.005, 2-tailed], but not in the total European and Asian sample combined). One interpretation of these findings is in terms ‘cognitive reserve’, the idea that individuals with lower IQ are more vulnerable to, or more likely to express the features of, neurodevelopmental, neurodegenerative, or acquired brain injury (72). In SZ, evidence of low intelligence as a risk factor is long established, with both prospective birth cohort studies (73-75) and conscription studies (76-80) consistently reporting lower intelligence in children and adolescence who will later develop SZ. However, differences in education (often used as a proxy measure of premorbid IQ) were only observed as a trend in the Irish samples, and were absent in the German samples, thus only weakly supporting lowered pre-morbid IQ as the mechanism of risk associated with NOS1. Instead, given the association between NOS1 and cognition in both patients and controls presented here, a more parsimonious explanation is that NOS1 influences cognition generally, an impact which is observed to some extent in both cases and controls. In terms of the intermediate phenotype aproach in psychiatric genetics, these findings highlight the benefits of cognitive studies of putative SZ variants for understanding the genetics of fundemental cognitive and neurodevelopmental processes. It remains an open question as to the degree to which these genes are coding for disease specific processes, either as mediated though or independent of the effects on cognition reported here. Acknowledgements The authors sincerely thank all patients would contributed to this study and all staff who facilitated their involvement. Recruitment of the patients from Munich, Germany was partially supported by GlaxoSmithKline (GSK). We are grateful to the Genetics Research Centre GmbH, an initiative by GSK and LMU. Genotyping of the German sample was funded by grants from the MRC and Wellcome Trust. Recruitment and genotyping of the Irish sample was supported by the Wellcome Trust and Science Foundation Ireland (SFI). Dr. Donohoe was supported by an SFI research frontiers grant and a NARSAD young Investigator award. Dr. Walters was supported by an MRC clinical training fellowship. References 1. Cardno AG, Gottesman II. Twin studies of schizophrenia: from bow-and-arrow concordances to star wars Mx and functional genomics. Am J Med Genet. 2000; 97(1):12-7. 2. Sullivan PF. Schizophrenia genetics: the search for a hard lead. Curr Opin Psychiatry. 2008; 21(2):157-60.ISC, 2008; 3. International Schizophrenia Consortium. Rare chromosomal deletions and duplications increase risk of schizophrenia. Nature. 2008; 455(7210):237-41. 4. O'Donovan MC, Craddock N, Norton N, Williams H, Peirce T, Moskvina V, Nikolov I, Hamshere M, Carroll L, Georgieva L, Dwyer S, Holmans P, Marchini JL, Spencer CC, Howie B, Leung HT, Hartmann AM, Möller HJ, Morris DW, Shi Y, Feng G, Hoffmann P, Propping P, Vasilescu C, Maier W, Rietschel M, Zammit S, Schumacher J, Quinn EM, Schulze TG, Williams NM, Giegling I, Iwata N, Ikeda M, Darvasi A, Shifman S, He L, Duan J, Sanders AR, Levinson DF, Gejman PV; Molecular Genetics of Schizophrenia Collaboration, Gejman PV, Sanders AR, Duan J, Levinson DF, Buccola NG, Mowry BJ, Freedman R, Amin F, Black DW, Silverman JM, Byerley WF, Cloninger CR, Cichon S, Nöthen MM, Gill M, Corvin A, Rujescu D, Kirov G, Owen MJ. Identification of loci associated with schizophrenia by genome-wide association and follow-up. Nat Genet. 