Lymphatic System The lymphatic system contributes to homeostasis
advertisement

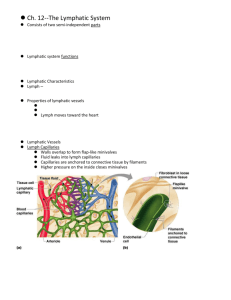
Lymphatic System The lymphatic system contributes to homeostasis by draining interstitial fluid and providing the mechanisms for defense against disease. Lymphatic System Structure and Function Structure of the Lymphatic System The lymphatic system consists of lymph fluid in lymphatic vessels, a number structures and organs containing lymphatic tissue and red bone marrow, where stem cells develop into various types of blood cells. The lymphatic system assists in circulating body fluids and helps defend the body against disease-causing agents. The filtering of the blood plasma through the blood capillary walls forms interstitial fluid. The interstitial fluid passing into the lymphatic vessels is the lymph. The major difference between interstitial fluid and lymph is location. Interstitial fluid is found between cells and lymph is within the lymphatic vessels and lymphatic tissue. Lymphatic tissue is a specialized form of reticular connective tissue. It contains a large number of the agranular WBC, the lymphocytes. There are two types of lymphocytes that participate in immune responses: B cells and T cells. Functions of the Lymphatic System The lymphatic system has 3 functions: 1. Draining excess interstitial fluid. The lymphatic vessels drain excess interstitial fluid from tissue spaces and return it to the blood. 2. Transporting dietary lipids. The lymphatic vessels transports lipids and lipid-soluble vitamins absorbed from the GI tract to the blood. 3. Protects the body against microbes and abnormal cells through immune responses. T cells and B cells aided by macrophages recognize foreign cells, microbes, toxins and cancer cells. The T and B cells respond to these reagents in 2 ways: a. In cell-mediated immune responses, T cells destroys intruding cells by releasing cytotoxic (cell killing) substances to rupture these cells. b. In antibody-mediated immune responses, B cells differentiate into plasma cells that produce antibodies. Antibodies are proteins that combine with and destroy specific foreign substances (antigens). Lymphatic Vessels and Lymph Circulation Lymphatic vessels begin as lymphatic capillaries. These vessels are in the interstitial spaces between the cells and begin as closed end vessels. The lymphatic capillaries unite to form larger lymphatic vessels, the lymphatic veins. The lymphatic veins resemble blood veins in structure but have thinner walls and more valves. At interval along the lymphatic veins there are encapsulated bean-shaped organs, the lymph nodes. The lymph nodes contain the T cells and B cells. 1 Lymphatic Capillaries The lymphatic capillaries have a structure that permits interstitial fluid to flow into these capillaries but not out. The ends of the endothelial cells of the lymphatic capillaries overlap. When pressure is greater in the interstitial fluid than in the lymph, the cells separate slightly and interstitial fluid enters the lymphatic capillaries. When pressure is greater inside the lymphatic capillaries, the cells adhere more closely and the lymph cannot escape back into the interstitial fluid. The pressure is relieved as the lymph moves further along the lymphatic capillary. In the small intestine, specialized lymphatic capillaries called lacteals carry dietary lipids into lymphatic veins and then into the blood. The presence of the lipids causes the lymph draining from the small intestine to appear white; such lymph is referred to as chyle. Elsewhere, lymph is a clear, pale yellow fluid. Lymph Trunks and Ducts As lymphatic veins exit the lymph nodes, they unite to form 5 lymph trunks. Lymph passes from lymph trunks into two lymphatic ducts and then drains into the venous blood. Thoracic Duct (Left Lymphatic Duct) The thoracic duct begins as dilation, the cisterna chyli. The thoracic duct is the main duct for return of lymph to the blood. The thoracic duct receives lymph from the left side of the body and entire body inferior to the ribs. The thoracic duct drains lymph into the left subclavian vein. Right Lymphatic Duct The right lymphatic duct receives lymph from the upper right side of the body and drains lymph into the right subclavian vein. Formation and Flow of Lymph Blood plasma that filters through the capillary walls becomes interstitial fluid but more fluid filters out of the blood capillaries than returns to them by reabsorption. The excess filtered fluid (about 3 liters/day) drains into the lymphatic system and becomes lymph. The small amount of proteins that do filter across the capillary wall cannot return to the blood by diffusion because the concentration gradient for the proteins opposes such movement. The proteins can easily move through the more permeable lymphatic capillaries into the lymph. An important function of the lymphatic vessels is to return the filtered plasma proteins to the blood. Lymphatic vessels contain valves, which ensure the one-way movement of lymph. 2 The sequence of fluid flow is: Blood capillaries (blood) →Interstitial spaces (interstitial fluid) →Lymphatic capillaries (lymph) →Lymphatic veins and trunks→Left and Right Lymphatic ducts→Left and Right Subclavian veins. The same two “pumps” that return venous blood to the heart maintain the flow of lymph. 1. Skeletal muscle pump. The “milking action” of skeletal muscle contractions compresses the lymphatic vessels and forces the lymph toward the subclavian veins. 