Generic Competency Framework for Registered and Unregistered
advertisement

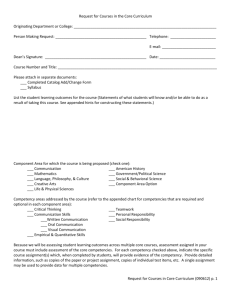
Generic Competency Framework for Registered and Unregistered Practitioners Version 4 Name of responsible (ratifying) committee Nursing and Midwifery Learning and Development Committee Date ratified 02/10/2012 Document Manager (job title) Head of Nursing and Midwifery Education Date issued 18/10/2012 Review date October 2015 Electronic location Nursing and Midwifery Related Procedural Documents Appraisal and Performance Review Policy Key Words (to aid with searching) Competencies, Nursing and Midwifery, Responsibly, Accountability. Development and Management of Procedural Documents: Version 4 Issue Date: 18/10/2012 (Review date October 2015 (unless requirements change) Page 1 of 21 CONTENTS 1. Introduction 2. Purpose 3. Scope 4. Definitions 5. Process 6. Duties and responsibilities 7. Training requirements 8. References and associated documentation 9. Equity impact 10. Monitoring compliance with procedural documents 11. Appendices: Appendix A: guidelines for writing a competency Appendix B: competency proforma (AC2) Appendix C: generic competency framework competency achievement requirements for registered practitioners Appendix D: generic competency framework competency achievement requirements for non registered practitioners Appendix E: minimum skill set for unregistered practitioners Appendix F: guidance on conduct for unregistered practitioners Development and Management of Procedural Documents: Version 4 Issue Date: 18/10/2012 (Review date October 2015 (unless requirements change) QUICK REFERENCE GUIDE 1. The policy provides a framework for the generic competencies required to be achieved and maintained to assure safe standards of care, and those to support professional and service development. 2. The purpose of the framework is to identify the Trust’s expectations for safe and effective practice. It provides a systematic and robust process for ensuring that the practice of all registered and unregistered practitioners (as stated in the scope) is consistent, safe and meets Trust and national requirements. 3. The policy applies to registered nurses, midwives, operating department practitioners, unregistered health care support workers, nursery nurses, associate practitioners and equivalent staff involved in the direct provision of patient care within Portsmouth Hospitals NHS Trust (PHT). 4. Competence and competences are job related, being a description of an action, behaviour or outcome that a person should demonstrate in their performance. 5. The framework recognises the profession specific regulatory requirements for registered staff and is intended to provide the process to regulate unregistered practitioners in association with the KSF. 6. Registered and unregistered practitioners will have access to information about the Generic Competency Framework during their induction period, and will agree priorities with their line manager within 4 weeks of commencing employment with the Trust. 7. Registered and unregistered practitioners will only practice a specific skill when they have been deemed competent to do so. 8. All registered practitioners who have already been deemed competent in a particular skill to at least level 3 will offer peer review and assessment in that skill as appropriate. 9. Registered, unregistered practitioners and their managers will maintain robust and easily accessible records of competency achievement via their learning records. 10. Staff who are involved in the development of a new competency will follow the agreed process (Appendix A), and use the validated proforma. (Appendix B). Development and Management of Procedural Documents: Version 4 Issue Date: 18/10/2012 (Review date October 2015 (unless requirements change) 1. INTRODUCTION This assurance framework sets the standard of expected performance for registered nurses, midwives, operating department practitioners, unregistered health care support workers, nursery nurses, associate practitioners and equivalent staff involved in the direct provision of patient care within Portsmouth Hospitals NHS Trust (PHT). The policy provides a framework for the generic competencies required to be achieved and maintained to assure safe standards of care, and those to support professional and service development. It is a local framework designed to complement the national competency frameworks listed below and is not intended as a replacement. 1.1 The NHS Knowledge and Skills Framework (KSF) (DOH 2004). The framework describes the knowledge and skills which NHS staff, excluding doctors, dentists and some senior managers, need to apply in their work to deliver quality services. These are described as generic and specific dimensions and every registered and unregistered practitioner will have those pertinent to their role identified in his or her KSF outline. This will inform their individual performance reviews. 