2008 Jul 30. [Epub ahead of print] 5. Stefansson H, Rujescu D, Cichon S, Pietiläinen OP, Ingason A, Steinberg S, Fossdal R, Sigurdsson E, Sigmundsson T, Buizer-Voskamp JE, Hansen T, Jakobsen KD, Muglia P, Francks C, Matthews PM, Gylfason A, Halldorsson BV, Gudbjartsson D, Thorgeirsson TE, Sigurdsson A, Jonasdottir A, Jonasdottir A, Bjornsson A, Mattiasdottir S, Blondal T, Haraldsson M, Magnusdottir BB, Giegling I, Möller HJ, Hartmann A, Shianna KV, Ge D, Need AC, Crombie C, Fraser G, Walker N, Lonnqvist J, Suvisaari J, Tuulio-Henriksson A, Paunio T, Toulopoulou T, Bramon E, Di Forti M, Murray R, Ruggeri M, Vassos E, Tosato S, Walshe M, Li T, Vasilescu C, Mühleisen TW, Wang AG, Ullum H, Djurovic S, Melle I, Olesen J, Kiemeney LA, Franke B, Sabatti C, Freimer NB, Gulcher JR, Thorsteinsdottir U, Kong A, Andreassen OA, Ophoff RA, Georgi A, Rietschel M, Werge T, Petursson H, Goldstein DB, Nöthen MM, Peltonen L, Collier DA, St Clair D, Stefansson K, Kahn RS, Linszen DH, van Os J, Wiersma D, Bruggeman R, Cahn W, de Haan L, Krabbendam L, Myin-Germeys I; Genetic Risk and Outcome in Psychosis (GROUP). Large recurrent microdeletions associated with schizophrenia. Nature. 2008; 455(7210):232-6. 6. Fanous AH, Kendler KS. Genetics of clinical features and subtypes of schizophrenia: a review of the recent literature. Curr Psychiatry Rep. 2008; 10(2):164-70. 7. Mefford HC, Sharp AJ, Baker C, Itsara A, Jiang Z, Buysse K, Huang S, Maloney VK, Crolla JA, Baralle D, Collins A, Mercer C, Norga K, de Ravel T, Devriendt K, Bongers EM, de Leeuw N, Reardon W, Gimelli S, Bena F, Hennekam RC, Male A, Gaunt L, Clayton-Smith J, Simonic I, Park SM, Mehta SG, Nik-Zainal S, Woods CG, Firth HV, Parkin G, Fichera M, Reitano S, Giudice ML, Li KE, Casuga I, Broomer A,Conrad B, Schwerzmann M, Räber L, Gallati S, Striano P, Coppola A, Tolmie JL, Tobias ES, Lilley C, Armengol L, Spysschaert Y, Verloo P, De Coene A, Goossens L, Mortier G, Speleman F, van Binsbergen E, Nelen MR, Hochstenbach R, Poot M, Gallagher L, Gill M, McClellan J, King MC, Regan R, Skinner C, Stevenson RE, Antonarakis SE, Chen C, Estivill X, Menten B, Gimelli G, Gribble S, Schwartz S, Sutcliffe JS, Walsh T, Knight SJ, Sebat J, Romano C, Schwartz CE, Veltman JA, de Vries BB, Vermeesch JR, Barber JC, Willatt L, Tassabehji M, Eichler EE. Recurrent Rearrangements of Chromosome 1q21.1 and Variable Pediatric Phenotypes. N Engl J Med. 2008 Sep 10. [Epub ahead of print] 8. Abkevich V, Camp NJ, Hensel CH, Neff CD, Russell DL, Hughes DC, Plenk AM, Lowry MR, Richards RL, Carter C, Frech GC, Stone S, Rowe K, Chau CA, Cortado K, Hunt A, Luce K, O'Neil G, Poarch J, Potter J, Poulsen GH, Saxton H, Bernat-Sestak M, Thompson V, Gutin A, Skolnick MH, Shattuck D, CannonAlbright L. Predisposition locus for major depression at chromosome 12q2212q23.2. Am J Hum Genet. 2003; 73(6):1271-81. 9. Bailer U, Leisch F, Meszaros K, Lenzinger E, Willinger U, Strobl R, Gebhardt C, Gerhard E, Fuchs K, Sieghart W, Kasper S, Hornik K, Aschauer HN. Genome scan for susceptibility loci for schizophrenia. Neuropsychobiology. 2000; 42(4):175-82. 10. Bailer U, Leisch F, Meszaros K, Lenzinger E, Willinger U, Strobl R, Heiden A, Gebhardt C, Döge E, Fuchs K, Sieghart W, Kasper S, Hornik K, Aschauer HN. Genome scan for susceptibility loci for schizophrenia and bipolar disorder. Biol Psychiatry. 2002; 52(1):40-52. 