2. Respiratory pump. Lymph flow is also maintained by pressure changes that occur during inhalation and exhalation. During inhalation lymph flows from the abdominal region, where the pressure is higher, toward the thoracic region where pressure is lower. When the pressure reverses during exhalation, the valves in the lymphatic veins prevent backflow of lymph. Also when the lymphatic veins are distended, smooth muscle in their wall contract to help move lymph from one part of a vessel to the next. Lymphatic Organs and Tissues The lymphatic organs and tissues are classified into two groups based on their functions. Primary Lymphatic Organs The primary lymphatic organs are the red bone marrow and the thymus. These are sites where stem cells divide and become capable of mounting an immune response (become immunocompetent). Stem cells in the red bone marrow give rise to mature, immunocompetent B cells and to pre-T cells. The pre-T cells migrate to the thymus and there become mature immunocompetent T cells. Secondary Lymphatic Organs and Tissues The secondary lymphatic organs and tissues are the places where most immune responses occur. They are the lymph nodes, spleen and lymphatic nodules (follicles). The thymus, lymph nodes and spleen are organs because each is surrounded by a connective tissue capsule. The lymphatic nodules are not organs as they lack a capsule. Lymph Nodes Lymph nodes are located along lymphatic veins. Large groups of lymph nodes are present near the mammary glands and in the axillae and groin. Stroma (Supporting framework of connective tissue) The lymph nodes are covered by a dense connective tissue capsule that extends into the node. The capsular extensions, the trabeculae, divide the node into compartments, provide support and provide a route for blood vessels into the interior of the node. Internal to the capsule there is a supporting framework of reticular fibers and fibroblasts. The capsule, trabeculae, reticular fibers and fibroblasts constitute the stroma of the lymph node. 3 Parenchyma (Functioning part) The parenchyma of the lymph node is divided into a cortex and a medulla. Outer Cortex Within the outer cortex are lymphatic nodules containing B cells. The center of a lymphatic nodule is the germinal center. In the germinal center the B cells proliferate and mature into antibody producing plasma cells or into B memory cells and dendritic cells which present antigen to the B cells. The outer part of the lymphatic nodule that surrounds the germinal center is composed of B cells that migrated from the germinal center. Inner cortex The inner cortex does not contain lymphatic nodules. It consists mainly of T cells that enter the lymph node from other tissues (thymus) and dendritic cells. The T cells proliferate here and then migrate from the lymph node to areas of the body where there is antigenic activity. Medulla The medulla of the lymph node contains B cells, plasma cells and T cells that have migrated out of the cortex. Lymph Flow through the Lymph Node The lymph flows through the lymph node in one direction. The lymph enters through several afferent (to carry toward) lymphatic veins, which penetrate the convex surface of the node. The afferent lymphatic veins contain valves that open toward the center of the lymph node directing the lymph inward. Within the node, the lymph flows through sinuses, a series of irregular channels. The lymph flows from the afferent lymphatic veins into the subcapsular sinus under the capsule. From here the lymph flows through trabecular sinuses, which extend through the cortex parallel to the trabeculae and then into the medullary sinuses, which extend through the medulla. The medullary sinuses drain into 1 or 2 efferent (to carry away) lymphatic veins which lead away from the lymph node. The efferent lymphatic veins contain valves that open away from the center of the lymph node to convey lymph out of the lymph node. The efferent lymphatic veins emerge from one side of the lymph node at a slight depression, the hilum. Blood vessels also enter and leave the lymph node at the hilum. Function of the Lymph Nodes Lymph nodes function as filters. As lymph enters one end of the lymph node, foreign substances are trapped by reticular connective tissue fibers within the sinuses of the lymph node. Then macrophages destroy some foreign substances by phagocytosis and the T and B lymphocytes destroy other foreign substances by immune responses. The filtered lymph then leaves the other end of the lymph node. Spleen The spleen is the largest organ of lymphatic tissue in the body. It is located between the stomach and diaphragm. The spleen has a hilum, through which pass the splenic artery and vein and efferent lymphatic vein. There is no afferent lymphatic vein. 4 A capsule of dense collagenous connective tissue surrounds the spleen and penetrates as trabeculae that extend inward from the capsule. The capsule, trabeculae, reticular fibers and fibroblasts constitute the stroma of the spleen. The parenchyma of the spleen consists of two kinds of tissue, white pulp and red pulp. The white pulp is lymphatic tissue consisting mostly of lymphocytes and macrophages arranged around branches of the splenic artery, the central arteries. The red pulp consists of bloodfilled venous sinuses and cords of splenic tissue, the splenic (Billroth’s) cords. The splenic cords consist of RBCs, macrophages, lymphocytes, plasma cells and granulocytes. Splenic veins drain blood from the red pulp. Functions of the Spleen Blood flowing into the spleen through the splenic artery enters the central arteries of the white pulp. Within the white pulp B cells and T cells carry out immune functions, while the spleen macrophages destroy blood-borne pathogens by phagocytosis. Within the red pulp the spleen carries out 3 functions related to blood cells: 1. removal by macrophages of ruptured; worn out or defective blood cells and platelets; 2. storage of platelets; 3. production of blood cells (hemopoiesis) during fetal life. Lymphatic Nodules (Follicles) The lymphatic nodules are masses of lymphatic tissue that are not surrounded by a capsule. The lymphatic nodules are scattered throughout the lamina propria (connective tissue) of the mucous membranes lining the GI, urinary, respiratory and reproductive tracts. The lymphatic nodules in these areas are referred to as mucosa-associated lymphatic tissue (MALT). Many lymphatic nodules are small and solitary, others occur in multiple large aggregations as the tonsils in the pharynx, aggregates in the ileum of the small intestine (Peyer’s patches) and in the appendix. 5