1.2 Specialty Specific Frameworks. These are nationally or locally determined to meet the requirements of patients with specific needs. 2. PURPOSE The purpose of this framework is to identify the Trust’s expectations for safe and effective practice. It provides a systematic and robust process for ensuring that the practice of all registered and unregistered practitioners (as stated in the scope) is consistent, safe and meets Trust and national requirements e.g. Care Quality Commission Standards 13 and 14. 3. SCOPE The Generic Competency Framework applies to:Registered Practitioners: Registered nurses, (including registered children’s nurses and registered nurses employed by the Military of Defence) Registered Midwives Registered Operating Department Practitioners and Unregistered Practitioners involved in direct care: for example Associate/ Assistant practitioners Dialysis Assistants Health Care Support Workers/Clinic/Outpatient Support Workers/Maternity Support Workers Medical Assistants employed by the Ministry of Defence Medical Technicians Nursery Nurses Operating Department Assistants For the purposes of this document they will be referred to as registered and unregistered practitioners ‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety’ Development and Management of Procedural Documents: Version 4 Issue Date: 18/10/2012 (Review date October 2015 (unless requirements change) 4. DEFINITIONS 4.1 Competence/ Competency As with many concepts, there is no standard definition of competence. This framework reflects the combination of ideas as described in an article by McMullan et al (2003). Competence and competences are job related, being a description of an action, behaviour or outcome that a person should demonstrate in their performance. Competency and competencies are person orientated, referring to a person’s underlying characteristics and qualities that lead to effective/superior performance in their job. Therefore the expectations of the framework relate not only to effective performance but also to professional and skill development. 4.2 Professional Regulation The framework recognises the profession specific regulatory requirements as stated in the Nursing and Midwifery Council’s standards of conduct performance and ethics for nurses and midwives (2008) and the Health Care Professions Council’s standards of conduct, performance and ethics (2008). The Trust as an employer expects that registered practitioners maintain their self regulatory functions in accordance with their professional bodies and utilise the framework as evidence for professional portfolios. 4.3 Regulation of Unregistered Practitioners This framework is intended to provide the process to regulate unregistered practitioners in association with the KSF. The competencies provide additional specific care related standards of expected performance and support the minimum skill set. The unregistered nursing staff, including nursery nurses, are expected to achieve the minimum skill set as per their job description/role. The competencies provide evidence for performance review and should be maintained and updated by unregistered staff in a learning record/portfolio. 4.4 Accountability 4.41 Registered Practitioners are accountable to their professional bodies in accordance with the standards for conduct, performance and ethics, to the patient and public under civil and criminal law and their employer under employment law. Accountability to the employer is discharged by acting in accordance with organisational policy and procedure. 4.42 Unregistered Practitioners are accountable for their actions to the patient and public under civil and criminal law and to their employer under employment law. The expectation to follow their contract of duty which is their job description and act in accordance with organisational policy and procedure. 4.5 Responsibility Responsibility is a two way process which can be both given and accepted. Both registered and unregistered practitioners are responsible for their actions and the outcome of their actions if they accept responsibility for an aspect of care. 4.6 Delegation Delegation must not compromise existing care and must be directed at meeting the needs and serving the interests of patients and clients (NMC 2007). There is no specific guidance regarding which activities can or cannot be delegated (RCN 2006). The decision as to which activities are appropriate to delegate lies solely with the registered practitioner who is responsible for delegating work to an unregistered practitioner. Development and Management of Procedural Documents: Version 4 Issue Date: 18/10/2012 (Review date October 2015 (unless requirements change) 4.61 Registered Practitioners When a healthcare professional delegates you are authorising that person to perform aspects of care normally within your scope of practice. Registered practitioners remain accountable for the appropriateness of the delegation and for ensuring that the person who does the work is able to do it and adequate supervision or support is provided (NMC 2007). 