11. DeLisi LE, Shaw SH, Crow TJ, Shields G, Smith AB, Larach VW, Wellman N, Loftus J, Nanthakumar B, Razi K, Stewart J, Comazzi M, Vita A, Heffner T, Sherrington R. A genome-wide scan for linkage to chromosomal regions in 382 sibling pairs with schizophrenia or schizoaffective disorder. Am J Psychiatry. 2002; 159(5):803-12. 12. Shinkai T, Ohmori O, Hori H, Nakamura J. Allelic association of the neuronal nitric oxide synthase (NOS1) gene with schizophrenia. Mol Psychiatry. 2002; 7(6):560-3. 13. Reif A, Herterich S, Strobel A, Ehlis AC, Saur D, Jacob CP, Wienker T, Töpner T, Fritzen S, Walter U, Schmitt A, Fallgatter AJ, Lesch KP. A neuronal nitric oxide synthase (NOS-I) haplotype associated with schizophrenia modifies prefrontal cortex function. Mol Psychiatry. 2006; 11(3):286-300. 14. Fallin MD, Lasseter VK, Avramopoulos D, Nicodemus KK, Wolyniec PS, McGrath JA, Steel G, Nestadt G, Liang KY, Huganir RL, Valle D, Pulver AE. Bipolar I disorder and schizophrenia: a 440-single-nucleotide polymorphism screen of 64 candidate genes among Ashkenazi Jewish case-parent trios. Am J Hum Genet. 2005; 77(6):918-36. 15. Tang W, Huang K, Tang R, Zhou G, Fang C, Zhang J, Du L, Feng G, He L, Shi Y. Evidence for association between the 5' flank of the NOS1 gene and schizophrenia in the Chinese population. Int J Neuropsychopharmacol. 2008; Jun 11[Epub ahead of print]. 16. Liou YJ, Tsai SJ, Hong CJ, Liao DL. Association analysis for the CA repeat polymorphism of the neuronal nitric oxide synthase (NOS1) gene and schizophrenia. Schizophr Res. 2003 Dec 1;65(1):57-9. 17. Brzustowicz LM, Simone J, Mohseni P, Hayter JE, Hodgkinson KA, Chow EW, Bassett AS. Linkage disequilibrium mapping of schizophrenia susceptibility to the CAPON region of chromosome 1q22. Am J Hum Genet. 2004; 74(5):1057-63. 18. Xu S, Guo S, Jiang X, Umezawa T, Hisamitsu T. The role of norepinephrine and nitric oxide in activities of rat arginine vasopressin neurons in response to immune challenge. Neurosci Lett. 2005; 383(3):231-5. 19. Lencz T, Lambert C, DeRosse P, Burdick KE, Morgan TV, Kane JM, Kucherlapati R,Malhotra AK. Runs of homozygosity reveal highly penetrant recessive loci in schizophrenia. Proc Natl Acad Sci U S A. 2007; 104(50):19942-7. 20. Walsh T, McClellan JM, McCarthy SE, Addington AM, Pierce SB, Cooper GM, Nord AS, Kusenda M, Malhotra D, Bhandari A, Stray SM, Rippey CF, Roccanova P, Makarov V, Lakshmi B, Findling RL, Sikich L, Stromberg T, Merriman B, Gogtay N, Butler P, Eckstrand K, Noory L, Gochman P, Long R, Chen Z, Davis S, Baker C, Eichler EE, Meltzer PS, Nelson SF, Singleton AB, Lee MK, Rapoport JL, King MC, Sebat J. Rare structural variants disrupt multiple genes in neurodevelopmental pathways in schizophrenia. Science. 2008; 320(5875):53943. 21. Harrison PJ, Weinberger DR. Schizophrenia genes, gene expression, and neuropathology: on the matter of their convergence. Mol Psychiatry. 2005; 10(1):40-68. 22. Ross CA, Margolis RL, Reading SA, Pletnikov M, Coyle JT. Neurobiology of schizophrenia. Neuron. 2006; 52(1):139-53. 23. Akbarian S, Viñuela A, Kim JJ, Potkin SG, Bunney WE Jr, Jones EG. Distorted distribution of nicotinamide-adenine dinucleotide phosphate-diaphorase neurons in temporal lobe of schizophrenics implies anomalous cortical development. Arch Gen Psychiatry. 1993; 50(3):178-87. 24. Akbarian S, Bunney WE Jr, Potkin SG, Wigal SB, Hagman JO, Sandman CA, Jones EG. Altered distribution of nicotinamide-adenine dinucleotide phosphatediaphorase cells in frontal lobe of schizophrenics implies disturbances of cortical development. Arch Gen Psychiatry. 