Arnolds Kadišs. The complex study of new small diameter composite
advertisement

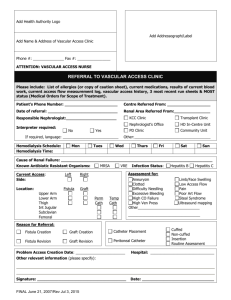
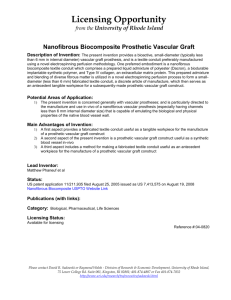
RIGA STRADINS UNIVERSITY LATVIA Arnolds Kadišs THE COMPLEX STUDY OF NEW SMALL DIAMETER COMPOSITE VASCULAR GRAFT AND EVALUATION OF ITS PRACTICAL USE Specialties - medical biomechanics, surgery Summary of doctoral thesis Riga, 2005 INTRODUCTION The fabrication and design of synthetic vascular grafts has been a challenging area in vascular surgical research during the past 30 years. Large diameter grafts (more than 5 mm) used for replacing arteries in high flow regions such as aorta have generally performed well. Despite, the replacement of small diameter arteries (5 mm and less) with synthetic grafts has not yet been successful and continues to be a problem in vascular surgery. The small-diameter synthetic vascular grafts that are presently implanted have shown poor patancy rates due to the development of anastomotic intimal hyperplasia (IH) and thrombus formation. It has been established that progression of the lesion involves migration and proliferation of smooth muscle cells (SMC) as well as the production of increased cellular matrix. This process involves a complex set of interaction between SMC, endothelial cells (ES) and number of growth factors and cytokines deriving from a disruption in the balance between inhibitory and stimulating factors. In additional to biomechanical incompatibility, physical forces have been associated with vascular graft IH. Prominent among these suggestions have been compliance mismatch between the graft and host artery, which results is different mechanical strain and various haemodynamic wall shear stress parameters. Mechanical characteristics of vascular grafts, such as size, compliance and modulus of elasticity, have significant potential to influence their long-term patency. Circumferential compliance mismatch has an important role in graft failure. It has been demonstrated that the compliance of biological conduit is significantly greater then those of current non-compliant (rigid) prosthetic graft materials. Also a longitudinal strain plays a very important role in maintaining SMC differentiation into contractile phenotype and for increasing of the production rate of an extracellular matrix. Tissue engineering is up-to-day approach of applying the principles and methods of engineering and biology in order to develop functional tissue for surgical replacement. First attempts to create vascular tissue engineered blood vessels resulted in the manufacturing of grafts with poor mechanical properties. In order to prevent anastomotic intimal thickening the ideal scaffolds for tissue engineered small diameter vascular grafts must mimic the biomechanical properties of natural arteries and have to be compliant. Employing principles of biomimetics or imitation of biomechanical properties and organization of fibro-elastic structure of natural blood vessel is one of most promising way to achieve this goal. Lack of vascular grafts for replacement of small diameter arteries and lack of ideal scaffold for tissue engineering is a cause why we should investigate every new small diameter composite vascular graft. AIM OF THE STUDY To investigate complex properties of small diameter composite vascular graft and to evaluate its possibility to use in practice and in tissue engineering. OBJECTIVES 1. To determine biomechanical properties of small diameter composite vascular graft and common iliac artery of dog in vitro; 2. to implant small diameter composite vascular graft into experimental animals dogs and to extirpate vascular graft after definite time (1,3 and 6 months); 3. to carry out biomechanical investigation of small diameter composite vascular graft after extirpation of experimental animals; 4. to perform morphological studies of small diameter composite vascular graft after extirpation of experimental animals; 5. to evaluate possibility to use small diameter composite vascular graft as a scaffold tissue engineered blood vessel. CONTRIBUTION AND IMPACT Atherosclerosis is one of the most important problems in our population. It affects all kind of arteries and causes stenosis and occlusion of arteries. As a result millions of people in whole world die every year. To cure stenosis or thrombosis caused by atherosclerosis substitutes of blood vessels are necessary. They can be artificial substitutes as well as