Hematopoietic drugs
advertisement

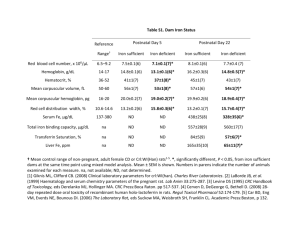
HEMATOPOIETIC DRUGS Diana Pendicheva1, Galya Stavreva1, Ivan Lambev2 1Faculty of Medicine, Medical University – Pleven 2Faculty of Medicine, Medical University – Sofia Introduction Hematopoiesis (formation of blood) is a complex process of proliferation, differentiation, and maturation of cellular components of blood (erythrocytes, leucocytes and platelets) from the bone marrow stem cells. It is regulated by balanced interaction between endogenously derived hematopoietic growth factors and exogenously supplied essential nutrients (hematinics). Inadequate supply of either the growth factors or the hematinics results in deficiency of normal blood cells which is manifested as anemia, thrombocytopenia or neutropenia. Hematopoietic growth factors are glycoproteins that control and maintain the production of various blood cell lineages from pluripotent hematopoietic stem cells and multipotent progenitors. A number of these factors (also called cytokines) have been cloned and produced for clinical use: Erythropoietin; Myeloid Growth Factors (Colony Stimulating Factors) – Granulocyte-Macrophage Colony Stimulating Factor (GM-CSF) and Granulocyte Colony Stimulating Factor (G-CSF); and Megacariocyte (Thrombopoietic) Growth factors – Interleukin-11 and Trombopoietin. Hematincs (iron, vitamin B12 and folic acid) and accessory hematinics (vitamin C, riboflavin, pyridoxine and certain minerals like Cu, Co and Mn) are also necessary for blood cell maturation and physiological turnover under basal conditions and on demand. Anaemia is the most common objective sign of a deficiency in oxygen-carrying erythrocytes. It is classified according to the size of erythrocytes (microcytic and macrocytic or megaloblastic) and their haemoglobin content (hypochromic or hyperchromic) or to the cause of the condition: haemorrhagic anaemia (due to acute or chronic blood loss), haemolytic anaemia (due to damaged red cell membranes and destruction of erythrocytes), aplastic and hypoplastic anaemia (caused by bone marrow damage), deficiency of essential nutrients (iron deficiency anemia, megaloblastic anemias) and genetic alteration in the hemoglobin molecule (hemoglobin-S in Sickle cell anemia). Thrombocytopenia and neutropenia are not rare and CSF therapy is used for their prevention and treatment in patients with immune deficiency, being on radiotherapy or receiving myelosuppressive chemotherapy. Classification of hematopoietic drugs A. Drugs for Anemia 1. Drugs for treatment of iron deficiency (microcytic, hypochromic) anemia 1.1. Oral preparations of iron (Fe2+) Ferrous sulfate: Ferro-gradumet, Hemofer prolongatum (film-tabl. 325 mg, 105 mg Fe2+; 1 tab. b.i.d. after meals), Tardyferon depot (80 mg Fe2+ included in mucoprotein obtained from intestinal mucosa of sheep; absorption continues 7 h; 1-2 tab. q.d.) Ferrous glutamate: Glubifer Ferrous aspartate: Ferrospartin (tab. 350 mg, 50 mg Fe2+) Ferrous fumarate: Ferronat Ferrous gluconate: TOTHEMA® (amp. Fe2+ gluconate 50 mg; Mn2+ gluconate; Cu2+ gluconate) Ferric hydroxide polymaltose complex: Maltofer (1 ml sol. contains 50 mg unionized Fe3+ hydroxide polymaltose complex) 1.2. Parenteral preparations of iron (Fe3+) Iron sucrose complex:, Venofer Iron isomaltoside: Monofer Iron dextran: Dexferrum®* Sodium ferric gluconate complex: Ferrlecit® 2. Drugs for treatment of megaloblastic (macrocytic, hyperchromic) anemias Vitamin B12 (Cyanocobalamin) – amp. 250 mcg/1 ml i.m. Folic acid Iron chelators: Deferoxamine (Desferal), Deferasirox (Exjade) B. Hematopoietic Growth Factors 1. Erythropoietins Erythropoietin: Epoetin alfa (Eprex), Epoetin beta (Recormon) Darbepoetin alfa (Aranesp) Methoxy polyethylene glycol-epoetin beta (long-acting erythropoietin receptor activator): Mircera 2. Myeloid growth factors Granulocyte Colony Stimulating Factor (G-CSF): Filgrastim (Neupogen), Lenograstim (Granocyte) Granulocyte-Macrophage Colony Stimulating Factor (GM-CSF): Molgramostim (Leucomax), Sargramostim (Leukine) 3. Megakaryocyte (Thrombopoietic) Growth Factors Oprelvekin (IL-11): Newmega Thrombopoietin Mechanisms of action and pharmacological effects 1. Drugs for treatment of iron deficiency Iron deficiency anemia is microcytic hypochromic anemia, caused by insufficient supply of iron. It is the most common type of anemia. Iron deficiency in normal conditions may occur more often in women (with menstrual blood loss or pregnancy), in adolescents (increased demand) and in vegetarians or persons with malnutrition (inadequate dietary iron intake). 