Stage I - Chemotherapy & Biotherapy
advertisement
Teacher’s Guide
STUDENT READ-AHEAD ASSIGNMENT
CHEMOTHERAPY & BIOTHERAPY CLINICAL SKILLS LAB
2/17/2016
Objectives:
Identify information needed for care of the patient with cancer receiving chemotherapy
treatment.
Be familiar with MCH policies addressing chemotherapy handling and administration,
vascular access guidelines, use of central lines, infiltration and extravasation
management, and hazardous material management.
Understand format of and resources for treatment protocols.
Identify appropriate patient education throughout course of treatment.
Identify processes and equipment necessary for safe administration of cytotoxic drugs.
Identify appropriate patient monitoring before, during, and after chemotherapy
treatment.
Review assessment and use of IV access sites.
Identify risks, signs, and management of hypersensitivity reactions.
Identify risks, signs, and management of extravasation.
Identify management of hazardous drug spills.
Identify appropriate use of Personal Protective Equipment (PPE) and disposal of body
fluids.
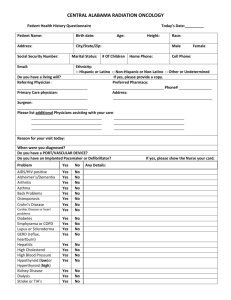
CASE STUDY PART 1
Geri is a 56 year-old female recently diagnosed with Stage IIIA (T3N2M0) Infiltrating Ductal
Carcinoma (see appendix for background information on IDC) of her right breast. Geri found a
lump in her breast while doing a breast self exam. Her physician performed a breast exam and
ordered a digital mammogram, which revealed a 6cm tumor in the right upper quadrant of her
breast. She then saw a surgical oncologist, who performed a core needle biopsy and sentinel
node biopsy, which were determined to be positive for invasive ductal breast cancer with two
cancerous axillary lymph nodes. A bone scan and chest x-ray were then completed to stage her
cancer, as well as genetic and hormone testing of the tumor (which is negative for estrogen and
progesterone receptors).
Geri’s treatment plan is for preoperative chemotherapy, followed by a total right
mastectomy and axillary node dissection. (See appendix for NCCN Practice Guidelines for
Invasive Breast Cancer).
Geri is single, no children, and was menopausal for 3 years at time of diagnosis. She works
as a medical technician for a local medical office. She is somewhat overweight, has seasonal
allergies and an unspecified anxiety disorder, for which she takes 10mg daily of loratadine
(Claritin) and, 40mg daily of fluoxetine (Prozac). She is also taking 1-2 tabs of Percocet Q4H prn
for chronic back pain and senna-s 1-2 tabs BID prn. She has no known drug allergies. Geri
1
smoked approximately one pack per day for 15 years and quit twenty years ago. She has an
alcoholic drink “perhaps one or two per week”.
Her known family history consists of her mother who died of a stroke 10 years ago, her
father is alive and well, her aunt had a bilateral mastectomy 8 years ago without further
treatment or recurrence, and two younger sisters who are alive; one with multiple sclerosis and
the other healthy with two children.
Geri reports that until recently, she has felt well and walked about 5 miles per week. She
reports her diet as “could be better”. Lately she has been feeling more tired and not walking as
much, seems to have more back pain, complains of insomnia, and her anxiety somewhat
increased.
She is admitted to the hospital under your care to start receiving the Sequential AC-T
regimen (see appendix for chemotherapy regimen):
Doxorubicin (Adriamycin) concurrently with cyclophosphamide (Cytoxan) every 21 days for
4 cycles, followed by paclitaxel (Taxol) every 21 days for 4 cycles. She has had a portacath
placed in her right subclavian vein as an outpatient, which is healed and she reports has been
previously accessed by the outpatient nurse with a 1 inch needle with no problems.
Lab results on day of admission (Reference range):
WBC 6.0 (4.8-10.8 x 10³)
Lymphocytes 20% (20.5-51.1%)
Hgb 12.0 (11.7-16.4 g/dL)
Hct 36 (35-47%)
Platelets 330 (140-400 x 10³)
Sodium 140 (136-144 meq/L)
Potassium 3.9 (3.6-5.1 meq/L)
BUN 18 (8-20 mg/dL)
Creatinine 0.7 (0.4-1.0 mg/dL)
Glucose 108 (74-118 mg/dL)
Alkaline Phosphatase 60 (32-91 U/L)
Baseline cancer antigen levels, or serum tumor markers (may be obtained initially and
checked periodically to assess response to treatment. They are not specific indicators of cancer
and are elevated in <50% of patients with localized breast cancer):
CEA (Carcinoembryonic antigen); 2 (<5 ng/ml)
CA 15-3; 20 (<22 U/ml)
CA27-29; 32 (<38 U/ml)
HER-2/neu (Human epidermal growth factor receptor 2): negative
Diagnostic Imaging:
Mammogram showing 6cm tumor in right upper quadrant of right breast.
Chest x-ray negative.
2
Bone scan showing no metastases.
Vital signs on admission:
Height 5’6”
Weight 180 lbs.
Temp 98.9
Pulse 88
Resp 20
BP 138/84
O2 sat 98% room air
Admitting Orders:
VS Q shift
Regular diet; encourage fluids
Up ad lib
I & O Q shift
CBC, CMET daily
Lorazepam, 0.5-2mg PO or IV Q4H prn anxiety or insomnia
Ondansetron 4-8mg PO or IV prn nausea/vomiting
Percocet, 1-2 tabs PO Q4H prn
Loratadine 10mg PO daily
Fluoxetine 40mg PO daily
Senna-s, 1-2 tabs PO BID prn
NS 100 ml/hour, to run before and after chemotherapy
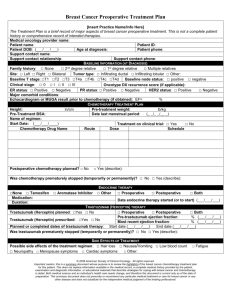
Chemotherapy, start tomorrow:
Premedication:
1. Aprepitant 125 mg PO Day 1; then 80mg PO or IV days 2 & 3
2. Dexamethasone 12mg IV in 50 mL NS over 10 minutes on day 1, then 8mg PO daily on
days 2-4
3. Palonsetron 0.25 mg IV Push on day 1
4. Doxorubicin 60mg/m² IV push, 135mg.
5. Cyclophosphamide 600mg/m² IV over 30 minutes, 1170mg in 100 mL NS.
Geri’s BSA is 1.95
Doxorubicin dose is incorrect. Correct dose is 117mg; doctor needs to be called since dose
difference is greater than 10 percent (per MCH policy).
Cyclophosphamide dose is correct.
3
CASE STUDY DISCUSSION:
1. Does Geri have appropriate lab work completed before starting chemotherapy? What labs
are critical to know before administering her ordered chemotherapy?
No; we’re missing her LFTs. After chemo will need WBC with differential, H&H, platelet
count, BUN/creatinine, sodium, potassium, magnesium. Liver function for doxorubicin;
renal function and hydration status for cyclophosphamide.
2. What else do you need to review from Geri’s medical information?
a. H&P, progress notes.
b. Current height & weight (not from her last office visit).
c. General performance status, nutritional status.
d. Symptoms and effectiveness of management strategies
e. Orders for chemotherapy, premeds, and prn medications for management of
likely symptoms).
3. What other tests should Geri have completed?
Doxorubicin; should have echocardiogram & ECG before administering doxorubicin.
4. What do you consider as possible issues/nursing diagnoses for Geri?
Altered Body image r/t surgery and alopecia; refer to American Cancer Society’s Look Good,
Feel Better program & local support groups.
Fear of intimacy; change in family & social relationships.
Possible weight gain from treatment.
Sexual dysfunction relative to altered body image.
Assess coping skills, support systems.
Knowledge deficit of medications and side effects.
Risk for infection, fatigue, pain, nausea/vomiting, altered bowel patterns, lymphedema,
anxiety, depression, anorexia, mucositis, cardiomyopathy, peripheral neuropathy; teach
preventive measures & signs to report.}
Maintenance of health & preventive screening (continuing to perform monthly BSE, both
breasts, yearly mammograms & clinical breast exams).