native vessels of the patient himself. However, efforts to develop vascular grafts of small diameter with potential for long term patency have not yet met with success. Up to now there is not an evidence of many complete studies where biomechanical properties of small diameter vascular grafts were investigated in vitro. Information exists in the literature about only solitary researches of vascular grafts in vivo in animals, but complex study of small diameter composite material textile vascular graft has not been done yet. Therefore this study focuses on the complex study of new composite material vascular graft. We have determinated water permeability, toxicity and biomechanical properties of composite material vascular graft and according to the date achieved it can be concluded that biomechanical properties of vascular grafts are similar with those of a native vessel. Good early postoperative results are achieved and the ideas developed could provide a good basis for further development of new type of small diameter vascular grafts. For the first time in the research of tissue engineering the even distribution of seeded cells alongside the thickness of the wall of the composite material vascular graft is achieved. Applying new cell seeding technique - centrifugal casting procedure provides high density of redistributed cells in the prosthesis. For the first time the experiment has shown that composite small diameter vascular graft is a perspective scaffold for creation of new type blood vessels in tissue engineering. The blood vessel substitutes developed on the new scaffold would give new opportunities in modern medicine including cardiac and vascular surgery which would radically improve the results of treatment and would save lives of millions of people suffering from atherosclerosis. STRUCTURE OF THE WORK Research work has been written in Latvian. It consists of 9 chapters (actuality, literature review, arm and objectives, contribution and impact, material and methods, results, discussion, conclusions and list with references consisting of 332 titles). Total volume of the research work covers 125 pages including 4 tables and 38 figures. LIST OF SCIENTIFIC PUBLICATIONS 1) Kadish A., Ozols AI, Ozolanta I., Ozols A., Kancevich V., Purinyia B., Feldmane L., Kasyanov V. Maza diametra asinsvada protēze ar garendeformatīvām un šķērsdeformatīvām īpašībām. Scientific Proceedings of Riga Stradins University. Riga. 2001: 66-69. 2) Kasjanovs V., Ozolanta I., Kadiss A., Ozols Al., Stradins P. Feature of biomechanical behaviour and structure of the arterial wall as a compliant biocomposite material. Scientific Proceeding of Riga Technical University. 2001; 2: 15-26. 3) Kadišs A., Ozolanta L, Kasjanovs V. Maza diametra kompozīta asinsvada protēzes biomehānisko īpašību vērtējums in vitro un eksperimentā ar dzīvniekiem. Acta Chirurgica Latviensis. 2004: 71-76. 4) Kadišs A., Ozolanta I., Puriņa B., Feldmane L., Murovska M, Kasjanovs V. Jauna tipa maza diametra kompozīta materiāla asinsvada protēzes kompleksie pētījumi. Scientific Proceedings of Riga Stradins University. 2004: 314-322. 5) Mironov V., Kasyanov V., Yost M., Visconti R., Twal W., Trusk T., Wen X., Ozolanta I., Kadishs A., Prestwich G., Terracio L., Markwald R. Cardiovascular Tissue Engineering I. Perfusion Bioreactors: A Review. J Long-Term Effects of Medical Implants. 2005 (in press). 6) Ozolanta 1., Kancevich V., Purinya B., Kadiss A., Kasyanov V. Mechanical and structural investigation of new compliant textile grafts. European Medical and Biological Engineering Conference. Vienna, Austria, 4-7 November. 1999: 302303. 7) Kasyanov V., Ozolanta 1., Ozols A., Kancevich V., Purinya B., Kadish A., Ozols Al., Mironov V. Longitudinally and circumferentially compliant composite vascular graft. Proceedings of the 12 Conference of the European Society of Biomechanics. 27th - 30th August 2000, Dublin, Ireland. 2000: 257. 8) Ozolanta I., Kadiss A., Purinya B., Feldmane L., Murovska M., Kancevich V., Kasyanov V. Biomechanical and morphological peculiarity of small diameter composite compliant vascular graft. Proceedings of 2. European Medical and Biological Engineering Conference, Part II. December 04-08, 2002, Vienna, Austria. 2002: 1032-1033. 9) Kadišs A. Kompozīta materiāla asinsvadu protēzes eksperimentāla aprobācija uz dzīvniekiem. Conference of AML Scientific Association of Students. Riga. 1999: 14. Abstract. 