4.62 Unregistered Practitioners The unregistered practitioner: Is accountable for accepting the delegated task as well as being responsible for his/her actions in carrying it out (RCN 2006). Work in accordance with the Guidance for the Conduct for Nursing and Midwifery Support Workers Should understand their limitations and not proceed if circumstances within which the task has been delegated changes. Meet the expectations of the minimum skill set by achieving the generic competencies to a minimum of level 1 and maintain competence. Should undertake training throughout their employment to ensure their competency in the tasks required. 4.7 Legal Duty of Care Once a practitioner assumes responsibility for the patient or undertakes to exercise his/her professional skills on the patient’s behalf, the practitioner owes the patient a legal duty of care. The standard of that duty is that of an ordinary competent practitioner (Bolitho 1988). 5. DUTIES AND RESPONSIBILITIES 5.1 Practising registered nurses, midwives and registered operating practitioners will operate in accordance with the standards and expectations set out in this document and:5.11 In accordance with the NMC and HCPC Standards of Performance, Conduct and Ethics, exercise self-assessment against all relevant competencies. Practitioners will agree relevant generic/specific competencies according to their sphere of practice with their line manager. 5.12 Newly appointed staff will complete the generic competencies at a minimum of level 2 within the first year of employment in time to meet the requirements of the foundation gateway. 5.13 Use their self-assessment to agree competency achievement priorities for their annual development plan. 5.14 Access education and learning resource opportunities to support competency achievement as per their annual development plan. 5.15 Provide evidence that their practice meets agreed competency standards and levels at annual appraisal. 5.16 Maintain own records/portfolio of competency achievements and submit this for audit purposes when requested. 5.17 Review/assess peers’ and unregistered practitioners’ practice (for competencies already achieved to at least level 3). 5.18 Only delegate tasks/ procedures that are appropriate to staff that are competent. 7.2 Unregistered Practitioners will operate in accordance with the standards and expectations set out in this document and:5.21 Only accept delegated responsibility for tasks/procedures in which they are competent. 5.22 Newly appointed staff will complete the generic competencies at a minimum of level 1 within the first year of employment in time to meet the requirements of the minimum skill set for the foundation gateway. 5.23 Use the competencies to guide practice and development needs within their performance reviews. Development and Management of Procedural Documents: Version 4 Issue Date: 18/10/2012 (Review date October 2015 (unless requirements change) 5.3 5.4 5.5 5.6 5.7 5.8 5.24 Access education and learning resource opportunities to support competency achievement as per their annual development plan. 5.25 Provide evidence that their practice meets agreed competency standards and levels at annual appraisal 5.26 Maintain own records/portfolio of competency achievements and submit this for audit purposes when requested. Line Managers/Professional Leads will: 5.31 Agree minimum competency requirements for their area of practice. 5.32 Adhere to Trust APDR policy. 5.33 Negotiate and agree individual staff member’s induction and orientation competencies for achievement within 4 weeks of commencing in Trust in order to determine induction and development plans. 5.34 Negotiate and agree annual development plans with individual staff members. 5.35 Manage a process to check each staff member’s developments/achievements annually against the standards and expectations for practice as set out in this document. 5.36 Maintain accurate and accessible records of staff member’s competency achievement. 5.37 Support the development of staff who are failing to progress their competency achievement in accordance with their individual development plan. 5.38 Identify where new competencies are required and initiate/action development of these. 5.39 Release staff to attend appropriate and agreed training sessions to support competency achievement. 5.310 Provide assurance annually to the Matron/Department Head that their staff, both registered and unregistered practitioners, meet the standards and expectations for practice as set out in this document. Matrons/ Department Head will: 5.41. Provide assurance annually to the Head of Nursing/Head of Midwifery that their staff, both registered and unregistered practitioners, meet the standards and expectations for practice as set out in this document. 5.42 Identify training requirements across their practice area, and ensure these are addressed in annual training plans. 