1993; 50(3):169-77. 25. Taneli F, Pirildar S, Akdeniz F, Uyanik BS, Ari Z. Serum nitric oxide metabolite levels and the effect of antipsychotic therapy in schizophrenia. Arch Med Res. 2004 Sep-Oct;35(5):401-5. 26. Das I, Khan NS, Puri BK, Sooranna SR, de Belleroche J, Hirsch SR. Elevated platelet calcium mobilization and nitric oxide synthase activity may reflect abnormalities in schizophrenic brain. Biochem Biophys Res Commun. 1995; 212(2):375-80. 27. Yilmaz N, Herken H, Cicek HK, Celik A, Yürekli M, Akyol O. Increased levels of nitric oxide, cortisol and adrenomedullin in patients with chronic schizophrenia. Med Princ Pract. 2007; 16(2):137-41. 28. Baba H, Suzuki T, Arai H, Emson PC. Expression of nNOS and soluble guanylate cyclase in schizophrenic brain. Neuroreport. 2004; 15(4):677-80. 29. Kirchner L, Weitzdoerfer R, Hoeger H, Url A, Schmidt P, Engelmann M, Villar SR, Fountoulakis M, Lubec G, Lubec B. Impaired cognitive performance in neuronal nitric oxide synthase knockout mice is associated with hippocampal protein derangements. Nitric Oxide. 2004; 11(4):316-30. 30. Weitzdoerfer R, Hoeger H, Engidawork E, Engelmann M, Singewald N, Lubec G,Lubec B. Neuronal nitric oxide synthase knock-out mice show impaired cognitive performance. Nitric Oxide. 2004; 10(3):130-40. 31. Johansson, C., Jackson, D.M., Svensson, L., 1997. Nitric oxide synthase inhibition blocks phencyclidine-induced behavioural effects on prepulse inhibition and locomotor activity in the rat. Psychopharmacology (Berl.) 131, 167–173. 32. Johansson, C., Magnusson, O., Deveney, A.M., Jackson, D.M., Zhang, J., Engel, J.A., Svensson, L., 1998. The nitric oxide synthase inhibitor, l-NAME, blocks certain phencyclidine-induced but not d-amphetamine induced effects on behaviour and brain biochemistry in the rat. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 22, 1341– 1360. 33. Klamer D, Engel JA, Svensson L. The nitric oxide synthase inhibitor, L-NAME, block phencyclidine-induced disruption of prepulse inhibition in mice. Psychopharmacology (Berl). 2001;156(2-3):182-6. 34. Klamer D, Engel JA, Svensson L. Phencyclidine-induced behaviour in mice prevented by methylene blue. Basic Clin Pharmacol Toxicol. 2004; 94(2):65-72. 35. Klamer D, Pålsson E, Revesz A, Engel JA, Svensson L. Habituation of acoustic startle is disrupted by psychotomimetic drugs: differential dependence on dopaminergic and nitric oxide modulatory mechanisms. Psychopharmacology (Berl). 2004; 176(3-4):440-50. 36. Klamer D, Engel JA, Svensson L. The neuronal selective nitric oxide synthase inhibitor, Nomega-propyl-L-arginine, blocks the effects of phencyclidine on prepulse inhibition and locomotor activity in mice. Eur J Pharmacol. 2004; 503(1-3):103-7. 37. Klamer D, Engel JA, Svensson L. Effects of phencyclidine on acoustic startle and prepulse inhibition in neuronal nitric oxide synthase deficient mice.Eur Neuropsychopharmacol. 2005; 15(5):587-90. 38. Wass C, Archer T, Pålsson E, Fejgin K, Alexandersson A, Klamer D, Engel JA, Svensson L. Phencyclidine affects memory in a nitric oxide-dependent manner: working and reference memory. Behav Brain Res. 2006; 174(1):49-55. 39. Wass C, Archer T, Pålsson E, Fejgin K, Klamer D, Engel JA, Svensson L. Effects of phencyclidine on spatial learning and memory: nitric oxide-dependent mechanisms. Behav Brain Res. 2006;171(1):147-53. 