Survivorship: monitoring of care r/t long term effects of chemotherapy drugs.
*Refer to ONS PEP cards for evidence-based interventions.
5. Where do you look to find drug administration information, side effect profile, and to
determine if ordered dose is within expected limits?
ONS Chemotherapy drug books, protocol books in chemo cart. ONS, NCCN, National
Cancer Institute web sites.
6. Are the chemotherapy orders correct and complete? What is her BSA? Are the ordered
drug doses correct?
BSA = 1.95 (Mostellar formula)
Doxorubicin 60mg/m² IV push, correct dose is 117 mg per BSA 1.95.
4
Cyclophosphamide 600mg/m² IV over 30 minutes, 1170 mg per BSA.
7. What do you need to do prior to administering this cycle of chemotherapy?
Calculate BSA, calculate dosages, verify with orders, and verify chemotherapy
labels; all above with 2nd chemo-competent RN. Both RNs should independently perform
all calculations.
Think about timing and revise with pharmacy as necessary: don’t have
chemotherapy start within an hour of shift change. Have as much pre-work done as
possible if chemo needs to be started on next shift. Notify the Resource Nurse that a
chemotherapy provider nurse will need to be assigned to that patient.
Don’t start giving premeds until everything is calculated and verified, you have
all lab results available, and the first dose of chemotherapy is on the floor.
Have medications available on the unit for hypersensitivity reaction if
appropriate based on drugs being given.
8. What does your patient education consist of for Geri, in terms of general chemotherapy
administration?
a. Does Geri understand her cancer, the treatment, and does she agree with the
plan of care (informed consent)?
b. What are her goals for treatment?
c. What else does she need to know?
d. How much does she want to know?
e. Who else does she want you to give information to?
f. Does she understand potential immediate and delayed side effects, and when to
call nurse/MD?
g. What are the most serious side effects/toxicities that she needs to know
symptoms to report? (time of expected nadir, s/s infection, how to take
temperature; does she have a thermometer?
h. Provide printed information and assure her you and other nurses will review this
information with her and answer any questions.
i. Provide other resources if she’s interested (see appendix)
9. What do you need to know and what will your patient education consist of specifically for
doxorubicin and cyclophosphamide?
a. Doxorubicin:
i. Severe vesicant; extravasation precautions, MCH policy on administering
vesicants {IVP only through peripheral IV, side arm of free flowing IV;
otherwise need central line}
ii. Teaching/Side effects for this drug:
1. Myelosuppression
2. Nausea/vomiting/diarrhea.
3. Colors urine red.
4. Mucositis.
5. Alopecia.
5
6. Cardiotoxicity (pre-treatment tests: echo, EKG)
7. Chronic & cumulative cardiomyopathy expected when total
lifetime dose > 550 mg/m² (lifetime dose drops to 450mg/m² for
concomitant cyclophosphamide treatment or prior chest
irradiation)
iii. Symptoms of reaction to any drug, when to call for help.
b. Cyclophosphamide:
i. Teaching/Side effects for this drug:
1. Adequate hydration; 2-3 liters per day.
2. Side effects of this drug:
3. Myelosuppression
4. Nausea/vomiting/diarrhea.
5. Anorexia.
6. Alopecia.
7. Mucositis.
8. Hemorrhagic cystitis: irritation of bladder. S/s are blood in urine,
pain or burning with urination.
9. Empty bladder frequently to prevent hemorrhagic cystitis.
10. Mesna may be considered as an addition to cyclophosphamide to
prevent hemorrhagic cystitis.
10. After 4 cycles of AC, what is her cumulative dose of doxorubicin? Why do you care?
468 mg; as patient approaches maximum lifetime dose, chance of Cardiotoxicity increases.
11. What do you need to document before, during, after administration? What does your RN
handoff consist of?
Review text pages ----12. Demonstrate correct use of PPE.
Have a set of PPE and demonstrate correct wearing and removal. May show video on
2009 ONS CD rom.
Review text pages ----13. Demonstrate correct setup of closed system tubing and its purpose.
Have a pump, spiros tubing, and connectors and demonstrate correct setup. (see
appendix for pictures and explanation of correct setup).
14. Explain chemo precautions, signage, and what to teach staff, patient, and visitors.
Review neutropenic policy and text pages ----18. Explain disposal of waste, contaminated linen, body fluids.
Review text pages ----19. Define a hazardous spill; what do you do? What should you document?
6
Review text pages ----Show video on 2009 ONS training class CDrom.
7
CASE STUDY PART 2: Administration of Chemotherapy with Central Lines and Monitoring and
management of Extravasation.
Geri has completed her 4th cycle of doxorubicin and cyclophosphamide three weeks ago,
and returns today for her first dose of paclitaxel.
Her EKG on admission shows Normal Sinus Rhythm; echocardiogram shows and EF of
60%.
Lab results on day of admission (Reference range):
WBC 4.0 (4.8-10.8 x 10³)
Lymphocytes 20% (20.5-51.1%)
Neutrophils 60% (55-70%)
Bands 3%
Hgb 10.8 (11.7-16.4 g/dL)
Hct 32 (35-47%)
Platelets 240 (140-400 x 10³)
Sodium 138 (136-144 meq/L)
Potassium 3.6 (3.6-5.1 meq/L)
BUN 10 (8-20 mg/dL)
Creatinine 0.5 (0.4-1.0 mg/dL)
Glucose 120 (74-118 mg/dL)
Alkaline Phosphatase 70 (32-91 U/L)
Admitting Orders:
1. Diphenhydramine 50mg IV in 50mL NS over 10 minutes, 60 minutes before paclitaxel.
2. Cimetidine 30mg IV in 50mL NS over 10 minutes, 30 minutes before paclitaxel.
3. Dexamethasone 10mg IV in 50mL NS over 10 minutes, 30 minutes before paclitaxel.
4. Paclitaxel 80mg/m² over 3 hours; 156mg in 500 mL NS.
5. In case of hypersensitivity reaction:
25mg Benadryl IV push.
100mg solucortef IV push.
If patient is hemodynamically unstable (hyptotensive, hypoxic); give 0.3mg epinephrine
SC and Call MD.
When symptoms subside, restart paclitaxel infusion.
You obtain a 20g 1” gripper needle and access Geri’s port. You got a few drops of blood when
pulling back the syringe, then nothing. You try to flush the port; it appears to flush fine with no
difficulty or pain. You try flushing by pushing saline & pulling back in short spurts, having Geri
cough, and reposition her shoulder, and are unable to obtain a blood return.
1.
What do you do next?
Per MCH policy, you need to obtain a blood return before giving chemotherapy. It is not
enough to verify placement based on diagnostic imaging. The most likely cause of lack of
8
blood return is the presence of a fibrin sheath; instilling chemo could cause vein irritation or
damage as the chemo adheres to the fibrin sheath and attaches to the vessel wall. You need
to call the doctor to get orders for Cath-Flo. Cath-Flo should be instilled for 60-90 minutes and
then retry for blood return, and a second dose may be used.
2.
What do you need to know and what will your patient education consist of specifically
for paclitaxel?
Paclitaxel:
Administration:
Is an irritant and possible vesicant
Use 0.22 micron filter (filter in our closed system tubing is 15 microns; you need
additional filter)
Premedicate to decrease hypersensitivity reactions (dexamethasone,
diphenhydramine, cimetidine)
Have Hypersensitivity treatment medications on unit before starting paclitaxel.
Stay with patient for first 15 minutes of treatment; monitor VS.