5.43 Promote the value of the framework to all key staff groups. Head of Nursing/ Equivalent Post Holder will: 5.51 Monitor competency achievement across clinical service centre and ensure competency-training needs are being met through training plans. 5.52 Provide assurance annually to the clinical service centre Team that their staff, both registered and unregistered practitioners, meet the standards and expectations for practice as set out in this document. Practice Educators will: 5.61 Facilitate and support competency achievement with staff in their respective clinical areas. 5.62 Develop competencies as required and ensure they are based on the best available evidence. 5.63 Promote the value of the framework to all key staff groups. Named Competency Lead will: 5.71 Review their competency (ies) two yearly and ensure current evidence is incorporated appropriately. 5.72 Consult on proposed changes to competencies. 5.73 Ensure that the most current version of their competency (ies) is available on the Trust’s intranet (Nursing and Midwifery Education pages). 5.74 Work with the Head of Education for Nursing and Midwifery to implement appropriate education resources to support competency achievement. 5.75 Present revisions to competencies to the appropriate committee in a timely manner. Head of Education for Nursing and Midwifery will: Development and Management of Procedural Documents: Version 4 Issue Date: 18/10/2012 (Review date October 2015 (unless requirements change) 5.81 Oversee the implementation and ongoing management of the Generic Competency Framework. 5.82 On behalf of the Trust, ensure that all registered and unregistered practitioners are clear about minimum competency requirements. 5.83 Promote the value of the framework to all key staff groups. 5.84 Ensure all staff adhere to the correct process for developing and approving new competencies. 5.85 Ensure new competencies and any amendments are presented to the appropriate committee for ratification in a timely manner. 5.86 Monitor education resources to support competency achievement. 6. PROCESS 6.1 Registered and non registered practitioners who attend the introductory Setting Direction Programme will receive a personal copy of a Learning Record and the generic competencies via taught sessions as appropriate. 6.2 Registered and unregistered practitioners will have access to information about the Generic Competency Framework during their induction period, and will agree priorities with their line manager within 4 weeks of commencing employment with the Trust. 6.3 New staff will review their progress with their line manager every 3 months during the first year of their employment with the Trust and at least annually thereafter via the performance review process. Appraisal and Performance Review Policy (APDR) 6.4 All registered and unregistered practitioners will discuss their self/peer assessment against the minimum competency requirements of the framework with their line manager and agree an annual development programme for achieving new competencies and/or increasing levels of achievement. 6.5 Registered and unregistered practitioners will only practice a specific skill when they have been deemed competent to do so. 6.6 All registered practitioners who have already been deemed competent in a particular skill to at least level 3 will offer peer review and assessment in that skill as appropriate. 6.7 All registered nurses and midwives supporting and assessing learners in practice are required to meet the educational aspect of the Nursing and Midwifery Council (NMC) Standards for Mentorship through a NMC recognised preparation for mentorship course (NMC 2006) and in accordance with hospital policy. 6.8 Managers will facilitate registered and unregistered practitioners to attend annual updates, and individual practitioners are expected to access annual updates relating to competency achievement as required. 6.9 Registered, unregistered practitioners and their managers will maintain robust and easily accessible records of competency achievement via their learning records. 6.10. Staff who are involved in the development of a new competency will follow the agreed process (Appendix A), and use the validated proforma. (Appendix B). Development and Management of Procedural Documents: Version 4 Issue Date: 18/10/2012 (Review date October 2015 (unless requirements change) 7. TRAINING REQUIREMENTS Registered and unregistered practitioners are expected to undertake learning and development opportunities to support the development of their competence as required within their clinical area. Development plans will be discussed and agreed with Line Managers within the APDR process and education sessions and learning opportunities accessed as agreed in accordance with the Learning and Development Policy. 8. REFERENCES AND ASSOCIATED DOCUMENTATION DOH (2004). Knowledge and Skills Framework. London. HMSO DOH (2006) The regulation of the non-medical healthcare professions. HMSO Heath Care Professions Council (HCPC). (2008). Standards of Conduct, Performance and Ethics. Retrieved from HCPC website: http://www.hpcuk.org/assets/documents/10003B6EStandardsofconduct,performancean dethics.pdf Mc Mullan et al (2003). Portfolios and assessment of competence: a review of the literature. Journal of Advanced Nursing. 