10)Kadish A., Ozols A., Ozolanta I., Ozols A., Kancevich V., Purinya B., Feldmane L., Kasyanov V.. Longitudinally and circumferentially compliant composite vascular graft. Scientific conference of Riga Stradins University. Riga. 2000: 15. Abstract. ll)Ozolanta I., Pūriņa B., Kasjanovs V., Kadišs A., Stradiņš P.. Bioloģiskie un mākslīgie konduīti, to piemērotība lietošanai sirds ķirurģijā. The 4* Congress of World Latvian Physicians. Riga. 2001: 130. Ahstract. 12) Kadišs A., Ozolanta I., Purina B., Feldmane L., Murovska M., Kasjanovs V. Jauna tipa maza diametra asinsvada protēzes biomehānisko un morfoloģisko īpašību analīze. Scientific conference of Riga Stradins University. Riga. 2003: 128. Abstract. 13)Kasyanov V., Ozolanta I., Kadiss A., Goswamy B., Markwald R., Mironov V. Rational biomimetic design of hybrid composite vascular scaffold. 8th Annual Hilton Head Workshop "Cardiovascular tissue Engineering: From basic biology to cell-based therapies". March 6-10, 2004, Sea Pines Plantation Hilton Head, SC, USA. 2004: 77. Abstract. 14)Kasyanov V., Ozolanta I., Kadiss A., Goswamy B., Markwald R., Mironov V. Vascular scaffold biomimetic design. In: Conference Proceeding „Medical Textile 2004. Advances in Biomedical Textiles and Healthcare Products". October 26 27, 2004, Pittsburgh. 2004: 102. Abstract. 15) Kadišs A., Kasjanovs V., Ozolanta I. Maza diametra kompozīta materiāla asinsvada protēze kā karkass audu inženierijā. The 3rd Congress of Latvian Surgeons. Riga. 2005: 39. Abstract. REPORTS ON THE STUDY SUBJECT 1. Kadiss A. Kompozita materiala asinsvadu protezes eksperimentala aprobācija uz dzīvniekiem Conference of AML Scientific Association of Students. Riga, Latvia. 1999. 2. Ozolanta I., Kancevich V., Purinya B., Kadiss A., Kasyanov V. Mechanical and structural investigation of new compliant textile grafts. European Medical and Biological Engineering Conference. Vienna, Austria. 1999. 3. Kasyanov V., Ozolanta I., Ozols A., Kancevich V., Purinya B., Kadish A., Ozols AL, Mironov V. Longitudinally and circumferentially compliant composite vascular graft. 12th Conference of the European Society of Biomechanics. Dublin, Ireland. 2000. 4. Ozolanta I., Pūriņa B., Kasjanovs V., Kadišs A., Stradiņš P.. Bioloģiskie un mākslīgie konduīti, to piemērotība lietošanai sirds ķirurģijā. The 4 th Congress of World Latvian Physicians. Riga, Latvia. 2001. 5. Kadish A., Ozols Al., Ozolanta I., Ozols A., Kancevich V., Purinyia B., Feldmane L., Kasyanov V. Maza diametra asinsvada protēze ar garendeformatīvām un šķērsdeformatīvām īpašībām. Scientific Conference of Riga Stradins University. Riga, Latvia. 2001. 6. Ozolanta L, Kadiss A., Purinya B., Feldmane L., Murovska M., Kancevich V., Kasyanov V. Biomechanical and morphological peculiarity of small diameter composite compliant vascular graft. European Medical and Biological Engineering Conference, Part II. Vienna, Austria. 2002. 7. Kadišs A., Ozolanta L, Puriņa B., Feldmane L., Murovska M., Kasjanovs V. Jauna tipa maza diametra asinsvada protēzes biomehānisko un morfoloģisko īpašību analīze. Latvia. 2003. Scientific Conference of Riga Stradins University. Riga, 8. Kadišs A., Ozolanta I., Pūriņa B., Feldmane L., Murovska M, Kasjanovs V. Jauna tipa maza diametra kompozīta materiāla asinsvada protēzes kompleksie pētījumi. Scientific Conference of Riga Stradins University. Riga, Latvia. 2004. 9. Kasyanov V., Ozolanta I., Kadiss A., Goswamy B., Markwald R., Mironov V. Rational biomimetic design of hybrid composite vascular scaffold. 8th Annual Hilton Head Workshop "Cardiovascular tissue Engineering: From basic biology to cell-based therapies". Sea Pines Plantation Hilton Head, SC, USA. 2004. 10.Kasyanov V., Ozolanta I., Kadiss A., Goswamy B., Markwald R., Mironov V. Vascular scaffold biomimetic design. Conference „Medical Textile 2004. Advances in Biomedical Textiles and Healthcare Products". Pittsburgh, USA 2004. ll.Kadišs A., Kasjanovs V., Ozolanta I. Maza diametra kompozīta materiāla asinsvada protēze kā karkass audu inženierijā. The 3rd Congress of Latvian Surgeons. Riga, Latvia. 