S/s hypersensensitivity reaction: urticaria, wheezing, chest pain, dyspnea,
hypotension, angioedema, tachycardia)
Treatment for hypersensitivity reaction (you need orders for this. For drugs with
increased likelihood of reaction, such as paclitaxel, orders and medications should be
obtained before administering drug):
ii. Stop infusion
iii. STAY WITH PATIENT
iv. CALL MD
v. Give 25mg Benadryl IV
vi. Give 100mg solucortef IV
vii. If patient is hemodynamically unstable (hyptotensive, hypoxic, give 0.3mg
epinephrine SC.
viii. Call MD
ix. When symptoms subside, restart paclitaxel infusion
Teaching/Side effects for this drug:
1. Myelosuppression; especially leukopenia.
2. Nausea/vomiting/diarrhea.
3. Mucositis.
4. Alopecia.
5. Peripheral Neuropathy (60% incidence of symptoms); may
manifest as:
6. Autonomic Nervous System:
a. BP: Orthostatic hypotension
b. Intestinal motility (constipation or ileus)
7. Sensory Nervous System:
a. Large nerve fiber vibration and proprioception
(altered sense of position, movement, and force)
9
8. Motor Nervous System:
a. Reflexes
b. Strength
c. Numbness & tingling, usually a stocking-glove
distribution (starts in tips of fingers & toes and moves
upwards)
9. Alopecia
You stay with Geri for the first 20 minutes of the infusion, taking vital signs before you start the
infusion and during the time you’re there. After 15 minutes, Geri continues talking but you
think she is started to get dyspneic and slightly wheezy. She is starting to scratch her neck.
What do you do?
See above treatment for hypersensitivity protocol; stop drug; maintain IV and infuse NS.
Stay with the patient; call for help and have someone bring the medications for hypersensitivity
and give them. Monitor VS; call MD is symptoms worsen or if pt becomes hypotensive and/or
hypoxic.
You’ve successfully treated Geri for a hypersensitivity reaction, her symptoms have subsides,
and you have restarted her infusion. You stay with her for 20 minutes and all is going well, so
you leave to answer another patient’s call light. 45 minutes later Geri calls you into the room
and asks you to look at her port site. What are you assessing? What are the signs and
symptoms of a central line extravasation?
Surrounding the site or the chest wall: Swelling (most common), stinging, burning, or
pain at injection site (may not always be present), IV flow rate that slows or stops, leaking
around catheter or implanted port needle, lack of blood return (not always a sign of
extravasation; extravasation may occur with the presence of a blood return), erythema,
inflammation, or blanching at the injection site; induration, vesicle formation, ulceration.
How would you manage an extravasation?
Stop all IV meds and fluids.
Disconnect IV tubing from catheter; leave catheter in place.
If portacath, assess site for proper needle placement.
Attempt to aspirate residual drug from IV device by using a small (1-3 cc) syringe, then remove
the IV catheter.
Apply cold or hot compresses per MCH policy (ice pack 15-20 minutes at least four times daily
for the first 24hrs for paclitaxel).
Call pharmacy for possible antidote.
Notify MD (for assessment & possible radiographic flow study, and antidote order if available).
Document!
Complete variance report.
Photograph the site.
Pt should rest & elevate site for 48 hours and then resume normal activity.
No medications should be given distally to an extravasation injury.
Patient teaching; provide written instructions on care.
10
APPENDIX: Additional information for Case Study
Invasive ductal carcinoma: from www.breastcancer.org
Invasive ductal carcinoma (IDC), sometimes called infiltrating ductal carcinoma, is the most
common type of breast cancer. About 80% of all breast cancers are invasive ductal carcinomas.
Invasive means that the cancer has “invaded” or spread to the surrounding breast tissues. Ductal
means that the cancer began in the milk ducts, which are the “pipes” that carry milk from the
milk-producing lobules to the nipple. Carcinoma refers to any cancer that begins in the skin or
other tissues that cover internal organs — such as breast tissue. All together, “invasive ductal
carcinoma” refers to cancer that has broken through the wall of the milk duct and begun to
invade the tissues of the breast. Over time, invasive ductal carcinoma can spread to the lymph
nodes and possibly to other areas of the body.
According to the American Cancer Society, more than 180,000 women in the United States are
diagnosed with invasive breast cancer each year. Most of them are diagnosed with invasive
ductal carcinoma.
Although invasive ductal carcinoma can affect women at any age, it is more common as women
grow older. According to the American Cancer Society, about two-thirds of women are 55 or
older when they are diagnosed with an invasive breast cancer. Invasive ductal carcinoma also
affects men.
At first, invasive ductal carcinoma may not cause any symptoms. Often, an abnormal area turns
up on a screening mammogram (x-ray of the breast), which leads to further testing.
In some cases, the first sign of invasive ductal carcinoma is a new lump or mass in the breast
discovered by palpation. According to the American Cancer Society, any of the following
unusual changes in the breast can be a first sign of breast cancer, including invasive ductal
carcinoma:
swelling of all or part of the breast
skin irritation or dimpling
breast pain
nipple pain or the nipple turning inward
redness, scaliness, or thickening of the nipple or breast skin
a nipple discharge other than breast milk
a lump in the underarm area
Diagnosing invasive ductal carcinoma usually involves a combination of procedures, including a
physical examination and imaging tests.
11
Physical examination of the breasts: A small lump may be felt in the breast or nearby
lymph nodes, including those under the armpit and above the collarbone.
Mammography: Invasive ductal carcinoma is usually found by mammography, a test that
obtains x-ray images of the breast. Mammograms are used to screen apparently healthy
women for early signs of breast cancer. One key feature of an invasive breast cancer is
spiculated margins, which means that on the mammography film, the doctor sees an
abnormality with finger-like projections coming out of it. These projections show the
“invasion” of the cancer into other tissues.
If a screening mammogram highlights an area of concern, additional mammograms often
will be done to gather more information about that area. Mammography will be
performed on both breasts.
Ultrasound bounces sound waves off of the breast to obtain additional images of the
tissue. Ultrasound is sometimes used in addition to mammography.
Breast MRI: MRI, or magnetic resonance imaging, uses magnetic fields, radio waves, and
a computer to obtain images of tissues inside the body. In certain cases breast MRI may
be used to gather more information about a suspicious area within the breast.
Biopsy: A suspicious mammogram finding or other imaging test result will require a
biopsy. A biopsy involves taking out some or all of the abnormal-looking tissue for
examination by a pathologist (a doctor trained to diagnose cancer from biopsy samples)
under a microscope.
When possible, your doctor will usually use one of the quicker, less invasive approaches
to biopsy:
o Fine needle aspiration biopsy involves inserting a very small, hollow needle into
the breast. A sample of cells is removed and examined under the microscope. This
method leaves no scars.
o Core needle biopsy inserts a larger needle into the breast to remove several
cylinder-shaped samples of tissue from the area that looks suspicious. In order to
get the core needle through the skin, the surgeon must make a tiny incision. This
leaves a very tiny scar that is barely visible after a few weeks.
If the lump cannot be felt, ultrasound or mammogram is used to guide the needle to the
right location (this is a stereotactic needle biopsy or ultrasound-guided biopsy).
If a needle biopsy is not able to remove cells or tissue, or it does not give definite results
(inconclusive), a more involved biopsy may be necessary. These biopsies are more like
regular surgery than needle biopsies, and may also involve the use of ultrasound or
mammography:
o Incisional biopsy removes a small piece of tissue for examination.
o Excisional biopsy attempts to remove the entire suspicious lump of tissue from
the breast.
These surgical biopsies are done only to make the diagnosis. If invasive ductal carcinoma is
diagnosed, more surgery is needed to ensure all of the cancer is removed along with “clear
12
margins,” which means that a border of healthy tissue around the cancer is also removed.
Usually this means having lumpectomy, or in some cases, mastectomy.
Staging is the process used to figure out how far invasive ductal carcinoma may have spread
from its original location. The stage of the cancer is based on three pieces of information:
the size of the tumor
whether the cancer has spread to any lymph nodes, and if so, how many
whether the cancer has spread to other parts of the body
Invasive ductal carcinoma is described on a scale from stage I (the earliest stage) through stage
IV (the most advanced stage). Each type of cancer has its own staging system; solid tumors are
defined using the TNM system and then grouped into stages; the differentiation between T1 and
T2, etc. are different for each type of cancer.
Breast cancer stage is based on the size of the tumor, whether the cancer is invasive or noninvasive, whether lymph nodes are involved, and whether the cancer has spread beyond the
breast.
The purpose of the staging system is to help organize the different factors and some of the
personality features of the cancer into categories, in order to:
best understand the prognosis (the most likely outcome of the disease)
guide treatment decisions (in tandem with the pathology report)
provide a common way to describe the extent of breast cancer.
