Chest physiotherapy in mechanically ventilated children: A review
advertisement

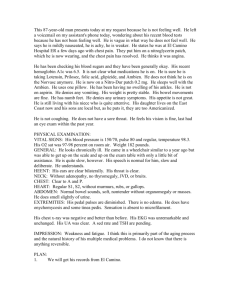
Chest physiotherapy in mechanically ventilated children: A review Crit Care Med. 2000 May;28(5):1648-51. Krause, Martin F. MD; Hoehn, Thomas MD Author Information From the Children's Hospital, Albert-Ludwigs-University, Freiburg, Germany. Address requests for reprints to: Martin F. Krause, MD, University Children's Hospital, Mathildenstr. 1, D79106 Freiburg, Germany. E-mail: Krause@kkl200.ukl.uni-freiburg.de Back to Top Abstract Objective: Many physicians, nurses, and respiratory care practitioners consider chest physiotherapy (CP) a standard therapy in mechanically ventilated children beyond the newborn period. CP includes percussion, vibration, postural drainage, assisted coughing, and suctioning via the endotracheal tube. Data Sources: We searched the medical literature by using the key words "chest physiotherapy" and "chest physical therapy" (among others) by means of the MEDLINE and Current Contents databases. Study Selection: Because of the paucity of objective data, we examined all reports dealing with this topic, including studies on adult patients. For data extraction, not enough material existed to perform a meta-analysis. Data Synthesis: Despite its widespread use, almost no literature dealing with this treatment modality in pediatric patients exists. Studies with mechanically ventilated pediatric and adult patients have shown that CP is the most irritating routine intensive care procedure to patients. An increase in oxygen consumption often occurs when a patient receives CP accompanied by an elevation in heart rate, blood pressure, and intracranial pressure. CP leads to short-term decreases in oxygen, partial pressure in the blood, and major fluctuations in cardiac output. Changes in these vital signs and other variables may be even more pronounced in pediatric patients because the lung of a child is characterized by a higher closing capacity and the chest walls are characterized by a much higher compliance, thus predisposing the child to the development of atelectasis secondary to percussion and vibration. Conclusion: CP in mechanically ventilated children may not be considered a standard therapy. Controlled studies examining the impact of CP on the duration of mechanical ventilatory support, critical illness, and hospital stay are needed. Chest physiotherapy (CP) has been advocated in the field of pediatrics for >20 yrs and has emerged as a standard treatment modality in young patients with pulmonary diseases (1). Different techniques of CP have been studied in a variety of different lung diseases in children with an almost unpredictable effect. A "positive effect" of CP has, in general, been defined as an acute improvement in the patient's overall appearance, lung auscultation, blood gas tensions, and chest radiographs (2). The volume of expectorated lung secretions after CP will be underestimated because parts of the secretions will be swallowed by the pediatric patient (3). CP has produced different effects on spontaneously breathing patients with a variety of acute pulmonary diseases. No improvement in lung function occurred in children with exacerbated bronchial asthma who received CP (4). CP seems to be of little value in the treatment of bronchiolitis. No favorable influence on lung mechanics (5), a rapid recovery, or earlier discharge from the hospital (6) was detected. Studies in adult patients with pneumonia (7) failed to detect any influence on the duration of fever, clearing of radiodensities on chest radiographs, duration of hospitalization, or mortality rate. In a controlled study with young adults (8), CP led to prolonged fever and hospital stay in the treated group. In contrast, CP has emerged as a standard treatment modality for young patients with cystic fibrosis. Its effectiveness has been proven by numerous studies (9, 10). However, CP does not improve pulmonary status in all chronic lung diseases. Wollmer et al. (11) studied adult patients with acutely exacerbated chronic bronchitis. Percussion, assisted coughing, and postural changes did not lead to improvements in this condition. A beneficence has been reported in pediatric lung abscess in children aged >7 yrs (12), acute lobar atelectasis (13), and lung complications after traumatic quadriplegia (14). The latter two studies included only adult patients. Therefore, we searched the literature for reports of the effectiveness of CP in mechanically ventilated pediatric patients. Children usually develop respiratory failure because of acute pulmonary diseases for which they receive mechanical ventilatory support. We limited our search to studies involving patients treated with mechanical ventilatory support to overcome respiratory failure caused by acute pulmonary diseases. Literature Search. We searched the literature by using the key words "chest physiotherapy" or "chest physical therapy," "mechanical ventilatory support," "children," and "vital signs" with the help of the MEDLINE and Current Contents databases. Reference lists of all related articles were checked for further articles of interest. Chest Physiotherapy Techniques. The following CP techniques are thoroughly described in the international literature for use in mechanically ventilated patients (1, 15): a) manual percussion with proper cupping of hand or with a face mask; b) vibration of the chest wall transmitting energy through the chest wall to loosen or move bronchial secretions; c) postural drainage using gravity to move secretions from peripheral airways to the larger bronchi; d) assisted coughing to transport loosened secretions from the bronchial tree to the trachea; and e) suctioning of secretions via the endotracheal