Asthma, Wheezing, COPD
advertisement

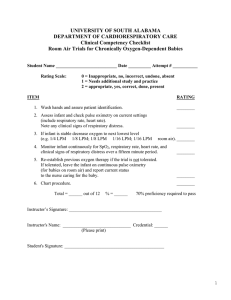
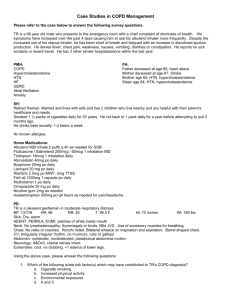
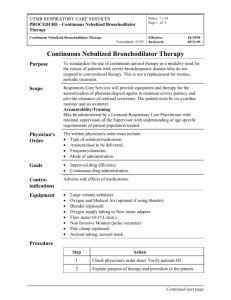
Asthma, Wheezing, COPD Asthma, also referred to as reactive airway disease, and Chronic Obstructive Pulmonary Disease, are conditions of obstructed outward airflow. These patients require substantial expiratory time in their ventilatory cycle. If these patients require BVM or intubation with assisted breathing, it is crucial to give sufficient time for the expiratory phase. They also require small tidal volumes, delivered slowly. Neglecting this technique will result in a patient that is tight and “can’t be bagged.” Indications All patient being treated for known or presumed asthma, wheezing or COPD. Guidelines 1. Airway Protocol. 2. Supplemental oxygen by the method yielding the highest usable 02 delivery tolerated by the patient. 3. Cardiac Monitoring Protocol if patient: Is in moderate to severe respiratory distress. Has prior cardiac history. Is >50 years old. Patients >35 years old receiving epinephrine. 4. ETCO2 Mild Distress 1. Albuterol inhaler, 3 breaths; Note: EMT-I may assist with patient’s own inhaler/nebulizer. 2. Nebulized albuterol, 2.5 mg at 6-8 LPM. Moderate Distress: Nebulized albuterol, 5 mg at 6-8 LPM, may repeat once. Severe Distress: 1. Nebulized albuterol, 5 mg at 6-8 LPM. Note: Continuous administration. 2. Epi 1:1,000: 0.3-0.5mg IM. Note: May repeat every 15 minutes x3. Physician contact required for age >55. 3. CPAP with inline nebulizer initially at 15 LPM (23 minutes; 5 cmH2O PEEP), gradually increasing to 20 LPM (16 minutes; 8 cmH2O PEEP) and finally to 25 LPM (14 minutes; 10 cmH2O PEEP) as necessary. Note: You will need two oxygen sources. 4. MgS04: 1 gm in 100 ml of NS over 10 minutes. Do not use if SBP < 100 or HR < 60/min. Pediatric dose: 25 mg/kg over 10 minutes to maximum of 1 gm. Use MgS04 1 gm/100 ml NS. NOTE: Not to be used in peds < 20 kg. 5. Pediatric: Epi 1:1000: 0.01 mg/kg IM; maximum 0.3 mg/dose. Note: May repeat every 15 minutes x3. Nebulized albuterol, 5 mg at 6-8 LPM, blow by into face, PRN, in transport. Note Epinephrine is not indicated in the patient with COPD. Oxygen administration is indicated for all symptomatic, hypoxemic patients. Those with severe COPD and CO2 retention may be very sensitive to 02; high concentrations may cause further C02 retention. Nevertheless, if these patients are having severe respiratory distress, they should be treated with 02 and monitored carefully for changes in mental status. As they improve, the 0 2 should be titrated down to the lowest comfortable level. Assist ventilations if respiratory distress does not improve and level of consciousness deteriorates. If a COPD patient is being treated for hypoxemia, carefully titrate oxygen to improve the patient¹s clinical status. If available, apply capnography and monitor C0 2 level. If it begins to increase, consider decreasing oxygen concentration. If ventilatory drive is suppressed and the need for oxygen persists, then augment with BVM or other measures as required. Utilize CPAP with inline nebulizer for acute/exacerbated obstructive pulmonary disease (COPD) as well as an acute exacerbation of asthma with respiratory fatigue and other acute pulmonary condition such as pneumonia in which oxygenation is marginal to poor and in whom respiratory effort suggests intubation may soon be required due to patient fatigue. All patients treated for asthma or COPD by AFD must be transported to a receiving facility.