41. 3. 283-294. NMC (2007). Advice for delegation to non-regulated healthcare staff. www.nmc.org.uk NMC Code of Professional Conduct (2008) http://www.nmc-uk.org/nmc/main/publications/codeOfProfessionalConduct.pdf PHT Trust Policy Appraisal and Personal Development Review (2012) Appraisal and Personal Development Review Policy ( 2012) PHT Trust Policy Adverse Incident and Near Miss policy (2011) Adverse Event and Near Miss Policy ( 2011) RCN, CSP, RCSLT and BDA (2006). Supervision, accountability and delegation of activities to support workers. RCN (2006). The regulation of Health Care Support Workers Policy Briefing 11/2007. 9. EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This policy has been assessed accordingly. Development and Management of Procedural Documents: Version 4 Issue Date: 18/10/2012 (Review date October 2015 (unless requirements change) 10. MONITORING COMPLIANCE WITH PROCEDURAL DOCUMENTS This document will be monitored to ensure it is effective and to assurance compliance. Minimum requirement to be monitored Lead Tool Frequency of Report of Compliance Reporting arrangements Lead(s) for acting on Recommendations Policy audit report to: Policy audit report to: Policy audit report to: The effectiveness in practice of all procedural documents should be routinely monitored (audited) to ensure the document objectives are being achieved. The process for how the monitoring will be performed should be included in the procedural document, using the template above. The details of the monitoring to be considered include: The aspects of the procedural document to be monitored: identify standards or key performance indicators (KPIs); The lead for ensuring the audit is undertaken The tool to be used for monitoring e.g. spot checks, observation audit, data collection; Frequency of the monitoring e.g. quarterly, annually; The reporting arrangements i.e. the committee or group who will be responsible for receiving the results and taking action as required. In most circumstances this will be the committee which ratified the document. The template for the policy audit report can be found on the Trust Intranet Trust Intranet -> Policies -> Policy Documentation The lead(s) for acting on any recommendations necessary Development and Management of Procedural Documents: Version 4 Issue Date: 18/10/2012 (Review date October 2015 (unless requirements change) APPENDIX A: GUIDELINES FOR WRITING A NURSING/MIDWIFERY COMPETENCY Wards and departments are required to produce speciality specific competencies to ensure safety and consistency of practice for nurses and midwives. This document is intended to provide guidance to ensure a standardised process in constructing these competencies. Guidelines 1. Before writing a competency complete the proposal form (AC1) for developing a new competency. Send to the Head of Education for Nursing and Midwifery to ensure that the competency does not exist already. The reply will be via email within 7 days. 2. New competencies are to be produced in accordance with the agreed Trust proforma (form AC2). Please see appendix B 3. Competency levels 1 - 4 are based on the Agenda for Change, Knowledge and Skills Framework (DoH 2004). These are intended to map skills from a minimum level of safety to expert but are not grade specific. Wards/departments will require staff to achieve different levels of skills to meet patient need so you need to indicate which level is expected to be achieved by which staff groups in your competency. Please refer to appendix B for an example of this. 4. Educational resources are to be stated within the competency document to support and guide staff development through the competency levels. These may include formal study days/modules, recommended reading, e-learning etc. 5. The competency is to be based on evidence, which is essential to ensure safe and effective practice. References are to be documented in the reference section on the back of the competency document. 6. The originator/specialty is responsible for the review of the competency, which is required annually to ensure currency of practice. The author’s name, department, date of completion and review date are to be stated on the competency document. 7. Ensure multi-professional consultation on the competency document including departmental 8. Managers if financial commitment is required to support staff’s competency development. 