CCNM Patient Profile – Adult - Champlain Center for Natural Medicine
advertisement

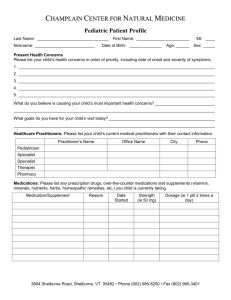
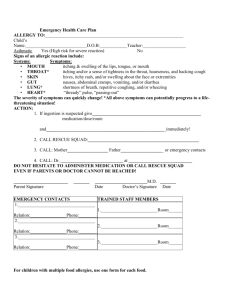
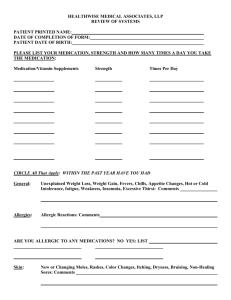
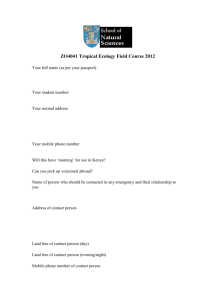
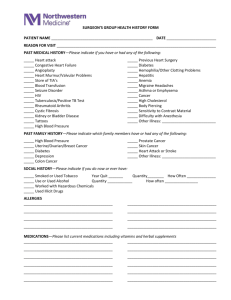
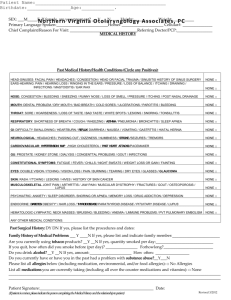
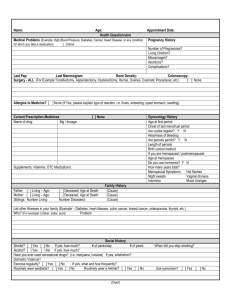
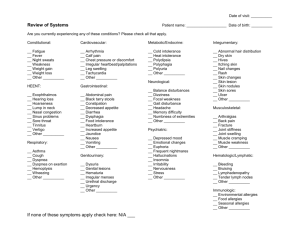
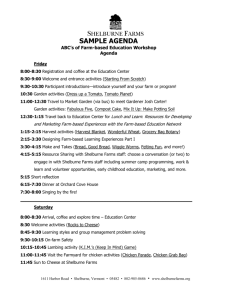
CHAMPLAIN CENTER FOR NATURAL MEDICINE Adult Patient Profile Last Name: _______________________________ First Name: _______________________ Nickname: __________________________ Date of Birth: ______________ MI: ____ Age: ______ Sex: _____ Present Health Concerns Please list your health concerns in order of priority, including date of onset and severity of symptoms. 1. _____________________________________________________________________________________ 2. _____________________________________________________________________________________ 3. _____________________________________________________________________________________ 4. _____________________________________________________________________________________ 5. _____________________________________________________________________________________ What do you believe is causing your most important health concerns? _______________________________ _______________________________________________________________________________________ What goals do you have for your visit today? ___________________________________________________ _______________________________________________________________________________________ Healthcare Practitioners: Please list your current medical practitioners with their contact information. Practitioner’s Name Office Name City Phone Primary Care OB/Gyn Specialist Therapist Other Pharmacy Medications: Please list any prescription drugs, over-the-counter medications and supplements (vitamins, minerals, nutrients, herbs, homeopathic remedies, etc.) you are currently taking. Medication/Supplement Reason Date began Dose Allergies: Please list and describe any severe or life-threatening allergies (medications, stings, foods, etc.): ________________________________________________________________________________ (OVER) 3804 Shelburne Road, Shelburne, VT 05482 • Phone (802) 985-8250 • Fax (802) 985-3401 Review of Systems: Check symptoms that you currently experience. Constitutional Max weight: _____ Year: ____ Min weight: ______ Year: ____ Appetite change Weight change Fevers or Chills Sweats Feel hot or cold Fatigue Weakness Eyes Eye pain Poor night vision Glasses or Contacts Near or Far sighted Blurred or Double vision Cataracts Dry eyes Ears, Nose, Mouth, Throat Ringing in ears Earaches Itchy ears Excessive ear wax Hearing loss or hearing aid Nosebleeds Stuffy or Runny nose Postnasal drip Sinus problems Change in taste or smell Teeth / Gum problems Grinding teeth Dentures Mouth sores Dry mouth Sore throat Hoarseness Jaw clicking or pain Facial pain Immune System Frequent infections Allergies to food Allergies to environment Lymph gland swelling / pain Other: Heart & Circulation Heart murmur Irregular heartbeat Chest pain Heart palpitations Lightheaded Fainting Blood clots Deep leg pain on walking Varicose veins Swelling of feet / ankles Cold hands / feet Anemia Easy bruising Bleeding tendency Blood transfusions Chest & Lungs Shortness of breath At rest Walking Lying down Wheezing or asthma Cough: wet or dry Breast lump or pain Nipple discharge Self breast exams Neurological Dizziness Poor balance Poor coordination Tremors or shaking Seizures Headaches Migraines Numbness or tingling Nerve pain Memory loss Poor concentration Changes in speech Mental / Emotional Mood swings Anger, frustration, irritability Sadness or anxiety Phobias Insomnia or disrupted sleep Other: Digestion & Intestine Bad breath Excessive thirst Difficulty swallowing Indigestion Belching Heartburn / Reflux Nausea Vomiting Abdominal pain or cramping Gas or Bloating # Bowel movements/ day: ____ Constipation Loose stools or Diarrhea Mucus in stool Blood in stool Rectal pain/itching Hemorrhoids Hernia Jaundice Muscles, Bones & Joints Neck pain Back pain Muscle pain Joint Pain: indicate R or L wrist fingers elbow shoulder hip knee ankle foot Joint swelling Morning stiffness: ___hours Joint replacements Muscle weakness Muscle cramps Skin, Hair, Nails Acne Rashes Itching or hives Dry skin or eczema Moles or growths Poor wound healing Hair loss Nail problems Other: WOMEN: Reproductive Age period started: _____ yrs Length of cycle: _______ days Length of flow: _______ days Last menstrual period: _______ # Pregnancies: _______ # Live births: _______ # Miscarriages: _______ # Abortions: _______ Last pap smear: ___________ Last mammogram: _________ Last Bone scan: ___________ Irregular menstrual cycle Bleeding between periods Heavy periods Painful periods Premenstrual syndrome Pelvic pain Abnormal pap smear