tube. Other CP techniques, such as with contact breathing or guided breathing, have been advocated. No studies are available evaluating their effectiveness. Studies in Mechanically Ventilated Children. Despite our extensive literature search, we found only the following two studies that involve mechanically ventilated children beyond the neonatal age. Reines et al. (16) describe the effects of CP in 44 cardiac patients aged 3 months through 9 yrs. Vibration and percussion, postural drainage (including the head-down position), and endotracheal suctioning were all used. In the CP group, 13/19 (68%) vs. 8/25 (32%) patients of the control group developed atelectasis after cardiac surgery, with the consequence of a longer hospital stay for those patients in the CP group. The two groups of patients showed no differences in age, incision site (sternotomy vs. lateral thoracotomy), and percentage of cardiac lesions with left-to-right shunt. Reines et al. speculated that this apparent reversal of expected results could be caused by a number of factors, such as an increase in ventilation-perfusion mismatch resulting from mucus moving from peripheral to central airways, lung compression from percussion, decrease in functional residual capacity because of pain induced by CP and hypoventilation in the head-down position. This study did not provide data on the length of mechanical ventilatory support postoperatively or the number of CP treatments during or after mechanical ventilatory support. Zach et al. (17) observed a high solution quota (>95%) of atelectases in children treated with CP. A minority of patients received mechanical ventilatory support. This study used a historical control group for comparison of results, omitted distinguishing children receiving mechanical ventilatory support from those breathing naturally, and did not describe the CP techniques used. Studies in Mechanically Ventilated Adult Patients. Applying the data from studies evaluating the effectiveness of CP in mechanically ventilated adult patients when considering benefits and burdens of CP in pediatric patients under these clinical conditions may be inappropriate because the specific physiologic properties of lung and chest wall of children differ from adults. All of the following studies used a variety of CP techniques mentioned above. Laws and McIntyre (18) were first to investigate the influence of CP on oxygenation and cardiac output in six mechanically ventilated patients in 1969. Their introduction states: "Chest physiotherapy has become accepted as an essential and valuable adjunct to the care of patients undergoing artificial ventilation for respiratory failure." No significant differences in oxygenation during and immediately after CP could be detected when comparing the results to the situation before initiating CP. However, a rise or fall by as much as 50% of the initial cardiac output was observed. Gormezano and Branthwaite (19) looked for changes in gas exchange 5 to 30 mins after CP in 42 patients on ventilatory support for reasons of major general surgery, respiratory failure, and cardiac diseases. Significant decreases in PaO2 and increases in PaCO2 could be detected, especially in those patients with low cardiac output or respiratory failure. Gormezano and Branthwaite postulated that the increase in intrathoracic pressure exerted by CP could lower the cardiac output so that for a given shunt effect, mixed-venous PO2 and, hence, PaO2 would fall. Similar results were obtained by Connors et al. (20) in 22 mechanically ventilated patients. Connors et al. claimed that an increase in ventilation-perfusion mismatch as responsible for the deterioration in oxygenation. Decrease in PaO2 was more pronounced in a subgroup of patients with less production of lung secretions. These findings were backed up by the results of Tyler et al. (21) describing a decrease of PaO2 by 18 mm Hg (75-57 mm Hg; 2.4, 9.9 to 7.6 kPa) during the sequence of CP. Tyler et al. emphasized the necessity of a thorough monitoring of the patient's vital signs during CP, especially for those patients with a low baseline PaO2. Results vary in studies involving the influence of CP on gas exchange in mechanically ventilated patients. Mackenzie et al. (22) could not detect any negative effect of CP on oxygenation during or after intervention in 47 patients. They were convinced that the use of an end-expiratory pressure of 510 cm H2O (0.5-1.0 kPa) prevented the fall in PaO2 observed by other authors. Mackenzie and Shin (23) found an improvement in oxygenation immediately and 2 hrs after CP, accompanied by small improvements in lung compliance and intrapulmonary shunt. They reported marked individual changes for cardiac index and intrapulmonary shunt among the patients. Weissman and Kemper (24) calculated a mean increase in oxygen consumption during CP of +62% ± 29% above the baseline level in 16 critically ill surgical patients. Weissman et al. (25) were able to identify two different groups of patients regarding their hemodynamic response during CP. The intervention resulted in an increase in oxygen consumption in all patients as verified by a significantly higher oxygen extraction (35% to 50%) in the vascular periphery or by a higher oxygen supply through the cardiorespiratory response that was reflected by an overall increase in heart rate, systemic blood pressure, and minute ventilation. Those patients reacting with an increase in oxygen extraction in the vascular periphery were those with an almost unchanged cardiac output reflecting absent cardiac reserve. The increased oxygen demand during CP is mainly because of increased muscle activity because administration of a muscle relaxant (in combination with a sedative) leads to a complete abolition