Stage 0
Stage 0 is used to describe non-invasive breast cancers (“carcinoma in situ”). In stage 0, there is
no evidence of cancer cells or non-cancerous abnormal cells breaking out of the part of the breast
in which they started, or of getting through to or invading neighboring normal tissue.
Stage I
Stage I describes invasive breast cancer (cancer cells are breaking through to or invading
neighboring normal tissue) in which:
the tumor measures up to 2 centimeters, AND
no lymph nodes are involved
Stage II
Stage II is divided into subcategories known as IIA and IIB.
Stage IIA describes invasive breast cancer in which:
13
no tumor can be found in the breast, but cancer cells are found in the axillary lymph
nodes (the lymph nodes under the arm), OR
the tumor measures 2 centimeters or less and has spread to the axillary lymph nodes, OR
the tumor is larger than 2 centimeters but not larger than 5 centimeters and has not spread
to the axillary lymph nodes
Stage IIB describes invasive breast cancer in which:
the tumor is larger than 2 but no larger than 5 centimeters and has spread to the axillary
lymph nodes, OR
the tumor is larger than 5 centimeters but has not spread to the axillary lymph nodes
Stage III
Stage III is divided into subcategories known as IIIA, IIIB, and IIIC.
Stage IIIA describes invasive breast cancer in which either:
no tumor is found in the breast. Cancer is found in axillary lymph nodes that are clumped
together or sticking to other structures, or cancer may have spread to lymph nodes near
the breastbone, OR
the tumor is 5 centimeters or smaller and has spread to axillary lymph nodes that are
clumped together or sticking to other structures, OR
the tumor is larger than 5 centimeters and has spread to axillary lymph nodes that are
clumped together or sticking to other structures
Stage IIIB describes invasive breast cancer in which:
the tumor may be any size and has spread to the chest wall and/or skin of the breast AND
may have spread to axillary lymph nodes that are clumped together or sticking to other
structures, or cancer may have spread to lymph nodes near the breastbone
Inflammatory breast cancer is considered at least stage IIIB.
14
Stage IIIC describes invasive breast cancer in which:
there may be no sign of cancer in the breast or, if there is a tumor, it may be any size and
may have spread to the chest wall and/or the skin of the breast, AND
the cancer has spread to lymph nodes above or below the collarbone, AND
the cancer may have spread to axillary lymph nodes or to lymph nodes near the
breastbone
Stage IV
Stage IV describes invasive breast cancer in which the cancer has metastasized to other organs of
the body -- usually the bone, lungs, liver, or brain
Additional staging information
You may also hear terms such as "early" or "earlier" stage, "later," or "advanced" stage breast
cancer. Although these terms are not medically precise (they may be used differently by different
doctors), here is a general idea of how they apply to the official staging system:
Early stage
Stage 0
Stage I
Stage II
Some stage III
Later or advanced stage
Other stage III
Stage IV
The most commonly used staging system is the TNM system.
The T (size) category describes the original (primary) tumor:
TX means the tumor can't be measured or found.
T0 means there isn't any evidence of the primary tumor.
Tis means the cancer is "in situ" (the tumor has not started growing into the breast tissue).
The numbers T1-T4 describe the size and/or how much the cancer has grown into the
breast tissue. The higher the T number, the larger the tumor and/or the more it may have
grown into the breast tissue.
The N (node involvement) category describes whether or not the cancer has reached nearby
lymph nodes:
NX means the nearby lymph nodes can't be measured or found.
15
N0 means nearby lymph nodes do not contain cancer.
The numbers N1-N3 describe the size, location, and/or the number of lymph nodes
involved. The higher the N number, the more the lymph nodes are involved.
The M (metastasis) category tells whether there are distant metastases (whether the cancer has
spread to other parts of body):
MX means metastasis can't be measured or found.
M0 means there are no distant metastases.
M1 means that distant metastases were found.
Once the pathologist knows your T, N, and M characteristics, they are combined in a process
called stage grouping, and an overall stage is assigned.
For example, a T3N2M0 breast cancer would mean that the primary breast tumor:
is greater than 5 centimeters across (T3)
metastasis to ipsilateral axillary lymph nodes or nodes fixed to one another or to other
structures (N2)
has not spread to distant parts of the body (M0)
This cancer would be grouped as a stage IIIA cancer.
At this point, your doctor may look for clues as to whether invasive ductal carcinoma cells could
have spread to other areas of the body. Your doctor may order certain blood tests, a test of your
liver function, and a test for a substance in the blood called alkaline phosphatase, or ALP. ALP
may be higher than usual in people who have cancer in the liver or the bones.
Based on these test results, a physical examination, and any symptoms you report, your doctor
will decide whether or not additional tests are needed to check other areas of the body. In most
cases, you can expect to have an x-ray of the chest to check the lungs. Beyond that, the need for
additional testing is determined on a case-by-case basis. Tests that could be done include:
Bone scan: This takes pictures of the bones after you are given a small injection of
radioactive substance.
CT (computerized tomography) scan, ultrasound, or MRI are used to create images of the
abdomen and pelvis (the stomach area) or other areas of the body.
PET/CT scan: PET (positron emission tomography)/CT scan is a newer technology used
to obtain images of the body’s cells as they work. This test is used to look for metastases.
A substance made up of sugar and a small amount of radioactive material is injected. The
scan then “highlights” any cancer cells throughout the body as they absorb the
radioactive substance (cancer cells metabolize glucose quicker than other cells).
The most common sites of spread for IDC are the bones, liver, lung, and/or brain.
Additional tests will be done on the tumor tissue to gather more information about how the
cancer is likely to behave and what treatments will be most effective. Examples include:
16
Grade: A pathologist examines the cancer cells under a microscope and determines how
abnormal they appear and behave when compared with healthy breast cells. The lower
the grade, the more closely the cancer cells resemble normal cells, the more slowly they
grow, and the less likely they are to spread. There are three grades of invasive ductal
carcinoma: low or grade 1; moderate or grade 2; and high or grade 3.
Grade 1 invasive ductal carcinoma cells, which are sometimes called “welldifferentiated,” look and act somewhat like healthy breast cells. Grade 3 cells, also called
“poorly differentiated,” are more abnormal in their behavior and appearance.
Surgical margins: When cancer cells are removed from the breast, the surgeon tries to
take out the whole cancer with an extra area or “margin” of normal tissue around it. This
is to be sure that all of the cancer is removed. The tissue around the very edge of what
was removed is called the margin of resection. It is looked at very carefully to see if it is
clear of cancer cells.
The pathologist also measures the distance between the cancer cells and the outer edge of
the tissue. Margins around a cancer are described in three ways:
o Negative: No cancer cells can be seen at the outer edge. Usually, no more surgery
is needed.
o Positive: Cancer cells come right out to the edge of the tissue. More surgery may
be needed.
o Close: Cancer cells are close to the edge of the tissue, but not right at the edge.
More surgery may be needed.
What are called “negative” (or “clean”) margins can be different from hospital to
hospital. In some places, doctors want at least 2 millimeters (mm) of normal tissue
beyond the edge of the cancer. In other places, doctors may define a “clean margin” as
less than 2 mm or more than 2 mm of healthy tissue.
Hormone receptor assay: This tissue test determines whether or not the breast cancer has
receptors for the hormones estrogen and progesterone. A positive result means that
estrogen or progesterone (or both) has the ability to fuel the cancer cells’ growth. If the
cancer is hormone-receptor-positive, hormonal therapies that block the effects of estrogen
or lower estrogen levels in the body will be recommended. Examples include tamoxifen
and aromatase inhibitors. For premenopausal women, other options may be
recommended, such as using medications to shut down your ovaries temporarily, or even
surgically removing them. The ovaries are the body’s main source of estrogen before
menopause.
HER2-receptor status: Another test is done to find out whether the breast cancer cells
make too much of a protein called HER2 (human epidermal growth factor receptor 2). If
they do, then they also have too many HER2 receptors at the cell surface. With too many
receptors, breast cancer cells pick up too many growth signals and start growing too
much and too fast. Traztuzumab (Herceptin) is a monoclonal antibody that slows down or
stops the growth of the cancer cells by blocking the receptors so they don't pick up as
many growth signals. About 1 out of 4 breast cancers are HER2-positive, which means
they can be treated with Herceptin.