2 Pharmacokinetics of iron: Haemoglobin is a protoporphyrin and each molecule has 4 iron-haeme residues. Haeme is responsible for the bulk of oxygen transport in the blood and iron is the essential metallic component of it. The total body iron is about 3.5–4 g in men and 2.5 g in women, and over 70% of it circulates in the blood as haemoglobin. About 15-18% is stored in the liver, spleen and bone marrow mainly as ferritin and haemosiderin. Maximum iron absorption occurs by active transport in the duodenum and proximal jejunum. Absorption rate depends on the ratio of apoferitin (a protein) to feritin (apoferitine-iron complex) in the intestinal mucosa. The so called “mucosal block” is a mechanism that prevents the entry of excess iron in the body. Ascorbic acid and SHgroup containing amino acids (in gastric juice) facilitate Fe3+ to Fe2+ conversion and promote its absorption. Iron absorption is hindered by coffee, tea, antacid agents, phosphates (rich in egg yolks), tetracyclines, etc. In the body iron is distributed into: haemoglobin (Hb) – 66%; iron storages (ferritin and haemosiderin) – 25%, myoglobin in muscles – 3%, and parenchimal iron (as prostetic group in cytochrome, peroxidases, catalases, xanthine oxidases and other cellular enzymes) – 6%. Haemoglobin contains 0.33% iron and 50 mg elemental iron is averagely lost with the loss of 100 ml blood (15 g Hb). Iron preparations: Treatment or prevention of iron deficiency anemia is the only clinical indication for the use of iron preparations. The preferred route of iron administration is oral. Elemental iron quantity per dose should be taken into consideration. Oral preparations contain ferrous (Fe2+) salts (sulfate, glutamate, aspartate, fumarate, gluconate, succinate, etc.). Ferric (Fe3+) salts are also available (Ferric hydroxide polymaltose complex, Iron polysaccharide, etc.), but ferrous (Fe2+) salts are supposed to be better absorbed. A number of iron combinations (with vitamins, minerals, amino acids, etc.) are marketed, but should be considered irrational due to lower iron content. About 50–100 mg of iron can be incorporated into hemoglobin daily, and about 25% of oral iron can be absorbed. Full haemopoetic response in adults is usually achieved with administration of 200 mg elemental iron daily p.o. in 2 or 3 divided doses after or in between meals. Absorption of iron is much better when taken in empty stomach, but side effects may limit patient compliance. For prophylactic use, a daily dose of 30 mg elemental iron is sufficient. Parenteral iron preparations are indicated only in case of: severe deficiency with chronic bleeding; intolerance to oral iron; malabsorption or inflammatory bowel disease; erythropoietin therapy (to meet the increased needs of induced erythropoiesis). Parenteral forms contain organically complexed salts of unionized iron: Iron dextran, Iron sucrose complex, etc. (See Classification). A sensitivity test with a small test dose must be performed before parenteral administration of iron to avoid any risk of hypersensitivity reactions. In severe anemia, treatment with oral iron should be continued for at least 3 months after correction to replenish iron stores. Desferrioxamine (Deferoxamine), an iron chelator, is a specific antidote that is given systematically to remove iron. 2. Drugs for treatment of megaloblastic anemias Megaloblastic anemia is clinically manifested with a deficiency in serum hemoglobin and erythrocytes in which the erythrocytes are hyperchromic, fragile and abnormally large. It results from either folate or vitamin B12 deficiency. Pernicious anemia is a form of megaloblastic anemia resulting from reduced intestinal absorption of vitamin B12 (extrinsic factor) due to deficiency of intrinsic factor (a