The overall goals of chronic kidney disease therapy are to:
advertisement

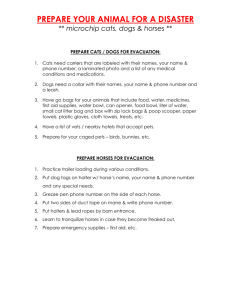
Characterizing and treating chronic kidney disease in dogs and cats Linda E. Luther, DVM, DACVIM (SAIM) Small Animal Track November 2012 The overall goals of chronic kidney disease therapy are to: Minimize clinical signs Slow disease progression Preserve/enhance Body Condition Score (BCS) CATER THERAPY TO THE CHARACTERISTICS OF EACH INDIVIDUAL CASE. Note: Don’t forget to rule out prerenal azotemia first! (Urine specific gravity > 1.030 in dogs, > 1.035-1.040 in cats) How can you tell if it is chronic vs. acute kidney disease? History (> 3 months) Hematocrit BCS Kidney size Why call it chronic kidney disease (CKD) vs. chronic renal failure (CRF)? Condition is progressive At time of diagnosis, quality life remains Encourages therapy Don’t ignore poor long term prognosis though IRIS (International Renal Interest Society) CKD Staging (www.iris-kidney.com) Diagnosis, prognosis and therapy recommendations CKD Stages 1-4 Staging is based on at least two creatinine levels when the animal is fasted and well hydrated. Proteinuria and blood pressure are also substaged. If creatinine is > 2 mg/dL (Stage 2-4 cats, Stage 3-4 dogs): A renal diet is recommended. Prevents/delays onset of uremia and premature death, decreases proteinuria, improves quality of life Protein, phosphorus, sodium and calcium are restricted. Omega-3 fatty acids, antioxidants, B vitamins, soluble fiber and potassium (feline diets) are added. Increased caloric density (higher in fat, watch if a dog has a history of pancreatitis) Neutral effect on acid-base balance Decreased body condition score and inappetance Uremic gastritis/oral ulcers may be factors. Decreased caloric intake can also contribute to anemia, azotemia. Treat with famotidine, mirtazapine. Hydration status Maintain hydration **Encourage water consumption SQ or IV fluids can be used, but the fluids available may contain too much sodium Proteinuria Localize (renal vs. post renal) o If urine sediment is active, post renal proteinuria exists. o If urine sediment is inactive, run urine protein/creatinine ratio to quantify renal proteinuria. Persistent/significant? o Document 3x at 2-week intervals if not azotemic. o Rule out infectious disease, recent vaccination, etc… Therapy o Renal diet o ACE inhibitors (enalapril vs. benazepril) o Spirinolactone? o Omega-3 fatty acids o Low-dose aspirin (0.5 mg/kg q 24 h in dogs only) o Immunosuppression? Hypertension (BP > 160 mmHg) Amlodipine in cats (0.625 mg/cat q 24 h) ACE inhibitor in dogs to start. Add amlodipine if necessary. Hypokalemia Especially in cats! “Pathophysiologic justification” vs. evidence Oral potassium gluconate (2 mEq/4.5 kg body weight BID with meals) Adequate potassium (KCl) should be added to IV and SQ fluids (see table below): (From DiBartola SP and De Morais HA , 2012) Potassium level (mEq/L) KCl (mEq/L) < 2.0 2.1-2.5 2.6-3.0 3.1-3.5 3.6-5.0 80 60 40 28 20 Max infusion (mL/kg/hr) (< 0.5 mEq/kg/hr) 6 8 12 18 25 Hyperphosphatemia First treat with a phosphorus restricted diet. If still hyperphosphatemic, then treat with phosphorus binders (given with food) o Aluminum hydroxide (compounded if needed) (30-45 mg/kg BID) o Ca salts Epakitin™: Chitosan and CaCarbonate Hyperparathyroidism (HPTH) Underlying calcitriol deficit results in HPTH. Parathyroid hormone (PTH) is a uremic toxin (contributes to symptoms). Hyperphosphatemia is a marker/predictor of HPTH. HPTH may also exist w/normal phosphorus levels. Total and ionized calcium can be normal, increased or decreased. First control hyperphosphatemia/keep phosphorus in low normal range with diet/phosphorus binders (see above). Then consider calcitriol. Calcitriol therapy should decrease PTH. o Dose approx.. 2-3 ng/kg/day or pulse therapy (9 ng/kg q 3.5 d or Wed. PM/Sun AM). Give on an empty stomach. o Do not use if hypercalcemic. Do not use calcium containing phosphorus binders concurrently. o Monitor by measuring PTH, ionized calcium and phosphorus. o Dogs: Increased survival shown w/calcitriol tx if IRIS stages 3 & 4. o Cats: Unproven, clinical observations positive, “pathophysiologic justification”. Anemia Mechanisms: Decreased erythropoietin, blood loss, decreased red blood cell lifespan due to uremia Treat when hematocrit < 20% o Epoetin (Procrit®, Epogen®) Cats and dogs: 100 IU/kg SQ 3x/wk then 50-100 IU/kg 2x/wk 25-30% of cats develop anti-EPO antibodies o Darbepoetin (Aranesp®) Cats: 1 ug/kg once weekly Longer half life, so less frequent administration One study, 56% of cats responded Less