2005. MATERIAL AND METHODS The most part of study has been done in Latvia at Riga Stradins University, Agriculture University of Latvia, Riga Technical University and University of Latvia. The tissue engineering stage has been done in the USA at Medical University of South Carolina. Veterinary department of Ministry of Agriculture of Latvia has approved the study. The performances of textile compliant composite vascular grafts (CVG) designed and constructed in this work were evaluated. In manufacturing the former, textile threads with two widely different deformative characteristics, one nearly matching those of the elastin and the other of the collagen fibers, were selected. The materials used were a polyurethane monofilament yarn (Volgograd Chemical Thread Plant, Volgograd. Russia) with a low modulus of elasticity (0.8 MPa) and a bulked polyester multifilament yarn (Mogilev Chemical Thread Plant, Mogilev, Russia) with a high modulus of elasticity (1.4 x 102 MPa). Tubular grafts of diameters 4 mm were made by a weaving process utilizing a foil ribbon loom and shown in the figure below. Small diameter composite vascular graft. Experiments were conducted to evaluate the mechanical properties of novel composite small diameter vascular grafts and a dog's iliac artery at different levels of the internal pressure. Mongrel dogs weighting approximately 25 kg were used. A total of five dog's iliac arteries obtained from autopsy were used. During experiments arterial and graft cylindrical segments were gradually loaded by increasing the internal pressure from 0 up to 200 mm Hg. For determining vascular graft water permeability, the procedure of Guidoin et al. was used. Then composite vascular graft was tested for toxicity. Afterwards 28 vascular grafts were implanted into dogs. A total of 14 mongrel dogs weighting approximately 25 kg were used. Grafts were implanted for one, three and 6 months. Both iliac arteries were used. After extirpation biomechanical properties of vascular grafts were evaluated. The distal and proximal ends of extirpated vascular grafts were routinely prepared for light microscopy. Biological compatibility was investigated by using various cell cultures and cell lines. Presence of blood-borne viruses in the cells infiltrating vascular graft was detected by RT test, PCR and nested PCR in vitro systems as well as in vascular graft 6 months post implantation. Finally, composite vascular graft was used as a scaffold for tissue engineering blood vessel development. There was used centrifugal casting procedure for cell seeding, histology and microscopic analysis, morphometric analysis and statistics. Before centrifugal casting procedure, the volume of hydrogel for the first hydrogel layer was calculated on the basis of given thickness of the layer (1mm) and length of the tube (less the length of stoppers in the tube). This volume of the hydrogel was placed in the tube. The tube was tightly closed with silicon stoppers and then fixed in the spinner. The tube was spun with a speed of 2000 rpm for 10 min, during which time the hydrogel crosslinked. The next required volume of hydrogel and cells was calculated starting from the thickness of the second layer. The viscous cell suspension was placed into the tube and spun for additional 10 min. After crosslinking of the second layer, the scaffold was removed from the tube and placed either in 4% paraformaldehyde or in media Ml99 with 10% fetal bovine serum RESULTS Hydraulic permeability for composite vascular graft without impregnation was 2,48 ± 0,68 l/min cm2. It was much more than expected and was not acceptable. After covering vascular graft with a coating of cross - linked gelatin by a vacuum impregnation method water permeability was lowered to 0,15 ± 0,03 l/min cm2. Composite vascular graft was inspected for toxicity with test organisms Tetrachymena pyriformis and Dqfnia magna Straus and with different cell cultures. Vascular graft was found not to be toxic for living organism. A total of 14 mongrel dogs weighting approximately 25 kg were used for graft implantation. Together 28 implantations were done. After implantation four grafts failed due to inflammation and were excluded from the study. Eight vascular grafts were extirpated after one month, eight - after three months and eight grafts were extirpated after six months. Vascular prostheses, extirpated after one and three months, had smooth inner surfaces. Two grafts, extirpated after six months, had stenosed lumen (more than 50 %), but two vascular grafts were trombosed. At first, biomechanical research of composite vascular graft was made before implantation to experimental animals. Results displayed in curves that allow analyzing results more easily. Experimental results in vitro showed that composite vascular grafts had deformation up to 15 % in the circumferential direction at internal pressure 120 