9. Submit draft of competency via email to the Head of Education for guidance/support in completing the competency as per the Trust format. This will be returned to you within 14 days. 10. The competency requires ratification prior to use. Return the completed document to the Head of Education who will submit it to the Nursing and Midwifery Learning and Development Committee (NMLDC). This forum will ratify the competency and inform you of the outcome. Development and Management of Procedural Documents: Version XX Issue Date: XXXX (Review date XXX (unless requirements change) Proposal Form for Developing a Nursing/Midwifery Competence (AC1) Name Position Contact no/email Department & Division Title of proposed competence Rationale for Competence e.g. new practice/updated clinical evidence Overview of evidence to support competency development Staff roles covered by competency e.g. HCSWs, RNs, RMs, RODPs etc Signature Date Competency Requirement Agreed 1. Y / N Rationale if No Head of Education Nursing/Midwifery: signature Date Development and Management of Procedural Documents: Version XX Issue Date: XXXX (Review date XXX (unless requirements change) APPENDIX B – COMPETENCY PROFROMA (AC2) Competency Statement: st Competency Indicators 1 Level Achieved Assessor Signature Competency Indicators 2nd Level Achieved Assessor Signature Competency Indicators 3rd level Achieved Assessor Signature Competency Indicators 4th level Achieved Assessor signature Education resources to support your development Author: Department: Review Date: Record of Achievement. To verify competence please ensure that you have the appropriate level signed as a record of your achievement in the boxes below either by the educator/ trainer if attendance on study session and or the workplace assessor when performed in practice. Level 1 Level 2 Level 3 Level 4 Date: Signature of Educator/ Trainer Date: Signature of Educator/ Trainer Date: Signature of Educator/ Trainer Development and Management of Procedural Documents: Version XX Issue Date: XXXX (Review date XXX (unless requirements change) Date: Signature of Educator/ Trainer Date Date Date Date Signature of Workplace Assessor Signature of Workplace Assessor Signature of Workplace Assessor Signature of Workplace Assessor References to Support Competency Development and Management of Procedural Documents: Version XX Issue Date: XXXX (Review date XXX (unless requirements change) Appendix C: GENERIC COMPETENCY FRAMEWORK COMPETENCY ACHIEVEMENT REQUIREMENTS FOR REGISTERED PRACTTIONERS 1. The competencies stated in this section are the minimum expected to be achieved by registered practitioners and have been included to reflect current clinical priorities. The list is not exhaustive and will be reviewed in line with the policy review date. 2. The competencies are expected to be completed to at least level 2 within the first year of employment in time for the foundation gateway. 3. All registered staff are expected to achieve and maintain a minimum of level 2 competence. 4. Additional competencies and levels to be achieved will be identified by clinical specialties based on patient and service requirements. 5. The individual practitioners are expected to keep a record of their achievements which they will utilise in their APDR. Staff Groups All Registered Nurses, Midwives and Operating Department Practitioners Ward/Dept based front line staff involved in direct patient care as appropriate to clinical requirements Competencies Basic Life Support or specialty equivalent. (maternal, neonatal, child health) Adult/child Anaphylaxis Patient centred dignity in care Documentation Assess physical wellbeing of the adult Administration of blood products** Administration of medication Prevention of Falls Moving and Handling Nutrition Prevention of Pressure Ulcers Taking, recording and assessment of vital signs in adults Comments **Only for staff involved in handling blood products Please Note: The competencies do not include hand hygiene as all staff are expected to comply with the policy and practice, the 7 step technique, which is assessed in regular compliance audits. Development and Management of Procedural Documents: Version XX Issue Date: XXXX (Review date XXX (unless requirements change) Appendix D: GENERIC COMPETENCY FRAMEWORK COMPETENCY ACHIEVEMENT REQUIREMENTS FOR NON REGISTERED PRACTTIONERS 1. The competencies stated in this section are the minimum expected to be achieved by the unregistered practitioners and have been included to reflect current clinical priorities. The list is not exhaustive and will be reviewed in line with the policy review. 2. The competencies are expected to be completed to at least level 1 to meet the requirements of the Minimum Skill Set for Unregistered Practitioners. 3. All unregistered staff are expected to achieve and maintain a minimum of level 1 competence. 4. Additional competencies and levels to be achieved will be identified by clinical specialities based on patient and service requirements. 