2014.12.25
advertisement
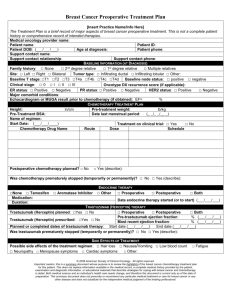
Hypoxia-inducible factors are required for chemotherapy resistance of breast cancer stem cell Proceedings of the National Academy of Sciences of the united states of American (PNAS) IF=9.8 PNAS | Published online December 1, 2014 | E5429–E5438 Background Possible origins of cancer stem cells 肿瘤的发生是一个多基因多步骤的基因变化效应,是多阶段或多次打击后产生的。正常 细胞转化为恶性肿瘤细胞需经历一个复杂而漫长的过程,至少需要4-7次突变,这需要很长的 时间。而与已分纯细胞相比,干细胞在体内分布广泛且更新能力强,更易发生恶性转化,这 意味着突变可能更容易在干细胞中得以积累。 BCSC and Breast Cancer 1. Although many breast cancer cells enter the circulation, only BCSCs are capable of forming a secondary tumor 2. BCSCs are also resistant to chemotherapy and the percentage of BCSCs following chemotherapy is increased compared with before therapy 3. A reduction in cancer cell burden of >95% may result in an apparent complete response to therapy, but may leave a population of residual BCSCs that represent the source of subsequent disease recurrence that will eventually lead to death of the patient. Breast cancer therapy is based on the classification of tumors into three groups A: estrogen receptor/progesterone receptor [ER/PR]+ cancers (60-70%) ER antagonists, such as tamoxifen, or aromatase inhibitors, such as letrozole B: human epidermal growth factor receptor 2 (HER2+) cancers (15-20%) anti-HER2 antibody, such as trastuzumab, or receptor tyrosine kinase inhibitor, such as lapatinib C: Triple negative breast cancers (TNBCs), which do not express ER, PR, or HER2(20%) Cytotoxic chemotherapy, such as paclitaxel or gemcitabine HIF and Drug resistance Microarray data from more than 500 human breast cancers revealed that one of the defining features of the basal molecular subtype is the increased expression of a large battery of genes that are regulated by hypoxia-inducible factors (HIFs) HIF-1 has been implicated in resistance to chemotherapy and in hypoxic colon cancer cells, HIF-1 activated expression of multidrug resistance 1 (MDR1), which mediates efflux of chemotherapy from cancer cells and represents a major mechanism underlying treatment failure. Increased expression of hypoxia-induced genes in breast cancer is also associated with poor prognosis. Methods 1. Cell Culture(MDA-MB-231+SUM-159+SUM-149 ) 2. RT –qPCR 3. Immunoblot assays 4. Luciferase Assay—HIF transcriptional activity 5. Aldefluor Assay--BCSC identification 6. Mammosphere Assay 7. MitoSox Staining--ROS Results 1. Paclitaxel Induces HIF Expression and Transcriptional Activity in TNBC Cells 2. Paclitaxel Treatment Increases the Percentage of BCSCs. 3. Paclitaxel-Induced Interleukin Expression Is Blocked by HIF Inhibitors 4. HIF-1 α and HIF-2 α Are Required for Paclitaxel-Induced BCSC nrichment Paclitaxel-Induced SMAD2 and STAT3 Activity Is Insufficient to Induce BCSC Enrichment TLR-4 and NF- κ B Do Not Mediate ChemotherapyInduced BCSC Enrichment. 5. Increased ROS Levels Mediate Induction of HIF-1 α and Enrichment of BCSCs 6. Paclitaxel-Induced MDR1 Expression Is Blocked by HIF Inhibitors 7. Digoxin Blocks PaclitaxelInduced BCSC Enrichment in Vivo 8. HIF Signature Predicts Mortality of Patients Treated with Chemotherapy DISCUSSION We have demonstrated that treatment of three different TNBC cell lines with clinically relevant concentrations of paclitaxel or gemcitabine increases ROS levels, which induce HIF-1 α and HIF-2 α mRNA and protein expression, leading to the HIFdependent expression of MDR1, IL-8, and/or IL-6, and to BCSC enrichment, both in vitro and in vivo