40. Pålsson E, Fejgin K, Wass C, Engel JA, Svensson L, Klamer D. The amino acid L-lysine blocks the disruptive effect of hencyclidine on prepulse inhibition in mice. Psychopharmacology (Berl). 2007; 192(1):9-15. 41. Reif A, Herterich S, Strobel A, Ehlis AC, Saur D, Jacob CP, Wienker T, Töpner T, Fritzen S, Walter U, Schmitt A, Fallgatter AJ, Lesch KP. A neuronal nitric oxide synthase (NOS-I) haplotype associated with schizophrenia modifies prefrontal cortex function. Mol Psychiatry. 2006; 11(3):286-300. 42. Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 1998; 12(3):426-45. 43. First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders - Patient Edition. New York: Biometrics Research Department, New York State Psychiatric Institute; 1995. 44. Andreasen, 1984a N.C. Andreasen, Scale for the Assessment of Negative Symptoms/Scale for the Assessment of Positive Symptoms (Manual), University of Iowa Press, Iowa City (1984). 45. Andreasen, 1984b N.C. Andreasen, The Scale for the Assessment of Negative Symptoms (SANS), University of Iowa Press, Iowa City (1984). 46. Corvin A, Donohoe G, Nangle JM, Schwaiger S, Morris D, Gill M. A dysbindin risk haplotype associated with less severe manic-type symptoms in psychosis. Neurosci Lett. 2008; 431(2):146-9. 47. First MB, Spitzer RL, Gibbon M, Williams BW, Benjamin L. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). New York: Biometrics Research Department, New York State Psychiatric Institute; 1990. 48. Rice JP, Reich T, Bucholz KK, Neuman RJ, Fishman R, Rochberg N, Hesselbrock VM, Nurnberger JI, Jr., Schuckit MA, Begleiter H (1995): Comparison of direct interview and family history diagnoses of alcohol dependence. Alcohol Clin Exp Res 19:1018-23. 49. Folstein MF, Folstein SE, McHugh PR. Mini-Mental-Status-Test. Version: Kessler J, Folstein SE, Denzler P. Weinheim: Beltz; 1990. German 50. Wechsler D. Wechsler Adult Intelligence Scale, Third edition (WAIS-III). The Psychological Corporation: New York; 1997. 51. Tewes U. HAWIE-R Hamburg-Wechsler Intelligenztest fu¨r Erwachsene. Hogrefe: Goettingen: 1991. 52. Wechsler D. Wechsler Memory Scale, Third edition (WMS-III). The Psychological Corporation: New York; 1998. 53. Wechsler D. Wechsler Memory Scale – Revised. The Psychological Corporation: San Antonio: 1987. 54. Härting C, Markowitsch HJ, Neufeld H, Calabrese P, Deisinger K, Kessler J. Wechsler Memory Scale- Revised; German Version: Wechsler Gedächtnistest; Revidierte Fassung. Huber: Bern; 2000. 55. Cambridge Cognition. Cambridge Neuropsychological Test Automated Battery, expedio version (CANTABexpedio). Cambridge Cognition Ltd: Cambridge; 2003. 56. Egan MF, Goldberg TE, Kolachana BS, Callicott JH, Mazzanti CM, Straub RE, Goldman D, Weinberger DR. Effect of COMT Val108/158 Met genotype on frontal lobe function and risk for schizophrenia. Proc Natl Acad Sci USA 2006; 98:6917-6922 57. Cornblatt et al., 1988 B.A. Cornblatt, N.J. Risch, G. Faris, D. Friedman and L. Erlenmeyer-Kimling, The continuous performance test, identical pairs version (CPT-IP): new findings about sustained attention in normal families, Psychiatry Res. 1988; 26: 223–238. 58. Nuechterlein K, Asarnow R. 3-7 Continuous Performance Test. University of California: Los Angeles; 2004. 59. SPSS Inc. Statistical package for the social sciences (SPSS) version 14.0. Chicago: Illanois; 2005. 60. Burdick KE, Lencz T, Funke B, Finn CT, Szeszko PR, Kane JM, Kucherlapati R,Malhotra AK. Genetic variation in DTNBP1 influences general cognitive ability. Hum Mol Genet. 