immunogenic? o Side effects: Hypertension, EPO antibodies, seizures o Concurrent iron dextran injections (10 mg/kg IM q. 3-4 weeks for cats) or ferrous sulfate (100-300 mg/dog/day PO) is recommended. o Goal hematocrit cat 25-30%; dog 30-35% Positive culture, pyuria Nonconcentrated urine may not show pyuria or bacturia in sediment. One study, 29% CKD w/occult urinary tract infections, so run cultures (w/MICs). Metabolic acidosis If bicarbonate < 15 mmol/L (more of a problem during a uremic crisis), treat with: o Renal diet first o Sodium bicarbonate or potassium citrate can be added to food. Ureteral calculi Weigh benefits vs. risks of surgical vs. medical management Medical therapy can include fluids, diuretics, amitriptyline, pain medications, control of CaOx calculi Chronic kidney disease (CKD): Problem-based therapeutic plans Parameter Urine specific gravity Chronic vs. acute IRIS CKD stage dogs IRIS CKD stage cats Plan If ≥ 1.030 in dogs, ≥1.035-1.040 in cats, then elevated creatinine = prerenal azotemia. Chronic if > 3 month history, decreased BCS, hematocrit or kidney size, and/or increased parathyroid gland size 1: Cr<1.4 mg/dL; 2: Cr 1.4-2 mg/dL; 3: Cr 2-5 mg/dL; 4: Cr>5 mg/dL 1: Cr<1.6 mg/dL; 2: Cr 1.6-2.8 mg/dL; 3: Cr 2.8-5 mg/dL; 4: Cr>5 mg/dL Creatinine > 2 mg/dL Renal diet Decreased BCS/Appetite Famotidine, mirtazapine, feeding tube Hydration status Encourage water consumption, give SQ or IV fluids to normalize Proteinuria If dipstick positive and quiet urine sediment, do urine protein/creatinine ratio Urine Pr/cr ratio If > 0.5 in dogs, > 0.4 in cats, treat with diet change, ACE inhibitor, spirinolactone, omega-3 FAs and in dogs, aspirin. Consider immunosuppression in dogs. If 0.2-0.5 in dogs, 0.2-0.4 in cats, monitor Systemic hypertension (BP > 160 mmHg) Amlodipine in cats, ACE inhibitor +/- amlodipine in dogs Hypokalemia Oral potassium gluconate supplement and/or supplement fluids w/KCl Hyperphosphatemia Hyperparathyroidism Anemia Positive urine culture, pyuria Leptospirosis titer/PCR Metabolic acidosis (HCO3 < 15 mmol/L) Ureteral calculi First, phosphorus restricted diet, then phosphorus binders w/meals: AlOH, calcium carbonate, Epikatin (Ca carbonate+chitosan) First, control hyperphosphatemia (see above), then rx calcitriol If hct < 20%, consider epoetin or darbepoetin and iron supplementation. Goal hct of 25-30% cats; 30-35% dogs Antibiotics Antibiotics if positive or suspected Renal diet, sodium bicarbonate, potassium citrate Medical or surgical therapy Therapy of CKD references Chalhoub S, Langston, Farrelly J. The use of darbepoetin to stimulate erythropoiesis in anemia of chronic kidney disease in cats: 25 cases. J Vet Intern Med 2012;26:363-369. Cortadellas O, del Paacio F, Talavera J, Bayón A. Calcium and phosphorus homeostasis in dogs with spontaneous chronic kidney disease at different stages of severity. J Vet Intern Med 2010;24:73-79. DiBartola SP, De Morais, HA. Disorders of potassium: Hypokalemia and hyperkalemia. In DiBartola SP (ed), Fluid, Electrolyte, and Acid-Base Disorders in Small Animal Practice. Elsevier Saunders, St. Louis, MO, 2012, 92-119. Graur GF. Proteinuria: Implications for management. In Kirk’s Current Veterinary Therapy XIV. Bonagura JD, Twedt DC (eds). Elsevier Saunders, St. Louis, MO., 2009, 860-863. IRIS 2009 Staging CKD and IRIS 2009 Treatment Recommendations Summary. IRIS (International Renal Interest Society) website: http://www.iriskidney.com/guidelines/en/index.shtml Kyles AE, Hardie EM, Wooden BG et al. Management and outcome of cats with ureteral calculi: 153 cases (1984-2002). J Am Vet Med Assoc 2005;226:937-944. Lees GE, Bahr A. Renal biopsy. In Nephrology and urology of small animals, Bartges J and Polzin DJ (eds), Wiley-Blackwell, Ames, IA, 2011, 209-214. Polzin DJ. Chronic kidney disease. In Textbook of Veterinary Internal Medicine, 7th ed., Ettinger SJ, Feldman EC (eds), Saunders Elsevier, St. Louis, MO, 2010, 1990-2021. Polzin DJ, Osborne CA, Ross S. Evidence-based management of chronic kidney disease. In Kirk’s Current Veterinary Therapy XIV. Bonagura JD, Twedt DC (eds). Elsevier Saunders, St. Louis, MO, 2009, 872-879. Schenck PA, Chew DJ, Nagode LA, Rosol TJ. Disorders of calcium: Hypercalcemia and hypocalcemia. In DiBartola SP (ed), Fluid, Electrolyte, and Acid-Base Disorders in Small Animal Practice. Elsevier Saunders, St. Louis, MO, 2012, 120-194. Vaden SL, Grauer GF. Glomerular disease. In Nephrology and urology of small animals, Bartges J and Polzin DJ (eds), Wiley-Blackwell, Ames, IA, 2011, 538-546. Disclaimer: Please verify all drug dosages before administering.