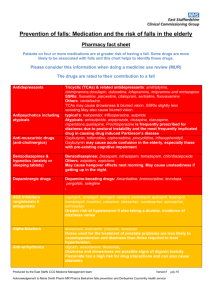
Appendix 11 – Medication that may increase the risk of falls
advertisement

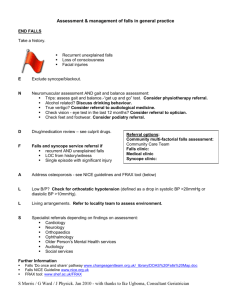
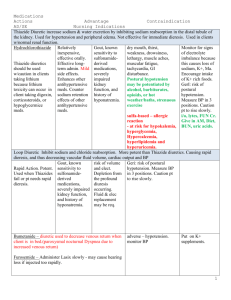
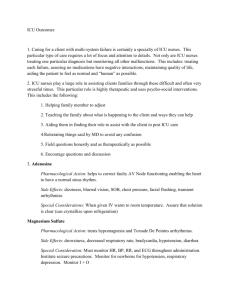
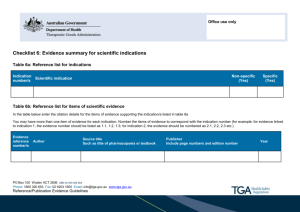
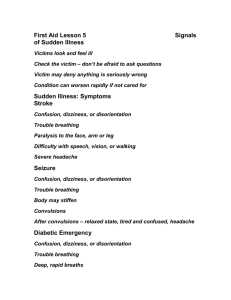
Appendix 11 Medication which may increase the risk of falls Note this is not an exhaustive list and any further advice and updates should be sought from pharmacists and medical colleagues CLASS/ TYPE Antidepressants EXAMPLES TriCyclic Antidepressants (TCA) e.g.Amitriptylline, Dosulepin (Dothiepin), Imipramine, Lofepramine. POSSIBLE SIDE EFFECTS Drowsiness, blurred vision, dizziness, postural hypotension, constipation, retention of urine. SSRIs e.g. Citalopram, Fluoxetine. Others Trazodone, Mirtazepine, Venlafaxine. Antipsychotic Antiemetics Sedatives and Hypnotics Medication for Parkinson’s Disease Medication with Anticholinergic Side-effects Chlorpromazine, Haloperidol, Lithium, Promazine, Trifluoperazine, Quetiapine, Olanzapine, Risperidone. Prochlorperazine, Cyclizine, Metoclopramide Temazepam, Diazepam, Lorazepam, Nitrazepam, Zopiclone, Chlordiazepoxide, Chloral Betaine, Clomethiazole Cobeneldopa, Cocareldopa, Rotigotine, Ropinirole, Pramipexole, Amantadine, Entacapone, Selegiline, Rivastigmine. (Benzhexol), Prochlorperazine, Oxybutynin, Tolterodine. Postural hypotension, confusion, drowsiness. Parkinsonian symptoms Postural hypotension, Confusion, drowsiness. Parkinsonian symptoms SUGGESTED ACTIONS Review appropriateness with prescriber/ GP. Stop if not required, may need to withdraw slowly. Consider changing a Tricyclic (TCA) to a Serotonin Specific Reuptake Inhibitor (SSRI) Consider specialist referral if further advice needed Review appropriateness and check if prescribed in line with relevant protocols. In long term use do not stop without specialist opinion. Avoid in management of delirium, consider specialist referral if further advice needed. Review appropriateness and indication for use with prescriber/ GP (often given for “dizziness”) Domperidone may be a suitable alternative. Drowsiness which can last into the next day, lightheadedness, confusion, loss of memory Review appropriateness and indication for use with prescriber/ GP. Stop if possible. Long term use will need slow withdrawal No new initiation on transfer of care – seek specialist advice if required. Sudden daytime sleepiness, dizziness, insomnia, confusion. Low blood pressure, blurred vision. May not be possible to change. Do not change without specialist opinion. Check for postural hypotension Dizziness, blurred vision,retention of urine,confusion, Review appropriateness and indication for use with prescriber/ GP. Reduce dose Cardiovascular Medication Analgesics Anticonvulsants drowsiness, hallucinations. or stop if possible. ACE inhibitors / AngiotensinII antagonists: Ramipril, Lisinopril, Captopril, Irbesartan, Candesartan. Vasodilators: Hydralazine Diuretics: Bendroflumethiazide, Bumetanide, Indapamide, Furosemide, Amiloride, Spironolactone, Metolazone. Betablockers: Atenolol, Bisoprolol, Carvedilol, Propranolol, Sotalol. Alphablockers: Doxazosin, Alfuzosin, Terazosin, (Tamsulosin). Opioids: Codeine, Tramadol, Nefopam, Dihydrocodeine, Buprenorphine, Alfentanyl Opiates: Morphine, Oxycodone. Low blood pressure, postural hypotension, dizziness, tiredness, sleepiness, confusion Check lying and standing BP. Review appropriateness and indication for use with prescriber/ GP (note alphablockers are also used for benign prostatic hyperplasia). Review dose. May not be possible to stop. Consider alternative to alphablocker. Drowsiness, confusion, hallucinations, postural hypotension. Review dose. • Use analgesic pain ladder to avoid excess use. • In older people start low and go slow Carbamazepine*, Sodium Valproate*, Gabapentin, Lamotrigine, Clonazepam, Phenytoin*, Phenobarbitone*, Primidone*. Drowsiness, dizziness, blurred vision. Consider indication (some are also used for pain control or mood stabilisation). • May need specialist review in problem cases. • *Consider Vitamin D supplements for at risk patients on long-term treatment with these drugs. Guidelines for Good Prescribing in Older Patients Carry out a regular medication review and discuss and agree all changes with the patient/carer. Make sure changes are highlighted in information to GP at Transfer of Care. Stop any current drugs that are not indicated. Check with GP for long term treatments e.g. antidepressants Prescribe new drugs that have a clear indication. Make sure changes (including the indication) are highlighted in information to GP at Transfer of Care. If possible, avoid drugs that have known deleterious effects in older people, such as benzodiazepines, and recommend dosage reduction when appropriate. Use the recommended dosages for older patients Use simple drug regimens and appropriate administration systems Consider using once daily or once weekly formulations and using fixed dose combinations when possible Consider non pharmacological treatments if appropriate Limit the number of people prescribing for each patient if possible Where possible, avoid treating adverse drug reactions with further drugs