17
HER2-positive cancers also can be treated with Tykerb (chemical name: lapatinib), a
medication that interferes with the activity of HER2 from inside the cell. Tykerb limits
the amount of energy the breast cancer cells have to grow and multiply. These tests are
done on the tissue that is removed during biopsy, or, in the case of surgical margins, after
the surgery to remove the cancer.
APPENDIX; ADDITIONAL INFORMATION FOR CASE STUDY
Resources for Clinical and Patient education:
References available in Chemotherapy cart on MedSurg:
Chemotherapy and Biotherapy Guidelines and Recommendations for Practice, 3rd edition 2009, ONS.
Clinical Guide to Antineoplastic Therapy; A Chemotherapy Handbook 2nd edition 2007, ONS.
Regimen/Protocol books:
Guide to Selected Cancer Chemotherapy Regimens and Associated Adverse Events, Amgen.
The Elselvier Guide to Oncology Drugs and Regimens
Clinical Guide to Antineoplastic Therapy; A Chemotherapy Handbook 2nd edition 2007, ONS, Chapter 6,
Chemotherapy Regimens (pp. 365-425).
Chemotherapy drug information, from Micromedex
Available in the Med/surg Education Closet and also on the websites:
“Chemotherapy and You”, National Cancer Institute
“Radiation Therapy and You”, National Cancer Institute
“Neutrophil: Your One-in-a-Million Bodyguard Guides You Through Neutropenia”, Oncology
Nursing Society Foundation.
“Eating Hints for Cancer Patients Before, During & After Treatment”, National Cancer Institute.
“The American Cancer Society Guidelines on Nutrition and Physical Activity for Cancer
Prevention”, American Cancer Society.
“Coping with Nausea and Vomiting from Chemotherapy”, Cancer Care.
“Finding New Ways to Cope with Fatigue”, Cancer Care.
Web sites:
American Cancer Society, www.cancer.gov
Cancer Care (free services from oncology social workers; 1-800-813-4673). www.cancercare.org
National Cancer Institute, www.cancer.org
National Comprehensive Cancer Network, www.nccn.org
Oncology Nursing Society, www.ons.org
FDA: www.drugs.com
www.chemocare.com
www.globalrph.com (drugs, calculators for BSA, ANC, renal clearance, corrected calcium,
opioids conversion calculator, more)
www.uptodate.com (from MCH computers) for comprehensive information for clinicians and
patients on diagnoses, treatments, drugs.
18
Mid Coast Hospital Policies:
MCH Vascular Access Guidelines
IV In-Line Filter Use Guidelines
Care and Use of Central Lines
Clearing Occluded Central Lines
Chemotherapy Administration
Chemotherapy Handling
Infiltration and Extravasation of IV Medications
Hazardous Material Management Program
Hazardous Materials Spill Procedure
**Insert NCCN Practice Guidelines for Invasive Breast Cancer (available on www.nccn.org) and
AC-T protocol (Doxorubicin, Cyclophosphamide, Paclitaxel)
19
Patient Drug Handouts
Doxorubicin (from www.chemocare.com)
Brand Names: Adriamycin ®, Rubex ®
Drug Type:
Doxorubicin is an anti-cancer (“antineoplastic” or “cytotoxic”) chemotherapy drug. Doxorubicin
is classified as an “anthracycline antiobiotic.” (For more detail, see “How Doxorubicin Works”
section below).
What Doxorubicin Is Used For:
Cancers treated with Doxorubicin include: bladder, breast, head and neck, leukemia
(some types), liver, lung, lymphomas, mesothelioma, multiple myeloma, neuroblastoma,
ovary, pancreas, prostate, sarcomas, stomach, testis (germ cell), thyroid, uterus.
Note: If a drug has been approved for one use, physicians sometimes elect to use this same drug
for other problems if they believe it might be helpful.
How Doxorubicin Is Given:
Doxorubicin is given through a vein by intravenous injection (IV). The syringe needle is
placed directly into the vein or central line and the drug is given over several minutes.
Doxorubicin can also be given by continuous infusion. Rarely, Doxorubicin is given by
injection into an artery. There is no pill form of Doxorubicin.
Doxorubicin is a vesicant. A vesicant is a chemical that causes extensive tissue damage
and blistering if it escapes from the vein. The nurse or doctor who gives Doxorubicin
must be carefully trained. If you notice redness or swelling at the IV site while you are
receiving Doxorubicin, alert your health care professional immediately.
The amount of Doxorubicin you will receive depends on many factors, including your
height and weight, your general health or other health problems, and the type of cancer
you have. Your doctor will determine your exact dosage and schedule.
Side Effects of Doxorubicin:
Important things to remember about the side effects of Doxorubicin:
You will not get all of the side effects mentioned below.
Side effects are often predictable in terms of their onset, duration, and severity.
Side effects are almost always reversible and will go away after therapy is complete.
Side effects are quite manageable. There are many options to minimize or prevent them.
20
The following side effects are common (occurring in greater than 30%) for patients taking
Doxorubicin:
Early Side Effects: (within one week after treatment begins)
Pain along the site where the medication was given
Nausea or vomiting
Later Side Effects: (within two weeks after treatment begins)
Low blood counts. Your white and red blood cells and platelets may temporarily
decrease. This can put you at increased risk for infection, anemia and/or bleeding.
Nadir: Meaning low point, nadir is the point in time between chemotherapy cycles in which you
experience low blood counts.
Onset: 7 days
Nadir: 10-14 days
Recovery: 21-28 days
Mouth sores
Hair loss on the scalp or elsewhere on the body (called alopecia). Most patients do lose
some or all of their hair during their treatment. But your hair will grow back after
treatment is completed.
The following side effects are less common (occurring in 10-29%) for patients taking
Doxorubicin:
Early: (within one week after treatment begins)
Eyes watering
Urine may appear red, red-brown, orange or pink from the color of the medication for
one to two days after you receive a dose.
Later: (within two weeks after treatment begins)
Darkening of the nail beds.
Darkening of the skin where previous radiation treatment has been given.
Problems with fertility – ability to bear children. (occurs in about 10% of both men and
women – this should be discussed with your doctor prior to therapy).
A serious but uncommon side effect of Doxorubicin can be interference with the pumping action
of the heart. You can receive only up to a certain amount of Doxorubicin during your lifetime.
This “lifetime maximum dose” may be lower if you have heart disease risk factors such as
radiation to the chest, advancing age, and use of other heart-toxic drugs. Your doctor will check
your heart function before you may take any Doxorubicin and will monitor your heart closely
21
during your treatment. Dose-related heart problems can occur as late as 7 or 8 years after
treatments have ended.
Delayed Effects of Doxorubicin:
There is a slight risk of developing a blood cancer such as leukemia years after taking
Doxorubicin. Talk to your doctor about this risk.
This list includes common and less common and important side effects for those taking
Doxorubicin. Side effects that are very rare – occurring in less than 10 percent of patients – are
not listed here. But you should always inform your health care provider if you experience any
unusual symptoms.
When To Contact Your Doctor or Health Care Provider:
Contact your health care provider immediately, day or night, if you should experience any of the
following symptoms:
Fever of 100.5º F (38º C), chills (possible signs of infection)
Blistering at the IV site
Shortness of breath, wheezing, difficulty breathing, closing up of the throat, swelling of
facial features, hives (possible allergic reaction).
The following symptoms require medical attention, but are not emergency situations. Contact
your health care provider within 24 hours of noticing any of the following:
Mouth sores (painful redness, swelling or ulcers)
Nausea (interferes with ability to eat and unrelieved with prescribed medication)
Vomiting (vomiting more than 4-5 times in a 24 hour period)
Diarrhea (4-6 episodes in a 24-hour period)
Fast or irregular heart beats
Unusual bleeding or bruising
Black or tarry stools, or blood in your stools or urine
Extreme fatigue (unable to carry on self-care activities)
Swelling of the feet or ankles
Doxorubicin Precautions:
Before starting Doxorubicin treatment, make sure you tell your doctor about any other
medications you are taking (including over-the-counter, vitamins, or herbal remedies).
Do not take aspirin or products containing aspirin unless your doctor permits this.
