Role of the Clinical Pharmacist in Reducing Decision-to
advertisement

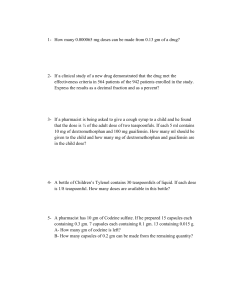
T-13 Role of the Clinical Pharmacist in Reducing Decision-to-Needle tPa Times During Code Stroke in the Emergency Department Authors: Kevin Brandon RPh, Clinical Pharmacist; Amanda Kramer RN, BSN-Emergency Department Clinical Advisor; Catherine Mulawka RN, MBA, Stroke Coordinator & Clinical Projects Advisor Background: Clinical observation revealed inconsistent ED decision-to-needle tPa times due to differing processes including pharmacist mixing in the central pharmacy, ED RN mixing at the bedside, and holding the tPa vial for stroke neurologist to mix upon arrival at the bedside Purpose: Implement a consistent process for tPa calculation and mixing Reduce decision-to-needle times, increasing the opportunity for successful patient outcome Method: Conduct retrospective chart review to establish baseline tPa decision-to-needle times in the ED Review current process of calculating, mixing, and administering tPa Identify areas for process streamlining and reducing potential for error by calculating and mixing tPa at the bedside Established goal of zero minute decision-to-needle time Clinical Pharmacist added to Code Stroke pager team in May 2010 Initial Clinical Pharmacist role consisted of dose calculation and verification with ED nurse at bedside Expanded Clinical Pharmacist role to include mixing tPa at beside in conjunction with nurse, while maintaining compliance with USP 797 Guidelines* Implement process of bedside conference between Clinical Pharmacist and ED RN to identify eligible candidates, allowing the Clinical Pharmacist to prepare tPa in preparation of anticipated administration Clinical Pharmacist’s role progressed to include immediate bedside medication education to patient and/or family, including verbal and written education materials Results: Addition of Clinical Pharmacist to Code Stroke team, with responsibility of calculating and mixing tPa at the bedside, has resulted in improved zero minute decision-to-needle times. 2010: zero minute decision-to-needle time not achieved 2011: zero minute decision-to-needle achieved in 60% of administrations 2012: (through July): zero minute decision-to-needle achieved in 78% of administrations Conclusion: Addition of a Clinical Pharmacist to the Code Stroke team resulted in a reduction of decision-toneedle tPa times in the Emergency Department Implications for Practice: Utilization of Clinical Pharmacist during Code Stroke to calculate and mix tPa reduces decision-toneedle time * http://www.emlab.com/s/services/USP_797.html