Vaginal discharge Vaginal itching or soreness Sores on genitals Infertility Sexual difficulties Pain with intercourse Menopausal symptoms Hormone Replacement MEN: Reproductive Sores on genitals Discharge Testicle lump/swelling/pain Prostate problems Infertility Sexual difficulties Self testicular exam Bladder & Kidney Waking to urinate Loss of bladder control Frequent / Urgent urination Interrupted flow Recurrent infections Painful urination Blood or pus in urine Kidney stones 3804 Shelburne Road, Shelburne, VT 05482 • Phone (802) 985-8250 • Fax (802) 985-3401 Past Medical History: Please list the date of or age at each event and describe: Serious Illnesses and Injuries: _______________________________________________________________ Surgeries: ______________________________________________________________________________ Hospitalizations: _________________________________________________________________________ Date of last physical/annual exam: ________________________ Date of last blood tests: _____________ Childhood Illnesses: Please check all that apply. Your health as a child was: Good Fair Poor Chicken Pox Mononucleosis (Mono) Rheumatic Fever Diphtheria Mumps Tonsillitis Ear Infections Pertussis (whooping cough) Scarlet Fever German Measles (Rubella) Pneumonia Strep Throat (recurrent) Measles Polio Personal and Family Medical History: Please check the box next to each condition that applies to you or one of your biological family members. YOU Mom Dad PGM Grandparents PGF MGM Siblings MGF Current Age or Age at Death Alcohol / Drug Abuse Allergies or Hay Fever Alzheimer’s or Dementia Anemia Anxiety / Panic Attacks Arthritis / Joint Disease Asthma Autoimmune Disease Bleeding Disorder Cancer (what type?) Celiac Disease Crohns Dis / Ulcerative Colitis COPD / Emphysema Depression / Suicide attempt Diabetes Eczema Epilepsy or Seizures Glaucoma Gall Bladder Disease Migraines / Headaches Heart Attack Heart Disease High Blood Pressure High Cholesterol HIV / AIDS Kidney Disease Liver Disease / Hepatitis Osteoporosis Schizophrenia Stroke Thyroid disorder Other: 3804 Shelburne Road, Shelburne, VT 05482 • Phone (802) 985-8250 • Fax (802) 985-3401 Social History Marital status: Single Married Civil Union Divorced Widowed Significant Other Do you have any children? Yes No Please list their age(s): ___________________________________ Household: Alone Roommate(s) Spouse/Significant other Children Grandchildren Parent Education level: High school College Professional school Other: _________________________ Occupation: Student Work Homemaker Unemployed Volunteer Retired Disability School/Job(s): ______________________________________________ Hours per week: _______________ Memories of your childhood: Mostly happy Mostly painful Normal Don’t recall Do you find your life: Unsatisfactory Too demanding Boring Satisfactory Wonderful Lifestyle and Personal Habits: What are your primary sources of stress? _______________________________________________________ How much does stress impact your life? ____________________ Hours of play/relaxation per week? ______ How do you manage stress and take care of yourself? _____________________________________________ Are you: Currently sexually active? Yes No Partners: # ___ Male Female Contraception: _______ Satisfied with your sex life? Yes No If no, why? ________________________________________ Satisfied with your social life? Yes No If no, why? ________________________________________ Satisfied with your spiritual life? Yes No If no, why? ________________________________________ Do you: Enjoy your job? Yes No If no, why? ________________________________________ Exercise regularly? Yes No If no, why? ________________________________________ Which activities? ___________________________________________________________________ Sleep soundly and wake rested? Yes No If no, why? ________________________________________ Smoke cigarettes? Yes No Quit date _______ Total years: ______ Packs /day: ______ Drink alcohol? Yes No Quit date _______ Type: _________ Drinks /week: ______ Use recreational drugs? Yes No Quit date _______ Type: ___________ How often: ______ Drink caffeinated beverages? Yes No Type? __________________________ Drinks /day: ______ Diet: Please describe your typical meals. Breakfast Time:_______ Lunch Time:_______ Dinner Time:_______ Snacks Times:________ Do you have any dietary restrictions? __________________________________________________________ How often do you eat out? __________________ What are your food cravings? ______________________ Water: ________ ounces per day Other beverages: ____________________________________________ What else would you like us to know about you? This form has been reviewed by the doctor with the patient. ____________________________________ ____________________________________ Signature of Patient Signature of Doctor Date Date 3804 Shelburne Road, Shelburne, VT 05482 • Phone (802) 985-8250 • Fax (802) 985-3401