mmHg, and maximum longitudinal deformation up to 30%. When vascular graft is coated with gelatin, it increases compliance in the circumferential direction that shown in figure below. Pressure - circumferential stretch ratio relationship for the composite vascular grafts. Infuence of gelatin to circumferential stretch ratio. This phenomenon can be explained by decrease of friction among the yarns of vascular graft. The increase of the longitudinal stretch ratio of the vascular graft leads to the increase of the compliance in the circumferential direction that shown in the figure below. Pressure - circumferential stretch ratio relationship for the composite vascular grafts at the different longitudinal stretch ratio. These results should be taken into account, when operations are made. Vascular graft should be sutured in longitudinal stretch to increase circumferential stretch ratio. Here it is necessary to admit that arteries also are in natural longitudinal stretch in the body. Experimental results of the study was compared with Hayashi data from literature and shown in the figure below. Hayashi summarized stiffness parameters β of different arteries and vascular grafts. From compared data we could see that stiffness parameter β of commercial vascular graft (CVG) and Gore - Tex vascular graft (GT) was almost identical. Stiffness parameter β of composite vascular graft (CGV) was similar to stiffness parameter p of common carotid artery (CCA) and little Hayashe data of stiffness parameter for different arteries and vascular prostheses compared with small diameter composite vascular graft. GT - Gore - Tex thin walled ePTFE vascular graft; CW - Cooley low porosity woven Dacron graft; CVCooley double velour knitted Dacron graft; DB - Dardik Biografi; KP Polyurethane grafts; CCA - human common carotid artery, FA - human femoral artery; CoA - human coronary artery; CVG - commercial vascular graft; DCIA dog common iliac artery; C.GV - composite vascular graft. bit higher than stiffness parameter p of dog common iliac artery (DCIA). Stiffness parameter (3 of composite vascular graft (CGV) is less than stiffness parameter p of polyurethane prostheses (PP) displayed in Hayashi data. From above it could be concluded that circumferential stretch ratio of composite vascular graft is less than identical ratio of native vessels, but much more than circumferential stretch ratio of Gore - Tex, polyurethane and other vascular grafts. Biomechanical properties of composite material vascular graft were analyzed after extirpation from dogs (after 1, 3 and 6 months). Curves in the figure below show relationship between pressure and circumferential stretch ratio. It is obvious, that Internal pressure - circumferential stretch ratio relationship for small diameter composite vascular graft and relationship dependency on time of implantation (before implantation, after 1 month, after 3 months and after 6 months after extirpation). deformities of the vascular grafts wall decreased due to ingrowths of the tissue. Circumferential stretch ratio of composite vascular graft was similar to circumferential stretch ratio of connective tissue after 6 months of implantation. The structure of vascular grafts was examined with light microscopy after extirpation of experimental animals. Cross examination of extirpated grafts after one month revealed an inner surface lined with a smooth, thin layer of glistening tissue, which was found to make a single layer of endothelial - like cells overlying several layers of myofibroblastic cells. Cross examination of grafts after three months of functioning showed neointima on inner surface and capsule of connective tissue on outer surface as showed in figure below. Small histiocytic cells and fibers were found in between structure of vascular graft. Light microscopy - small diameter composite vascular graft after 3 months of implantation. (Hematoxilin and eosin), x50. Smouth intima covers internal side of vascular graft. EC - external capsule, P - vascular graft, IC - internal capsule. The inner surfaces of vascular graft after 6 month was covered with thicken neointima, in some specimens reduction of lumen was observed and shown in figure below. Light microscopy - small diameter composite vascular graft after 6 months of implantation. (Hematoxilin and eosin), x50. Thicken neointima covers inner surface of vascular graft. TNI-thicken neointima, P-vascular graft, Al- iliac artery. To exclude