Do not receive any kind of vaccination without your doctor’s approval while taking
Doxorubicin.
For both men and women: Use contraceptives, and do not conceive a child (get pregnant)
while taking Doxorubicin. Barrier methods of contraception, such as condoms, are
22
recommended. Discuss with your doctor when you may safely become pregnant after
therapy.
Do not breast feed while taking Doxorubicin.
People with congestive heart failure, those who have already had high doses of
Doxorubicin or a similar drug, and those with permanent problems with blood counts
(bone marrow suppression) cannot receive Doxorubicin.
Doxorubicin Self Care Tips:
Apply ice if you have any pain, redness or swelling at the IV site, and notify your doctor.
You may be at risk of infection so try to avoid crowds or people with colds, and report
fever or any other signs of infection immediately to your health care provider.
Wash your hands often.
To reduce nausea, take anti-nausea medications as prescribed by your doctor, and eat
small, frequent meals.
To help treat/prevent mouth sores, use a soft toothbrush, and rinse three times a day with
1 teaspoon of baking soda mixed with 8 ounces of water.
Use an electric razor and a soft toothbrush to minimize bleeding.
Avoid contact sports or activities that could cause injury.
Avoid sun exposure. Wear SPF 15 (or higher) sunblock and protective clothing.
Drink two to three quarts of fluid every 24 hours, unless you are instructed otherwise.
Get plenty of rest.
Maintain good nutrition.
In general, drinking alcoholic beverages should be minimized or avoided. You should
discuss this with your doctor.
If you experience symptoms or side effects, be sure to discuss them with your health care
team. They can prescribe medications and/or offer other suggestions that are effective in
managing such problems.
Monitoring and Testing While Taking Doxorubicin:
A baseline heart evaluation is recommended before starting treatment. A full blood count will be
done regularly, and a heart function test will be done as your doctor prescribes. Various tests to
monitor the function of other organs (such as your kidneys and liver) will also be ordered by
your physician.
How Doxorubicin Works:
Cancerous tumors are characterized by cell division, which is no longer controlled as it is in
normal tissue. “Normal” cells stop dividing when they come into contact with like cells, a
mechanism known as contact inhibition. Cancerous cells lose this ability. Cancer cells no
longer have the normalchecks and balances in place that control and limit cell division. The
process of cell division, whether normal or cancerous cells, is through the cell cycle. The cell
cycle goes from the resting phase, through active growing phases, and then to mitosis (division).
23
The ability of chemotherapy to kill cancer cells depends on its ability to halt cell division.
Usually, the drugs work by damaging the RNA or DNA that tells the cell how to copy itself in
division. If the cells are unable to divide, they die. The faster the cells are dividing, the more
likely it is that chemotherapy will kill the cells, causing the tumor to shrink. They also induce
cell suicide (self-death or apoptosis).
Chemotherapy drugs that affect cells only when they are dividing are called cell-cycle specific.
Chemotherapy drugs that affect cells when they are at rest are called cell-cycle non-specific. The
scheduling of chemotherapy is set based on the type of cells, rate at which they divide, and the
time at which a given drug is likely to be effective. This is why chemotherapy is typically given
in cycles.
Unfortunately, chemotherapy does not know the difference between the cancerous cells and the
normal cells. Chemotherapy will kill all cells that are rapidly dividing. The “normal” cells will
grow back and be healthy but in the meantime, side effects occur. The “normal” cells most
commonly affected by chemotherapy are the blood cells, the cells in the mouth, stomach and
bowel, and the hair follicles; resulting in low blood counts, mouth sores, nausea, diarrhea, and/or
hair loss. Different drugs may affect different parts of the body.
Doxorubicin is classified as an antitumor antibiotic. Antitumor antibiotics are made from natural
products produced by species of the soil fungus Streptomyces. These drugs act during multiple
phases of the cell cycle and are considered cell-cycle specific. There are several types of
antitumor antibiotics:
Anthracyclines: Doxorubicin, Daunomycin, Mitoxantrone, and Idarubicin
Chromomycins: Dactinomycin and Plicamycin
Miscellaneous: Mitomycin and Bleomycin
Note: We strongly encourage you to talk with your health care professional about your specific
medical condition and treatments. The information contained in this website is meant to be
helpful and educational, but is not a substitute for medical advice.
Cyclophosphamide (from www.chemocare.com)
Cyclophosphamide
(sye-kloe-FAHS-fah-mide)
Trade names: Cytoxan®, Neosar®
Chemocare.com uses generic names in all descriptions of drugs. Cytoxan is the trade name for
cyclophosphamide. Neosar is another name for cyclophosphamide. In some cases, health care
professionals may use the trade name cytoxan or other names neosar when referring to the
generic drug name cyclophosphamide.
24
Drug type: Cyclophosphamide is an anti-cancer (“antineoplastic” or “cytotoxic”) chemotherapy
drug. This medication is classified as an “alkylating agent.” (For more detail, see “How this
drug works” section below).
What this drug is used for:
Cancers treated with cyclophosphamide include: Hodgkin’s and non-Hodgkin's
lymphoma, Burkitt’s lymphoma, chronic lymphocytic leukemia (CLL), chronic
myelocytic leukemia (CML), acute myelocytic leukemia (AML), acute lymphocytic
leukemia (ALL), t-cell lymphoma (mycosis fungoides), multiple myeloma,
neuroblastoma, retinoblastoma, rhabdomyosarcoma, Ewing's sarcoma; breast, testicular,
endometrial, ovarian, and lung cancers, and in conditioning regimens for bone marrow
transplantation.
Cyclophosphamide is also used to treat many disorders that are not cancer.
Note: If a drug has been approved for one use, physicians may elect to use this same drug for
other problems if they believe it may be helpful.
How this drug is given:
Cyclophosphamide can be given can be given by a number of different routes. The route
that it is given depends on the dosage, the condition being treated, as well as the purpose
it is being used for.
It is usually given through a vein by injection or infusion (intravenous, IV) or by mouth
in tablet form, depending upon the diagnosis.
Cyclophosphamide is also approved to be given by a shot into a muscle (IM), into the
abdominal lining (intraperitoneal, IP), or into the lining of the lung (intrapleural).
Tablets should be given with food or after meals. Tablets should not be cut or crushed.
The amount of cyclophosphamide that you will receive depends on many factors,
including your height and weight, your general health or other health problems, and the
type of cancer or condition you have. Your doctor will determine your exact dosage and
schedule.
Side effects:
Important things to remember about the side effects of cyclophosphamide:
The side effects of cyclophosphamide and their severity depend on how much of the drug
is given. In other word, high doses may produce more severe side effects.
You will not get all of the side effects mentioned below.
Side effects are often predictable in terms of their onset, duration, and severity.
Side effects are almost always reversible and will go away after therapy is complete.
Side effects are quite manageable. There are many options to minimize or prevent them.
The following side effects are common (occurring in greater than 30%) for patients taking
cyclophosphamide:
25
Low blood counts. Your white and red blood cells and platelets may temporarily
decrease. This can put you at increased risk for infection, anemia and/or bleeding.
Nadir: Meaning low point, nadir is the point in time between chemotherapy cycles in which you
experience low blood counts.
Onset: 7 days
Nadir: 10-14 days
Recovery: 21 days
Hair loss. Temporary - usually begins 3-6 weeks after the start of therapy. Hair will grow
back after treatment is completed although the color and/or texture may be different.
Nausea and vomiting, more common with larger doses, usually beginning 6-10 hours
after therapy.
Poor appetite
Loss of fertility. Meaning, your ability to conceive or father a child may be affected by
cyclophosphamide. Discuss this issue with your health care provider.
Discoloration of the skin or nails (see skin reactions).
These are less common side effects for patients receiving cyclophosphamide:
Diarrhea
Mouth sores
Bladder irritation and bleeding (hemorrhagic cystitis) (see bladder problems)
Delayed effects:
There is a slight risk of developing a blood cancer such as leukemia or myelodysplasia
after taking cyclophosphamide. Talk to your doctor about this risk.
This list includes common and less common side effects for those taking cyclophosphamide. Side
effects that are very rare -- occurring in less than about 10 percent of patients -- are not listed
here. But you should always inform your health care provider if you experience any unusual
symptoms.