protein produced by parietal cells of the gastric mucosa). Parenteral injections of vitamin B12, but not oral preparations, are effective for treatment of pernicious anemia. Vitamin B12 3 Cyanocobalamin (vitamin B12 – amp. 250 mcg/1 ml i.m.). Cyanocobalamin and hydroxocobalamin are complex cobalt-containing compound present in diet and referred to as vitamin B12. Vitamin B12 is essential for cell growth and multiplication. Along with folic acid, it is involved in the DNA synthesis as a cofactor in the transfer of 1-carbon units. Two biochemical reactions require vitamin B12: conversion of methylmalonyl-coenzyme A (CoA) to succinyl-CoA and conversion of homocysteine to methionine. Methylcobalamin and deoxyadenosylcobalamin are the active forms of the vitamin. Conversion of homocysteine to H4 folate and methionine is conjugated with the conversion of cobalamin to methylcobalamin. Vitamin B12 deficiency results in deficiency of folate cofactors for DNA synthesis and megaloblastic anemia occurs first. This biochemical interaction explains why high doses of folic acid can improve the anemia, caused by insufficient supply of vitamin B12. Conversion of methylmalonyl-CoA to succinyl-CoA requires desoxycobalamin. Vitamin B12 deficiency results in accumulation of methylmalonyl-CoA, synthesis of abnormal fatty acids and neurologic defects, which may become irreversible if not treated promptly. The disruption of methionin synthesis is also supposed to be involved in the neuronal damage. Vitamin B12 deficiency is manifested by megaloblastic anaemia, glossitis, peripheral neuritis, paresthesias, poor memory, mood changes, hallucinations, etc. It is clinically used for treatment of megaloblastic anaemia, tobacco amblyopia, neuropathies and psychiatric disorders. Hydroxocobalamin is highly protein-bound and longer acting, but is associated with the development of antibodies (hence lesser in use). Folic acid Humans do not synthesize folic acid and meet theirs requirements from green leafy vegetables, fruit, mushrooms, liver, meat, kidney, eggs, milk and yeast. In the intestinal mucosa of jejunum folic acid is reduced by dihydrofolate reductase to tetrahydrofolic acid. Tetrahydrofolic acid through 1-C carbon transfer reactions is involved in the synthesis of purines and pyrimidines which are essential for DNA synthesis. Deficiency of folic acid leads to megaloblastic anaemia and teratogenic effects (spina bifida, etc.). Vitamin B9 prophylactically can be used during pregnancy and lactation – 0.4 mg p.o. daily) 3. Haematopoetic Growth Factors Erythropoetin: Epoetin alfa and Epoetin beta (Recormon). Erythropoietin stimulates erythrocyte proliferation and differentiation by acting on specific receptors present on red cell progenitors and promotes the release of reticulocytes. It is used to treat anemia in chronic renal failure or anemias secondary to cancer chemotherapy or HIV treatment, bone marrow transplantation, AIDS, cancer. Myeloid Growth Factors (Colony Stimulating Factors – CSFs). Granulocyte (G) and Granulocyte-Macrophages (GM) CSFs are cytokines. They accelerate the formation of matured leucocytes by acting on many progenitor cells. Filgrastim (recombinant G-CSF), Lenograstim (rG-CSF), Molgramostim (rGM-CSF) and Sargramostim (rGM-CSF) are used: to reduce the severity and duration of neutropenia induced by cytotoxic chemotherapy, radiotherapy or following bone marrow transplant; to treat congenital neutropenia, cyclic neutropenia and neutropenia associated with aplastic anaemia. Pegfilgrastim is a PEGilated (covalently conjugated to PolyEthylene Glycol polymer chain) form of filgrastim with a much longer t1/2 than the recombinant G-CSF. Megakaryocythe Growth Factors. Oprelvekin (IL-11) and Thrombopoietin stimulate the growth of megakaryocytic progenitors and increase the number of peripheral platelets. They are used to treat thrombocytopenia following cancer chemotherapy. 