adjacent factors influencing vascular grafts In vivo, specimens were studied to presents of blood-borne viruses in the cells infiltrating vascular graft. In vivo studies neither the presence of canine herpesvirus nor retroviruses was found in the vascular graft infiltrating cells. Cytometric analysis of vascular graft was made after extirpation of experimental dogs. Found that 1 mm2 of vascular graft was infiltrated with 7500 cells. Then native vessel was analyzed for cell containing, 6000 cells was isolated from 1 mm2 of native vessel. Finally, composite vascular graft was used as scaffold in tissue engineering. In order to estimate effect of centrifugal forces on cell survival (vs. cell damage), there were used green fluorescent protein (GFP)-labeled quail QCE-6 cells. Mixing of GFPlabeled QCE cells with the ungelled synthetic extracellular matrix (sECM) induces limited cell damage, as observed by a small number of non-fluorescent cells. Living, fluorescent QCE cells in hydrogel incubated for 10 min without centrifugation and living fluorescent QCE-6 cells in the sECM experiencing 10 min centrifugation at 2000 rpm were similar in appearance and numbers. Quantitative cytometry of dead (green negative) QCE cells in control (10 min incubation in sECM without centrifugation) and in experiments (10 min centrifugation in sECM) demonstrated the absence of statistically significant effect (p>0,05) of centrifugal forces of cell damage, shown in the figure below. Quantitative cytometry of dead QCE cells. 1 - QCE cells in control group 10 min incubation without centrifugation, 2 - QCE cells in experimental group 10 min incubation with centrifugation. Centrifugal casting allowed the redistribution of cells into the form of tubular construct with a circular cross-sectional cell layer. This layer consisted of densely packed cells. The fluorescence of the labeled cells indicated that most of cells in this layer were viable and undamaged. The packing density is very high as shown both on frozen and histological sections. Morphometric stereological estimation of surface cell density based on histological sections demonstrated that packing volume density (65.6%) approaches the packing density calculated as average theoretically maximally possible packing density (62.3 %). Moreover, the experimentally obtained density is very close to volume density of natural myocardium in adult animal (75%). In order to estimate suitability of centrifugal casting technology for placing of cells on tissue engineered scaffolds for vascular tissue engineering, a wetted woven hybrid vascular graft was employed. In the first experiment two steps centrifugal casting procedure was employed. Fluorescent microscopy demonstrated a high density of redistributed cells on the luminal surface of vascular construct. Strong fluorescence indicates that virtually all cells survived the centrifugal casting procedure. The fabricated tissue engineered construct contained HA-based sECM hydrogel and circular layer consisted of several rows densely packed living cells. In another experiment designed to place a cellularized sECM into wetted woven composite vascular graft, a one-step centrifugal casting method was used. This technique produced a remarkably homogeneous redistribution of fluorescent cells throughout whole wall thickness of vascular graft as shown in the figure below. Fluorescent microscopy of composite vascular graft after one step centrifugal casting procedure. A. high density of redistributed cells on the luminal surface of vascular graft. Thus in future, centrifugal casting technique in combination with the in situ cross-likable sECM could be used to rapidly (10 min) fabricate a bioreactor-free. cellularized composite hybrid compliant biodegradable vascular graft. In principle, such a construct would be and "off-the-shelf" tissue engineered vascular graft for in vivo implantation. DISCUSSION The problem of the small diameter vascular substitutes has been crucial all over the world. In comparison with the large diameter vessel substitutes, mostly vascular grafts, where efficiency of graft is highly justified in the clinical practice (Szilagyi et al., 1986, Kakisis et al., 2005) the small diameter vascular grafts get trombosed in a considerably short period of time. (Akiyama et al., 1997, Steinthorsson, Sumpio, 1999) due to neointimal hyperplasia (Callow, 1988, Cassel et al., 1989, Xue, Greisler, 2003) and long-term solution hasn't been