5. The individual practitioners are expected to keep a record of their achievements which they will utilise in their APDR. Staff Groups All non Registered Practitioners excluding Maternity Support Workers (see section below) Ward/Dept. based front line staff involved in direct patient care as appropriate to clinical requirements Maternity Support Workers Competencies Basic Life Support or specialty equivalent. (maternal, neonatal, child health) Adult/child Anaphylaxis Patient centred dignity in care Documentation Comments Personal Care Elimination Assess physical wellbeing of the adult Prevention of Falls Moving and Handling Nutrition Prevention of Pressure Ulcers Taking, recording and assessment of vital signs in adults To achieve all competencies as identified in the Maternity Support Worker Competency Framework which is specific to Maternity Services. Please Note: The competencies do not include hand hygiene as all staff are expected to comply with the policy and practice, the 7 step technique, which is assessed in regular compliance audit. Development and Management of Procedural Documents: Version XX Issue Date: XXXX (Review date XXX (unless requirements change) Appendix E Minimum Skill Set for Health Care Support Workers and Nursery Nurses Portsmouth Hospitals Minimum Skill Set for Health Care Support Workers and Nursery Nurses Portsmouth Hospitals has set a minimum level of expectation for the role of the Health Care Support Worker and Nursery Nurse. Each unregistered member of nursing staff must ensure that they are competent to deliver the care and seek education to support them to meet their role. Minimum Skill Set Expectations Core Skills Components 1. Patient Safety Basic Life Support Routine monitoring of vital Signs (temperature, pulse, respiration rate blood pressure, oxygen saturations, level of consciousness via AVPU and to include blood glucose) Recognition of an ill patient Moving and handling Falls prevention Health and safety Personal and environmental infection prevention and control to include ward equipment and priority cleaning Safeguarding the vulnerable adult and child Reporting risks to include completing adverse incident forms Supporting relatives and carers in the care the patient e.g. listening to patients/carers raising issues, to help raise concerns and to help resolve concerns to avoid progression to a formal complaint 2. Communication Feedback on care provision Record keeping to include recording basic patient information and demographic detail as well as care provision. Appropriate communication with patients and relatives and in challenging situations e.g. deaf, confused, upset, aggrieved. Using basic Trust information technology e.g. patient access system (PAS) electronic rostering and email Maintaining confidentiality & data protection Access to patient records Obtain patients consent in accordance with policy Employ appropriate telephone skills 3. Being an Effective Being accountable for your actions Team Member Understanding and responding appropriately to delegation Ensuring equality & diversity Professional behaviours e.g. treating patients and team members with respect. Upholding the Trust values Development and Management of Procedural Documents: Version XX Issue Date: XXXX (Review date XXX (unless requirements change) 4. Respect for Others 5. Personal Hygiene 6. Continence 7. Nutrition 8. Pressure Area Care 9. Planned Simple Discharge 10. End of Life Care Resource management and reducing waste Supporting learners Delivering customer service in accordance with the Trust values Maintaining privacy and dignity in accordance with the Trust’s dignity charter Assisting to wash in for example bed, bath and or shower Providing oral hygiene Care of hair, nails and feet Providing eye care Assist patients to the toilet and managing incontinence Using bedpans, commodes Catheter care Specimen taking Emptying urinary devices Assist with eating and drinking Promote independence Monitor and record weight, height and Body Mass Index (BMI) Recording food and fluid input/output Recognition of vulnerable pressure areas Provide skin care Moving and turning Maintenance and ordering of equipment Tablet To take Home (TTO) collection Ordering transport Completing discharge checklist and giving discharge leaflets to patients Communicating with families/ carers Managing patient property Care skills and knowledge of Liverpool Care Pathway and last offices Assisting in last offices Supporting bereaved relatives Please discuss this with you Ward Sister/Charge Nurse to recognise the skills you have and to action plan how you maintain and develop to meet the skill set. This will be monitored as part of your annual appraisal. Development and Management of Procedural Documents: Version XX Issue Date: XXXX (Review date XXX (unless requirements change) Appendix F: Guidance on Conduct for Nursing and Midwifery Support Workers Guidance on Conduct for Nursing and Midwifery Support Workers This guide is designed to help you set the standard for how you work on a day to day basis. It is based on the key principle of protecting the public and mirrors what is required from professionals who are formally regulated. You have a significant impact on the quality of service delivered within the Trust and the following guidance identifies the standards of behaviour and attitudes that are required from all Nursing and Midwifery Support Staff* working within Portsmouth