When to contact your doctor or health care provider:
Contact your health care provider immediately, day or night, if you should experience any
of the following symptoms:
Fever of 100.5º F (38º C) or higher, chills (possible signs of infection)
The following symptoms require medical attention, but are not an emergency. Contact
your health care provider within 24 hours of noticing any of the following:
Nausea (interferes with ability to eat and unrelieved with prescribed medication).
26
Vomiting (vomiting more than 4-5 times in a 24 hour period).
Diarrhea (4-6 episodes in a 24-hour period).
Unusual bleeding or bruising
Black or tarry stools, or blood in your stools.
Blood in the urine.
Pain or burning with urination.
Extreme fatigue (unable to carry on self-care activities).
Mouth sores (painful redness, swelling or ulcers).
Always inform your health care provider if you experience any unusual symptoms.
Precautions:
Before starting cyclophosphamide treatment, make sure you tell your doctor about any
other medications you are taking (including prescription, over-the-counter, vitamins,
herbal remedies, etc. Do not take aspirin, products containing aspirin unless your doctor
specifically permits this.
Do not receive any kind of immunization or vaccination without your doctor’s approval
while taking cyclophosphamide.
For both men and women: Use contraceptives, and do not conceive a child (get pregnant)
while taking cyclophosphamide. Barrier methods of contraception, such as condoms, are
recommended.
Do not breast feed while taking this medication.
Self-care tips:
Drink at least two to three quarts of fluid every 24 hours, unless you are instructed
otherwise.
It is important to void (empty your bladder) frequently especially in the first 24 hours
after taking cyclophosphamide. Report any pain or burning on urination to your health
care provider.
You may be at risk of infection so try to avoid crowds or people with colds, and report
fever or any other signs of infection immediately to your health care provider.
Wash your hands often
To help treat/prevent mouth sores, use a soft toothbrush, and rinse three times a day with
1 teaspoon of baking soda mixed with 8 ounces of water.
Use an electric razor and a soft toothbrush to minimize bleeding.
Avoid contact sports or activities that could cause injury.
To reduce nausea, take anti-nausea medications as prescribed by your doctor, and eat
small, frequent meals.
Avoid sun exposure. Wear SPF 15 (or higher) sunblock and protective clothing.
In general, drinking alcoholic beverages should be kept to a minimum or avoided
completely. You should discuss this with your doctor.
Get plenty of rest.
Maintain good nutrition.
27
If you experience symptoms or side effects, be sure to discuss them with your health care
team. They can prescribe medications and/or offer other suggestions that are effective in
managing such problems.
Monitoring and testing:
You will be checked regularly by your doctor while you are taking cyclophosphamide, to
monitor side effects and check your response to therapy. Periodic blood to monitor your
complete blood count (CBC) as well as the function of other organs (such as your kidneys and
liver) will also be ordered by your doctor.
How this drug works:
Chemotherapy (anti-neoplastic drugs):
Cancerous tumors are characterized by cell division, which is no longer controlled as it is in
normal tissue. “Normal” cells stop dividing when they come into contact with like cells, a
mechanism known as contact inhibition. Cancerous cells lose this ability. Cancer cells no
longer have the normal checks and balances in place that control and limit cell division. The
process of cell division, whether normal or cancerous cells, is through the cell cycle. The cell
cycle goes from the resting phase, through active growing phases, and then to mitosis (division).
The ability of chemotherapy to kill cancer cells depends on its ability to halt cell division.
Usually, the drugs work by damaging the RNA or DNA that tells the cell how to copy itself in
division. If the cells are unable to divide, they die. The faster the cells are dividing, the more
likely it is that chemotherapy will kill the cells, causing the tumor to shrink. They also induce
cell suicide (self-death or apoptosis).
Chemotherapy drugs that affect cells only when they are dividing are called cell-cycle specific.
Chemotherapy drugs that affect cells when they are at rest are called cell-cycle non-specific. The
scheduling of chemotherapy is set based on the type of cells, rate at which they divide, and the
time at which a given drug is likely to be effective. This is why chemotherapy is typically given
in cycles.
Unfortunately, chemotherapy does not know the difference between the cancerous cells and the
normal cells. Chemotherapy will kill all cells that are rapidly dividing. The “normal” cells will
grow back and be healthy but in the meantime, side effects occur. The “normal” cells most
commonly affected by chemotherapy are the blood cells, the cells in the mouth, stomach and
bowel, and the hair follicles; resulting in low blood counts, mouth sores, nausea, diarrhea, and/or
hair loss. Different drugs may affect different parts of the body.
Cyclophasphamide is classified as an alkylating agent. Alkylating agents are most active in the
resting phase of the cell. These drugs are cell-cycle non-specific. There are several types of
alkylating agents.
28
Mustard gas derivatives: Mechlorethamine, Cyclophosphamide, Chlorambucil,
Melphalan, and Ifosfamide.
Ethylenimines: Thiotepa and Hexamethylmelamine.
Alkylsulfonates: Busulfan.
Hydrazines and Triazines: Procarbazine, Dacarbazine and Temozolomide.
Nitrosureas: Carmustine, Lomustine and Streptozocin. Nitrosureas are unique because,
unlike most chemotherapy, they can cross the blood-brain barrier. They can be useful in
treating brain tumors.
Metal salts: Carboplatin and Cisplatin.
Note: We strongly encourage you to talk with your health care professional about your specific
medical condition and treatments. The information contained in this website is meant to be
helpful and educational, but is not a substitute for medical advice.
Paclitaxel (from www.chemocare.com)
Trade Names: Taxol ®, Onxal TM
Drug Type:
Paclitaxel is an anti-cancer ("antineoplastic" or "cytotoxic") chemotherapy drug. Paclitaxel is
classified as a "plant alkaloid," a "taxane" and an "antimicrotubule agent." (For more detail, see
"How Paclitaxel Works" section below).
What Paclitaxel Is Used For:
Paclitaxel is used for the treatment of breast, ovarian, lung, bladder, prostate, melanoma,
esophageal, as well as other types of solid tumor cancers. It has also been used in
Kaposi's sarcoma.
Note: If a drug has been approved for one use, physicians sometimes elect to use this same drug
for other problems if they believe it might be helpful.
How Paclitaxel Is Given:
Paclitaxel is given as an injection or infusion into the vein (intravenous, IV).
Paclitaxel is an irritant. An irritant is a chemical that can cause inflammation of the vein
through which it is given. If the medication escapes from the vein it can cause tissue
damage. The nurse or doctor who gives Paclitaxel must be carefully trained. If you
experience pain or notice redness or swelling at the IV site while you are receiving
Paclitaxel, alert your health care professional immediately.
Because severe allergic reactions have occurred in some people taking Paclitaxel, you
will be asked to take medications to help prevent a reaction. Your doctor will prescribe
the exact regimen.
29
Paclitaxel is given over various amounts of times and in various schedules.
There is no pill form of Paclitaxel.
The amount of Paclitaxel and the schedule that it is given will receive depend on many
factors, including your height and weight, your general health or other health problems,
and the type of cancer or condition being treated. Your doctor will determine your dose
and schedule.
Side Effects of Paclitaxel:
Important things to remember about the side effects of Paclitaxel include:
Most people do not experience all of the side effects listed.
Side effects are often predictable in terms of their onset and duration.
Side effects are almost always reversible and will go away after treatment is complete.
There are many options to help minimize or prevent side effects.
There is no relationship between the presence or severity of side effects and the
effectiveness of the medication.
The side effects of Paclitaxel and their severity vary depending on how much of the drug
is given, and/or the schedule in which it is given.
The following side effects are common (occurring in greater than 30%) for patients taking
Paclitaxel:
Low blood counts. Your white and red blood cells and platelets may temporarily
decrease. This can put you at increased risk for infection, anemia and/or bleeding.
Hair loss
Arthralgias and myalgias, pain in the joints and muscles. (see pain) Usually temporary
occurring 2 to 3 days after Paclitaxel, and resolve within a few days.