achieved yet. In order to increase patency of the small diameter vascular graft, prosthesis must have both longitudinal and circumferential stretch or according to its biomechanical properties it should be similar with a native vessel (Hsu, Kambic, 1997, Salacinski et., al 2001). However, it is concluded that small diameter synthetic vascular grafts applied before have low patency rates (David et al., 1999, Kakisis et al., 2005) and they get trombosed due to neointimal hyperplasia. Latvia has taken out a patient on a new small diameter composite vascular graft (Kancevich, Kasyanov, 1997, Kasyanov et al., 1999). The new type of vascular graft is unique and has no equal in the world yet. Topicality of the problem and the original properties of the graft make all inclusive research into the graft properties very significant. In the literature there are reports describing experiments in vitro, however systematic research and experiments in vivo have not been conducted yet. The research was carried out in three stages: experiments in vitro, experiments in vivo and working with tissue engineering. Experiments in vitro showed that the wall of prosthesis has up to 30% of longitudinal stretch and up to 15% circumferential stretch. In comparison with the present grafts the biomechanical properties of composite material prosthesis were considerably similar to the biomechanical properties of a native vessel. Regardless of the fact, that the stretch ratio of composite vascular graft was lower than the stretch ratio of a native blood vessel the character of analysed stretch curves was similar. To analyse the toxic influence on living organism, compatibility of two primary tripsinised reseeding cell cultures were examined: embryonic lamb fibroblasts and thymus cells. Likewise no difference was diagnosed in density of cell growth in the culture with prosthesis and the control culture. It can be concluded that prosthesis has no toxic influence on living organism. The scientific literature doesn't hold many reports on researches in vitro into the small diameter composite material vascular prosthesis (Kambic, 1988, Hayashe et al., 1989, Bos et al. 1998), Nevertheless there are few researches in vivo done. However, researches into the small diameter textile vascular grafts based on original weaving technique in vivo have not been found. As the complex studies on the woven small diameter composite material vascular graft patented in Latvia have not been conducted yet it was considered to start a research both in vitro and in vivo. The results of the research in vitro were a success and the research in vivo on animals was immediately started. Initially the results were good, one and three months later smooth neointima was found on the inner surface with no signs of rejection of tissues. Circumferential stretch ratio decreased due to ingrowths of connective issues into the wall of prosthesis. Nevertheless, circumferential stretch ratio maintained between 7 -12%. Six months later neointimal hyperplasia was detected in about 50% of all prosthesis. The research showed good results and they can be compared with the research data on the small diameter vascular grafts carried out in other countries (Hayashi et al., 1989, Greisler et al., 1992, Pasic et al., 1996, Davids et al., 1999, Xue, Greisler, 2003). There are scientists who suggest to use interrupted sutures for anastomoses (Schajer et al., 1996) to avoid paraanastomotic increased compliance zone with neointimal hyperplasia, which is caused when using continuous sutures. Furthermore interrupted sutures didn't cause significant change in a pulse wave. (Tiwari et al., 2003). It must be admitted that despite these important reports on the significance of interrupted sutures the method didn't receive much recognition and in the daily practice continuous sutures are used for small diameter vascular anastomoses. In order to make our study comparable with the studies done in the other countries continuous sutures were applied in the study. Although suture technique could affect the results, its effects were not analyzed in the study. To develop long-terms results scientists in 2000 started to focus on tissue engineering (L'Heureux et al., 1998, Niklason et al., 1999, Schmidt, Baier, 2000, Watanabe et al, 2001, Rabkin, Schoen, 2002, Xue, Greisler, 2003, Kakisis et al, 2005). One of the biggest problems in tissue engineering is the lack of appropriate scaffold with highly