Hospitals NHS Trust. The clinical responsibilities and activities of all staff who support the delivery of nursing and midwifery services are defined within individual job descriptions and the knowledge and skills framework outlines. Role boundaries are also agreed in accordance within Portsmouth Hospital NHS Trust policies and guidelines within relevant legal frameworks. Delegation This is the transfer of authority to a competent individual to enable a specific task to be performed in a specified situation without direct supervision. Delegation of care must always take place in the best interests of the patient and be based on individual patient need. The registered practitioner delegating an aspect of care is held accountable for the appropriateness of that delegation. If you accept a task you become accountable for the performance of that task. The registered practitioner is accountable for ensuring that the outcome of delegated tasks meet the required standards. Accountability This is the principle that individuals, organisations and the community are responsible for their actions and that you should be able to explain your actions to others if required. You are accountable for your actions when work is delegated to you. You are also accountable for any actions you do not take when you might have been reasonably expected to anticipate that distress or harm may arise. Responsibility You are responsible to your manager for your standard of performance. Delegated tasks must fall within your job description and your level of competence. Competence Competent practice requires appropriate skill, knowledge, understanding and attitude to perform a task safely and effectively without direct supervision. Development and Management of Procedural Documents: Version XX Issue Date: XXXX (Review date XXX (unless requirements change) * This guidance applies to all staff who work under the delegated authority of the Registered Nurse or Midwife. This includes Health Care Support Workers, Maternity Support Workers, Out-Patient Support Workers , Nursery Nurses, Dialysis Assistants etc. This list is not intended to be exhaustive Expected Conduct for Nursing and Midwifery Support Workers The following guidance is based on the Royal College of Nursing Principles of Nursing Practice (2010) What this means to you is: 1. Respect, protect and promote the dignity and privacy of patients and provide compassionate and sensitive care in a way that respects all people equally. 2. Always act under the direction and supervision of a registered practitioner. 3. Ensure that you carry out all activities safely, effectively and to the best of your abilities, in accordance with the policies and protocols of the Trust and relevant legal obligations. 4. Be aware of potential risks to patients and act immediately to ensure their safety and be conscientious in reporting any concerns or complaints. 5. Ensure that the patient is central to the delivery of care. Work in partnership with patients, families and carers to support their rights to make informed choices, be independent and selfmanage their treatment and care. 6. Handle patient information sensitively and treat all information about patients as confidential. 7. Work constructively with all members of your own team and other health care colleagues: respect their skills and contribution to ensure that care delivered is of a high standard and promotes the best possible outcomes. 8. Do not take on an activity unless you have the relevant knowledge and skills to do so and have been assessed as competent to carry it out safely and effectively. 9. If you do not feel ready to take on an activity, report this to a registered practitioner and ask them to help you develop or update to ensure that you have up-to-date knowledge and skills. 10. Maintain your Learning Record. This will provide evidence of Essential Skills training and of relevant other learning and will enable you to demonstrate nursing competencies achieved in practice. Development and Management of Procedural Documents: Version XX Issue Date: XXXX (Review date XXX (unless requirements change) References Please also refer to associated documents Heath Care Professions Council (HCPC). (2008). Standards of Conduct, Performance and Ethics. Retrieved from HCPC website: http://www.hpcuk.org/assets/documents/10003B6EStandardsofconduct,performanceandethics. pdf Nursing Midwifery Council (2008) Code of Professional Conduct. London: Nursing and Midwifery Council. Retrieved from NMC website: www.nmc.org.uk Royal College of Nursing (2007) Policy Briefing 11/2007 The Regulation of Health Care Support Workers. London Royal College of Nursing (2008) Health Care Assistants and Assistant Practitioners Delegation and Accountability. Nursing Standard Essential Guide. Middlesex Royal College of Nursing (2010) Principles of Nursing Practice. RCN Bulletin. Nov 2010. p5 . Development and Management of Procedural Documents: Version XX Issue Date: XXXX (Review date XXX (unless requirements change)