4 Table 1: Pharmacokinetic parameters Drug Iron preparations Ferrous sulfate Rout of application t1/2; Tmax; Cmax Methabolism Orally (20-30% absorption); sustained release tablets Bound to transferrin; endogenous system for storage and transport; elimination with cell loss (skin, hair, nails), in feces, perspiration, breast milk, blood loss, urine. About 5% excreted in urine in 24 hours t1/2=6 h Tmax is 2 h Mean Cmax is 203 mcg/dL t1/2 values do not represent clearance of iron from the body Iron sucrose intravenously complex Vitamin B12 and Folic acid Vitamin B12 orally, rapidly (Cyanocobalamin) absorbed; intranasally, intramuscularly; should not be administered i.v. t1/2=6 h, T max is 10 min, Cmax is 538 μmol/l Folic acid t1/2=24 (15-60) h Tmax is 1 h (oral) Cmax is 273. 3 ng/mL orally, rapidly absorbed; (rarely intravenously, subcutaneously, intramuscularly) t1/2=1.5-2 h Tmax is 1.25±1.9h (intranasal); 1 h (i.m.). Cmax is 757.96 pg/mL Hematopoietic growth factors Erythropoietin intravenously, t1/2=4-13 h (i.v.) to 24 h Alfa (Epoetin alfa) subcutaneously (s.c.) in chronic renal (1-3 times a week) failure Tmax is 12-18 h (s.c.) Cmax is 861 mIU/mL G-CSF Filgrastim intravenously, subcutaneously t1/2= 3.5 h Tmax is 2 (8) h Cmax is 49 (150) ng/mL Oprelvekin (IL-11) subcutaneously t1/2= 6.2 h Tmax is 3.2 h Bound to intrinsic factor during transit through the stomach; bound to transcobalamin for transport; main storage in the liver; secretion in the bile (3-8 mcg) and enterohepatic circulation; unbound vitamin is rapidly eliminated in the urine (50 to 98% within 48 h after i.m. injection). Intracellular demethylation of methyltetrahydrofolate to tetrahydrofolate (reaction requires vitamin B12); tetrahydrofolic acid is the active metabolite; methyltetrahydrofolic acid is the form for transport and storage; excreted mainly in the urine (traces in feces), breast milk. Metabolism is unknown, some degradation occurs; majority of excretion is found in feces with 10% unchanged in urine. It is not cleared by dialysis. Elimination route is not known. Level of circulating neutrophils may affect filgrastim clearance, with clearance increasing as neutrophil counts increase. Excreted through the kidney. 5 Cmax is 17.4 ng/mL Iron helators Desferrioxamine (Deferoxamine) intramuscularly, subcutaneously t1/2=6.4 min Tmax is 0.5 h Cmax is 8.7 µg/ml Liver, transamination, oxidation, beta-oxydation, decarboxylation and Nhydroxylation yielding neutral metabolites; excreted in the urine Side effects and toxicity Iron Iron salts can cause constipation, diarrhea (rarely), epigastric pain, heart burns, nausea, vomiting, metallic taste, and staining of teeth (mainly with oral liquid or chewable preparation). Local reactions: Pain at the site of action, skin pigmentation, sterile abscess. Systemic side effects: Fever, headache, joint pain, urticaria, lymphadenopathia; anaphylactoid reaction (palpitation, chest pain, dyspnoea, cardiovascular collapse) may occur with iron-sorbitol preparations, but rarely with other preparations). Acute iron toxicity occurs mostly in young children after accidental ingestion of iron tablets. Severe intoxication is clinically presented with necrotizing gastroenteritis, shock and metabolic acidosis. Coma and death may result. Unfortunately, activated charcoal, does not work here. Deferoxamine is used as a specific antidote. Chronic iron toxicity (hemochromatosis) occurs in persons with an inherited abnormality of iron absorption or with frequent transfusions (eg, thalassemia major). Iron chelators (deferoxamine or the oral agent deferasirox) are used in the treatment of chronic iron overload. Vitamin B12 and folic acid Both substancies are well tolerated and neither their form has significant toxicity. Hematopoietic growth factors Erythropoietin can provoke an increase in hematocrit, blood viscosity and peripheral vascular resistance. Hypertension, thrombotic complications and flu-like symptoms (rare) may occur. For prevention of CV complications, it is recommended to maintain hemoglobin levels < 12 g/dL. Myeloid Growth Factors: G-CSF is better tolerated than GM-CSF. It may cause fever, bone pain (10-15%), myalgia, and vasculitis. GM-CSF is more likely to provoke fever, arthralgia, myalgia and skin rash. Megakaryocythe Growth Factors IL-11 treatment is associated with dizziness, headache and fatigue. Recombinant human trombopoietin is supposed to be better tolerated. OUESTIONS1 1. All of the following drugs are used for iron deficiency anemia, except: A) Ferrous sulphate; B) Folic acid; C) Ferrous glutamate; D) Ferrous fumarate. 