porous structure that could be used as a basis for synthesizing a native vessel (Hoesrstrup et al., 2001) thus ensuring a proper cell penetration along the wall of the scaffold (Rabkin, Schoen, 2002). To sum up the results gained in the research both in vitro and in vivo it can be concluded that the properties of composite vascular grafts almost correspond to the properties of an ideal scaffold. It led to the third stage - tissue engineering study. Cell casting on the small diameter vascular graft provides even distribution of seeded cells alongside the thickness of the wall of the graft. Cells remain viable which can be observed using fluorescent microscopy. Also high cell density was achieved in the prosthesis (65,6%) in comparison with a native animal myocardium (75%) (Olivetti et al., 1980). What marks difference is that the data gained from our study are considerably better than those given by literature (Yang et al., 2001, Dar et al., 2002, Godbey et al., 2004) in terms of cell density and distribution of cells in the prosthesis which were achieved due to the properties of composite material vascular graft structure. The results gained in the tissue engineering prove the assumption made before that composite material graft can be an ideal scaffold for creation of a new type blood vessel in tissue engineering. To take it further, centrifugal casting method in combination with composite material graft woven in diameter of different size could also serve as a basis for synthesizing of other crucial hollow organs like esophagus, trachea, intestines, urinary bladder, uretheris etc. (Atala, 2003, Grikscheit et al., 2003, Macchiarini et al., 2004, Chen, Beierle, 2004, Corvin et al., 2004, Zini et al., 2004, Beckstead et al., 28005, Grillo, 2005, Omori et al., 2005). CONCLUSSIONS 1. The research methods applied in the study on the change of biomechanical and structural properties of small diameter composite material in vitro and in vivo allow gaining objective data and estimating the possibilities of practical use of vascular grafts. 2. Composite small diameter vascular graft in vitro has longitudinal and circumferential stretch, which makes the prosthesis correspond to a native blood vessel according to its properties. The stiffness parameter of composite vascular graft is slightly higher than of those of a native blood vessel, however they are much lower than the stiffness parameter of commercial grafts GoreTex, woven and polyurethane prosthesis. 3. By increasing the longitudinal stretch ratio of composite material vascular graft also circumferential stretch ratio increases which is particularly important during the reconstructive operations to have good postoperative results. In the process of implantation vascular graft should be pre-stretched in longitudinal direction. 4. The examination of composite material vascular graft has not revealed toxic influence on living organisms. Tissue ingrowth in prosthesis is identified as normal with no chronic inflammation or rejection. In experiments with animals morphological changes in the wall of prosthesis is not affected by the side factors like viruses that are spread through blood. 5. With the increasing of time of residence of the composite vascular graft in an animal, the circumferential stretch ratio of vascular graft decrease due to ingrowths of connective tissues to the wall. Nevertheless the research shows good data, which are comparable with the studies conducted in other countries of the world on small diameter vascular grafts. 6. Cell density or number of cells into the graft wall after six months is higher for 25% than the number of cells into a wall of a normal blood vessel. It can be explained by neointimal hyperplasia and connective tissue capsule formation. 7. Considering possible structural modification of a vascular graft and corresponding improvement of its physical and biomechanical properties as well as the use of new materials and coverings makes the future of a small diameter composite material vascular prosthesis perspective. 8. Using of the composite vascular graft for cell seeding and introduction of the new cell seeding technique (centrifugal casting technology) has provided high cell density and uniform distribution of seeded cells alongside the thickness of the wall of the composite vascular graft. It suggests that the graft may be recommended as a perspective scaffold for creation of novel tissue engineered blood vessel.