2006; 15(10):1563-8. 61. Donohoe G, Morris DW, Clarke S, McGhee KA, Schwaiger S, Nangle JM, Garavan H, Robertson IH, Gill M, Corvin A. Variance in neurocognitive performance is associated with dysbindin-1 in schizophrenia: a preliminary study. Neuropsychologia. 2007; 45(2):454-8. 62. Plomin R. Genetics, genes, genomics and g. Mol Psychiatry. 2003; 8(1):1-5. 63. Donohoe G, Clarke S, Morris D, Nangle JM, Schwaiger S, Gill M, Corvin A, Robertson IH. Are deficits in executive sub-processes simply reflecting more general cognitive decline in schizophrenia? Schizophr Res. 2006; 85(1-3):168-73. 64. Plomin R, Spinath FM. Genetics and general cognitive ability (g). Trends Cogn Sci. 2002; 6(4):169-176. 65. Engle RW, Tuholski SW, Laughlin JE, Conway AR. Working memory, shortterm memory, and general fluid intelligence: a latent-variable approach. J Exp Psychol Gen. 1999; 128(3):309-31. 66. Kyllonen PC, Is working memory capacity Spearman's g?. In: I. Dennis and P. Tapsfield, Editors, Human Abilities: Their Nature and Measurement, Erlbaum; 1996. 67. Stauffer, J.M. Cognitive-components tests are not much more than g: an extension of Kyllonen's analyses. J. Gen. Psychol. 1996; 193–205. 68. Boissel JP, Zelenka M, Gödtel-Armbrust U, Feuerstein TJ, Förstermann U.Transcription of different exons 1 of the human neuronal nitric oxide synthase gene is dynamically regulated in a cell- and stimulus-specific manner Biol Chem. 2003; 384(3):351-62. 69. Bros M, Boissel JP, Gödtel-Armbrust U, Förstermann U. Transcription of human neuronal nitric oxide synthase mRNAs derived from different first exons is partly controlled by exon 1-specific promoter sequences. Genomics. 2006; 87(4):463-73. 70. Hall AV, Antoniou H, Wang Y, Cheung AH, Arbus AM, Olson SL, Lu WC, Kau CL, Marsden PA. Structural organization of the human neuronal nitric oxide synthase gene (NOS1). J Biol Chem. 1994; 269(52):33082-90. 71. Meyer-Lindenberg A, Weinberger DR. Intermediate phenotypes and genetic mechanisms of psychiatric disorders. Nat Rev Neurosci. 2006; 7(10):818-27. 72. Barnett JH, Salmond CH, Jones PB, Sahakian BJ. Cognitive reserve in neuropsychiatry. Psychol Med. 2006; 36(8):1053-64. 73. Crow TJ, Done DJ, Sacker A. Childhood precursors of psychosis as clues to its evolutionary origins. Eur Arch Psychiatry Clin Neurosci. 1995; 245(2):61-9. 74. Kremen WS, Buka SL, Seidman LJ, Goldstein JM, Koren D, Tsuang MT. IQ decline during childhood and adult psychotic symptoms in a community sample: a 19-year longitudinal study. Am J Psychiatry. 1998; 155(5):672-7. 75. Cannon M, Caspi A, Moffitt TE, Harrington H, Taylor A, Murray RM, Poulton R. Evidence for early-childhood, pan-developmental impairment specific to schizophreniform disorder: results from a longitudinal birth cohort. Arch Gen Psychiatry. 2002; 59(5):449-56. 76. David AS, Malmberg A, Brandt L, Allebeck P, Lewis G. IQ and risk for schizophrenia: a population-based cohort study. Psychol Med. 1997; 27(6):131123. 77. Davidson M, Reichenberg A, Rabinowitz J, Weiser M, Kaplan Z, Mark M. Behavioral and intellectual markers for schizophrenia in apparently healthy male adolescents. Am J Psychiatry. 1999; 156(9):1328-35. 78. Gunnell D, Harrison G, Rasmussen F, Fouskakis D, Tynelius P. Associations between premorbid intellectual performance, early-life exposures and early-onset schizophrenia. Cohort study. Br J Psychiatry. 2002; 181:298-305. 