BLEEDING DISORDERS
advertisement
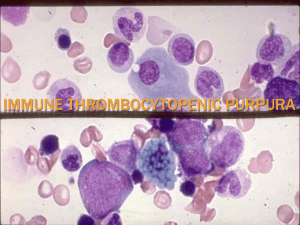
BLEEDING DISORDERS AN OVERVIEW WITH EMPHASIS ON EMERGENCIES CLASSIFICATION • • • PLATELET DISORDERS AND VASCULAR COMPONENTS COAGULATION ABNORMALITIES OTHER VASCULAR AND PLATELET ABNORMALITIES • Vascular - hereditary – Hereditary hemorrhagic telangiectasia – Ehlers-Danlos syndrome • - acquired – – – – “senile purpura” Henoch-Schonlein syndrome Scurvy - Amyloid Steroid purpura Acquired Coagulation Disorders • • • • • Vitamin K deficiency Warfarin therapy Liver disease DIC Antibodies against factor VIII (or other factors) • Massive transfusion • Thrombocytopenia – False reading • Clumping of platelets • Platelet satelitism – Margination in congestive splenomegaly – True thrombocytopenia • Failure to produce platelets – Acquired - drugs - alcohol – Inherited – TAR, May-Hegglin. Wiscott-Aldrich • Platelet destruction – Immune – TTP – DIC • Disorders of platelet function – Inherited • • • • Von Willebrand’s disease Glanzmann’s Bernard-Soulier Storage pool disease – gray platelets – Acquired • • • • Drugs MDS Multiple myeloma – hyperglobulinemia Uremia COAGULATION DISORDERS • Hemophilias A & B • Others • Von Willebrand’s disease Inherited Coagulation Disorders • Factor VIII deficiency may be severe <1%, moderate 1-5%, or mild 5-20% activity • After repeated doses of Factor VIII patients may develop and antibody against the factor – Treatment then requires bypassing the factor to effect hemostasis with FEIBA or Factor VIIa – Rarely the low concentration of antibody can be taken up by larger amounts of factor VIII • Other inherited factor deficiencies – Factor XI – mostly in Ashkenazi Jews • Bleeding is usually mild except after surgery or significant injury • XI concentrate may be available or give plasma – Factor XIII deficiency is rare and is similar to XI deficiency in clinical presentation – Factor VII and X deficiencies are seen and are variable in severity from case to case True Emergencies • • • • • Hemophilia A or B with bleeding TTP DIC ITP with bleeding Factor inhibitor with bleeding True Emergencies • Remember that bleeding can occur because of injury with no bleeding diathesis! • Hemophilia A or B with bleeding • TTP • DIC • ITP with bleeding • Factor inhibitor with bleeding Management of the Emergency • Be sure you have a proper diagnosis. • Remember the things you must not do, if there are any. • Be sure that the institution has the capacity to deal with the problem. – Available medications – Available procedures and equipment Injured or Postoperative Patients • With no history of bleeding in the past (or no history at all) – Do the diagnostic things – PT/PTT, Plt and PFT – If above are normal think of an open vessel. Hemophilia • Diagnosis is based on the Factor level and the history • Replacement of factor is the main thing • Remember antibodies Thrombotic Thrombocytopenic Purpura • Diagnosis is made by finding 3 of 5 features. – – – – – Microangiopathic hemolytic anemia Thrombocytopenic purpura Fever Neurologic abnormalities Renal failure TTP • Things to avoid. – Don’t waste time. This is a serious, rapidly progressive and fatal illness. – Transfusion of blood cells, especially platelets, can accelerate the disease. TTP Treatment • Plasma infusion in large amounts. This almost always means plasmapheresis, using plasma to replace volume for volume. • Other treatment with pheresis includes: – ASA and persantine – Prednisone DIC • Diagnsis is ever so important TTP – Warning! • Do not try to take care of TTP in a hospital that doesn’t have pheresis and a blood bank able to handle the demands. • Immediate transfer to a hospital that has these capacities is in order. • Before transfer, you might consider giving 2 – 3 units of FFP