2. The recommended dose of elemental iron for oral supplementation is: A) 50 mg daily; B) 100 mg daily; C) 150 mg daily; D) 200 mg daily. 3. An adverse effect of oral iron therapy is: A) Anemia; B) Thrombocytopenia; C) Constipation; D) Headache. 1 Answers: 1B; 2D; 3C; 4B, C; 5D; 6D; 7C; 8A, B; 9A; 10A, C, D; 11C. 6 4. Iron preparations for parenteral use are: A) Ferrous aspartate; B) Iron dextran; C) Iron isomaltoside; D) Ferric hydroxide polymaltose complex. 5. Iron sucrose complex can be administered: A) Orally; B) Subcutaneously; C) Intramuscularly; D) Intravenously. 6. Which of the following is used for treatment of pernicious anemia? A) Erythropoetin B) Oral Vitamin B12; C) Iron; D) Parenteral Vitamin B12. 7. Which of the following statements about Folic acid is correct? A) It is used for treatment of trombocytopenia; B) It is contraindicated in pregnancy; C) It is used for treatment of megaloblastic anemias; D) Its clinical use is limited by serious side effects. 8. Select the correct statements about Desferrioxamine: A) It is specific antidote in acute iron overdose; B) It is an iron chelator; C) It is a drug of choice for treatment of iron deficiency; D) Both B and C are correct. 9. Erythropetin is used for: A) Treatment of anemia associated with chronic renal failure; B) Treatment of neutropenia associated with radiotherapy; C) Treatment of thrombocytopenia associated with cancer chemotherapy; D) Prevention of congenital neural tube defects. 10. Which of the following drugs influence leucopoiesis? A) Filgrastim; B) Erythropoetin; C) Doxorubicin; D) Sargramostim. 11. This drug is used for treatment of thrombocytopenia following cancer chemotherapy: A) Vitamin B12; B) Filgrastim; C) Oprelvekin; D) Molgramostim. Conclusions: Hemopoiesis is regulated by balanced interaction between endogenously derived hematopoietic growth factors and exogenously supplied essential nutrients (hematinics). Hematopoietic growth factors in clinical use are: Erythropoietins (Epoetin alfa, Epoetin beta); GCSF (Filgrastim, Lenograstim), GM-CSF (Sargramostim, Molgramostim); Oprelvekin (IL 11) and Trombopoietin. Hematinics in clinical use are: Iron salts, Vitamin B12 and Folic acid. Treatment or prevention of iron deficiency anemia is the only clinical indication for the use of iron preparations. The main therapeutic preparation is Ferrous sulfate. Vitamin B12 and Folic acid are used for the treatment of megaloblastic anemias. Parenteral Vitamin B12 is required for treatment of pernicious anemia. Erythropoietin stimulates the production of erythrocytes and increases their release from the bone marrow. It is used to treat anemia in chronic renal failure and anemias secondary to inflammation, cancer or cytotoxic therapy. Myeloid Growth Factors are used to treat neutropenia after myelosuppressive therapy. Oprelvekin (IL-11) and Thrombopoietin are used to treat thrombocytopenia following cancer chemotherapy. Recommended References: Katzung B et al (2009) Basic & Clinical Pharmacology. Katzung B and A Trevor (2010) Pharmacology Examination and Board Review. Tripathi KD (2008) Essentials of Medical Pharmacology. Sharma HL et al (2007) Principles of Pharmacology. Rang H et al (2011) Pharmacology. Clark S (2009) Current Opinion in Gastroenterology 25: 122–128. Novak J et al (2008) Curr Opin Nephrol Hypertens 17 (6):580-8. Castro R et al (2010) California Journal of Health-System Pharmacy March/April: 5-14. Testa U (2010) Expert Opin. Emerging Drugs 15(1):119-138. Pasricha S-R et al (2010) MJA 193: 525–532. Zhu A et al (2010) Dig Dis Sci (2010) 55:548– 559. McKoy J et al (2008) Transfusion 48(8):1754-1762. Locatelli F et al (2012) Expert Opin. Pharmacother. 13(4):495-503. Gejsler B (2010) Expert Opin. Biol. Ther. 10(8): 1209-1216. Foote MA et al (2002) Cytokines, Cellular & Molecular Therapy 7: 49-59. Kuter D (2007) Blood 109: 4607-4616. McCune J et al (2012) Pharmacotherapy 32(1):7-19. Montero A (2006) Leuk Lymphoma 47(10):2049-54. Imbach P et al (2011) N Engl J Med 365:734-741. 7 8