79. Reichenberg A, Weiser M, Rabinowitz J, Caspi A, Schmeidler J, Mark M, Kaplan Z, Davidson M. A population-based cohort study of premorbid intellectual, language, and behavioral functioning in patients with schizophrenia, schizoaffective disorder,and nonpsychotic bipolar disorder. Am J Psychiatry. 2002; 159(12):2027-35. 80. Reichenberg A, Weiser M, Rapp MA, Rabinowitz J, Caspi A, Schmeidler J, Knobler HY, Lubin G, Nahon D, Harvey PD, Davidson M. Elaboration on premorbid intellectual performance in schizophrenia: premorbid intellectual decline and risk for schizophrenia. Arch Gen Psychiatry. 2005; 62(12):1297-304. 81. Reif A, Jacob CP, Rujescu D, Herterich S, Lang S, Gutknecht L, Baehne CG, Strobel A, Freitag CM, Giegling I, Romanos M, Hartmann A, Rösler M, Renner TJ, Fallgatter AJ, Retz W, Ehlis A-C, Lesch K-P. Functional Variant of Neuronal NO Synthase Influences Impulsive Behaviors in Humans. Arch Gen Psychiatry, in press. 82. Barnett JH, Scoriels L, Munafò MR. Meta-analysis of the cognitive effects of the catechol-O-methyltransferase gene Val158/108Met polymorphism. Biol Psychiatry. 2008 64(2):137-44. 83. Gottesman II, Gould TD. The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry. 2003. 160(4):636-45. 84. Feil R, Kleppisch T. NO/cGMP-dependent modulation of synaptic transmission. Handb Exp Pharmacol. 2008. 184:529-60. 85. Jensen LJ, Kuhn M, Stark M, Chaffron S, Creevey C, Muller J, Doerks T, Julien P, Roth A, Simonovic M, Bork P, von Mering C. STRING 8--a global view on proteins and their functional interactions in 630 organisms. Nucleic Acids Res. 2009. 37:D412-6. 86. H. Hermjakob, L. Montecchi-Palazzi, C. Lewington, S. Mudali, S. Kerrien, S. Orchard, M. Vingron, B. Roechert, P. Roepstorff, A. Valencia, H. Margalit, J. Armstrong, A. Bairoch, G. Cesareni, D. Sherman, R. Apweiler.IntAct - an open source molecular interaction database. Nucl. Acids. Res. 2004. 32: D452-D455 87. Bader GD, Donaldson I, Wolting C, Ouellette BF, Pawson T, Hogue CW. The BIND-The Biomolecular Interaction Network Database. Nucleic Acids Res 2001; 29: 242-245. 88. Lee HJ, Song JY, Kim JW, Jin SY, Hong MS, Park JK, Chung JH, Shibata H, Fukumaki Y. Association study of polymorphisms in synaptic vesicle-associated genes, SYN2 and CPLX2, with schizophrenia. Behav Brain Funct. 2005; 31:1-15. 89. Saviouk V, Moreau MP, Tereshchenko IV, Brzustowicz LM. Association of synapsin 2 with schizophrenia in families of Northern European ancestry. Schizophr Res. 2007; 96:100-11. List of Tables: Table 1: Demographic and clincial data for Irish and German samples. Table 2: Cognitive performance according to NOS1 genotype in both discovery and replication samples. Supplemental Table 1: Principal component analysis of positive and negative symptoms in Irish and German samples. Supplemental Table 2: Observed correlations of verbal and spatial working memroy with Verbal, Performance and full scale IQ. List of Figures: Figure 1: Differences in verbal IQ associated with NOS1 rs6490121 in the Irish and German cases and controls. In addition to a main effect of genotype in both samples, an genotype-diagnosis interaction was observed in the German sample such that the effect of NOS1 was greater in cases than controls. Figure 2: Differences in working memory associated with NOS1 genotype. In addition to a main effect of NOS1 genotype an interaction effect was observed in both groups with NOS1 showing a larger effect in controls in the Irish sample and a larger effect in cases in the German sample.