Peripheral neuropathy (numbness and tingling of the hands and feet)
Nausea and vomiting (usually mild)
Diarrhea
Mouth sores
Hypersensitivity reaction. Fever, facial flushing, chills, shortness of breath, or hives after
Paclitaxel is given (see allergic reaction). The majority of these reactions occur within
the first 10 minutes of an infusion. Notify your healthcare provider immediately
(premedication regimen has significantly decreased the incidence of this reaction).
The following are less common side effects (occurring in 10-29%) for patients receiving
Paclitaxel:
Swelling of the feet or ankles (edema).
Increases in blood tests measuring liver function. These return to normal once treatment
is discontinued. (see liver problems).
Low blood pressure (occurring during the first 3 hours of infusion).
Darkening of the skin where previous radiation treatment has been given (radiation recall
- see skin reactions).
30
Nail changes (discoloration of nail beds - rare) (see skin reactions).
Nadir: 15-21 days
This list includes common and less common side effects for individuals taking Paclitaxel. Side
effects that are very rare, occurring in less than 10% of patients, are not listed here. However,
you should always inform your health care provider if you experience any unusual symptoms.
When To Contact Your Doctor or Health Care Provider:
Contact your health care provider immediately, day or night, if you should experience any of the
following symptoms:
Fever of 100.5º F (38º C), chills (possible signs of infection)
Shortness of breath, wheezing, difficulty breathing, closing up of the throat, swelling of
facial features, hives (possible allergic reaction).
The following symptoms require medical attention, but are not an emergency. Contact your
health care provider within 24 hours of noticing any of the following:
If you notice any redness or pain at the site of injection
Nausea (interferes with ability to eat and unrelieved with prescribed medication)
Vomiting (vomiting more than 4-5 times in a 24 hour period)
Diarrhea (4-6 episodes in a 24-hour period)
Unusual bleeding or bruising
Black or tarry stools, or blood in your stools or urine
Extreme fatigue (unable to carry on self-care activities)
Mouth sores (painful redness, swelling or ulcers)
Yellowing of the skin or eyes
Swelling of the feet or ankles. Sudden weight gain
Signs of infection such as redness or swelling, pain on swallowing, coughing up mucous,
or painful urination.
Always inform your health care provider if you experience any unusual symptoms.
Paclitaxel Precautions:
Before starting Paclitaxel treatment, make sure you tell your doctor about any other
medications you are taking (including prescription, over-the-counter, vitamins, herbal
remedies, etc.). Do not take aspirin, or products containing aspirin unless your doctor
specifically permits this.
Do not receive any kind of immunization or vaccination without your doctor's approval
while taking Paclitaxel.
Inform your health care professional if you are pregnant or may be pregnant prior to
starting this treatment. Pregnancy category D (Paclitaxel may be hazardous to the fetus.
31
Women who are pregnant or become pregnant must be advised of the potential hazard to
the fetus).
For both men and women: Do not conceive a child (get pregnant) while taking Paclitaxel.
Barrier methods of contraception, such as condoms, are recommended. Discuss with your
doctor when you may safely become pregnant or conceive a child after therapy.
Do not breast feed while taking Paclitaxel.
Paclitaxel Self Care Tips:
Paclitaxel, or the medications that you take with Paclitaxel may cause you to feel dizzy or
drowsy. Do not operate any heavy machinery until you know how you respond to
Paclitaxel.
If you notice any redness or pain at the injection site, place a warm compress, and notify
your healthcare provider.
Drink at least two to three quarts of fluid every 24 hours, unless you are instructed
otherwise.
You may be at risk of infection so try to avoid crowds or people with colds and those not
feeling well, and report fever or any other signs of infection immediately to your health
care provider.
Wash your hands often.
To help treat/prevent mouth sores, use a soft toothbrush, and rinse three times a day with
1/2 to 1 teaspoon of baking soda and/or 1/2 to 1 teaspoon of salt mixed with 8 ounces of
water.
Use an electric razor and a soft toothbrush to minimize bleeding.
Avoid contact sports or activities that could cause injury.
Paclitaxel causes little nausea. But if you should experience nausea, take anti-nausea
medications as prescribed by your doctor, and eat small frequent meals. Sucking on
lozenges and chewing gum may also help.
Acetaminophen or ibuprophen may help relieve discomfort from fever, headache and/or
generalized aches and pains. However, be sure to talk with your doctor before taking it.
You may experience drowsiness or dizziness; avoid driving or engaging in tasks that
require alertness until your response to the drug is known.
Paclitaxel will make you sensitive to sunlight. You must wear sunglasses when outside,
and avoid sun exposure. Wear protective clothing, and also wear SPF 15 (or higher) sun
block.
In general, drinking alcoholic beverages should be kept to a minimum or avoided
completely. You should discuss this with your doctor.
Get plenty of rest.
Maintain good nutrition.
If you experience symptoms or side effects, be sure to discuss them with your health care
team. They can prescribe medications and/or offer other suggestions that are effective in
managing such problems.
Monitoring and Testing While Taking Paclitaxel:
32
You will be checked regularly by your health care professional while you are taking Paclitaxel,
to monitor side effects and check your response to therapy. Periodic blood work to monitor your
complete blood count (CBC) as well as the function of other organs (such as your kidneys and
liver) will also be ordered by your doctor.
How Paclitaxel Works:
Cancerous tumors are characterized by cell division, which is no longer controlled as it is in
normal tissue. "Normal" cells stop dividing when they come into contact with like cells, a
mechanism known as contact inhibition. Cancerous cells lose this ability. Cancer cells no
longer have the normal checks and balances in place that control and limit cell division. The
process of cell division, whether normal or cancerous cells, is through the cell cycle. The cell
cycle goes from the resting phase, through active growing phases, and then to mitosis (division).
The ability of chemotherapy to kill cancer cells depends on its ability to halt cell division.
Usually, the drugs work by damaging the RNA or DNA that tells the cell how to copy itself in
division. If the cells are unable to divide, they die. The faster the cells are dividing, the more
likely it is that chemotherapy will kill the cells, causing the tumor to shrink. They also induce
cell suicide (self-death or apoptosis).
Chemotherapy drugs that affect cells only when they are dividing are called cell-cycle specific.
Chemotherapy drugs that affect cells when they are at rest are called cell-cycle non-specific. The
scheduling of chemotherapy is set based on the type of cells, rate at which they divide, and the
time at which a given drug is likely to be effective. This is why chemotherapy is typically given
in cycles.
Chemotherapy is most effective at killing cells that are rapidly dividing. Unfortunately,
chemotherapy does not know the difference between the cancerous cells and the normal cells.
The "normal" cells will grow back and be healthy but in the meantime, side effects occur. The
"normal" cells most commonly affected by chemotherapy are the blood cells, the cells in the
mouth, stomach and bowel, and the hair follicles; resulting in low blood counts, mouth sores,
nausea, diarrhea, and/or hair loss. Different drugs may affect different parts of the body.
Paclitaxel belongs to a class of chemotherapy drugs called plant alkaloids. Plant alkaloids are
made from plants. The vinca alkaloids are made from the periwinkle plant (catharanthus rosea).
The taxanes are made from the bark of the Pacific Yew tree (taxus). The vinca alkaloids and
taxanes are also known as antimicrotubule agents. The podophyllotoxins are derived from the
May Apple plant. Camptothecan analogs are derived from the Asian "Happy Tree" (Camptotheca
acuminata). Podophyllotoxins and camptothecan analogs are also known as topoisomerase
inhibitors. The plant alkaloids are cell-cycle specific. This means they attack the cells during
various phases of division.
Vinca alkaloids: Vincristine, Vinblastine and Vinorelbine.
Taxanes: Paclitaxel and Docetaxel.
Podophyllotoxins: Etoposide and Tenisopide.
Camptothecan analogs: Irinotecan and Topotecan.
33
Antimicrotubule agents (such as Paclitaxel), inhibit the microtubule structures within the cell.
Microtubules are part of the cell's apparatus for dividing and replicating itself. Inhibition of
these structures ultimately results in cell death.
Note: We strongly encourage you to talk with your health care professional about your specific
medical condition and treatments. The information contained in this website is meant to be
helpful and educational, but is not a substitute for medical advice.
Proper set up of the Chemotherapy Closed system delivery set
{Insert details about your own system}
34