of this side effect (26). Increases in heart rate and systemic blood pressure are not influenced by muscle relaxants because these side effects are a result of increased sympathetic output. Our literature search detected a single clinical study dealing with physiologic aspects other than gas exchange and hemodynamics after CP. MacLean et al. (27) proved that CP positively influences maximum expiratory flow rates in mechanically ventilated patients, and this effect could even be augmented when administering an increased pressure on the epigastric area of the patient treated. Weissman et al. (28) demonstrated in 23 mechanically ventilated patients that CP met with the most pronounced variations of vital signs when compared with other routine daily intensive care activities. CP caused an average increase in oxygen consumption of 38% and an 35% increase in CO 2 production as well as marked increases in heart rate and systemic blood pressure when compared with spontaneous movements, physical exam, presence of visitors, bathing, dressing, and taking chest radiographs. Administration of 3 µg/kg fentanyl immediately before beginning CP clearly attenuated the hemodynamic response (heart rate, systemic blood pressure, cardiac output, PaO 2, PaCO2 and minute ventilation) to CP (29). In contrast, 1.5 µg/kg fentanyl was not superior to placebo when comparing those above-mentioned vital signs. We were unable to find a single study dealing with the influence of CP on the weaning process or weaning strategy and the duration of mechanical ventilatory support. All available data are confined to short-term effects such as hemodynamics, gas exchange, or lung function as acute changes after CP. Therefore, we do not know from clinical data whether CP really contributes to shortening the duration of mechanical ventilatory support. Study with Research Animals. Zidulka et al. (30) demonstrated in mechanically ventilated dogs after muscle relaxation that percussion of the lungs with cupped hands (comparable with the clinical setting) leads to esophageal pressure swings of 10-17 cm H2O (1.0-1.7 kPa). Consecutive histopathologic examinations of the lungs immediately after termination of the treatment and killing of the animals showed large atelectatic areas adjacent to the areas of the chest wall where CP was administered. Moreover, there were atelectatic areas on the surface of the opposite lung to be seen that could be best described as a contra-coup effect. Zidulka et al. speculated that worsening of oxygenation, demonstrated in numerous clinical studies during and immediately after CP, happens because of the induction of atelectasis in treated lungs. They recommended giving patients a couple of deep breaths after termination of CP to overcome ventilation-perfusion mismatch caused by the formation of atelectases. Special Properties of Lungs in Pediatric Patients. The special properties of the lungs in pediatric patients must be considered when applying therapy for respiratory failure found to be beneficial in adult patients to children. First, closing capacity refers to the volume of gas present in the lung at the point that small conducting airways begin to collapse. In children aged >6 yrs, functional residual capacity exceeds closing capacity. In infants and in children <6 yrs of age, however, the closing capacity exceeds functional residual capacity (31). Second, the increasing chest wall stiffness with age leads to a diminishing ratio of compliance of the chest wall:lung compliance (Cw/Cl) with age. A value of ~3-6 occurs in infancy, 2 in early childhood, unity in young adulthood, and 0.5 in the elderly (32). For these two reasons, infants and children are more prone to developing atelectasis associated with a variety of pulmonary diseases and CP may lead to atelectasis in young patients after the administration of vibration and percussion to the chest wall. Burden of Chest Physiotherapy in Children. Vandenplas et al. (33) demonstrated a significant increase in gastroesophageal reflux prevalence while administering CP in 63 spontaneously breathing infants, ranging in age from 1 to 4 months. Gastroesophageal reflux was defined as an episode of esophageal pH <4 as measured by an esophageal pH probe. All three components of CP (percussion, vibration, and postural drainage) were linked with an increased prevalence of gastroesophageal reflux when compared with a control group. Vandenplas et al. observed that there was no timely relation of gastroesophageal reflux episodes and coughing during treatment. They concluded that CP should only be administered in the fasting infant because of the potential risk of developing aspiration pneumonia. Dependent head position as part of the postural drainage regimen in CP leads to an increase in intracranial pressure (ICP) as demonstrated by Emery and Peabody (34) in 14 mechanically ventilated newborns with or without perinatal asphyxia. Use of a 30° head-down position resulted in an increase in ICP from 13.8 ± 2.5 cm H2O (1.38 ± 0.25 kPa) to 17.2 ± 2.0 cm H2O (1.72 ± 0.2 kPa) and was even augmented by a concomitant lateral position to a maximum of 25.0 ± 2.6 cm H 2O (2.5 ± 0.26 kPa). Perlman and Volpe (35) described a significant increase in cerebral blood flow velocity and ICP after routine suctioning of 34 preterm infants. These increases subsided only gradually after cessation of the procedure. Similar results were obtained in 12 comatose adult patients after suctioning or hyperinflation of the lungs as part of a regimen to clear lung secretions. ICP rose by 34% and 31%, respectively, in comparison with baseline values before commencement of these procedures. In some patients, ICP increased by as much as +70 mm Hg (+9.3 kPa) (36). Raval et al. (37) reported a frequency rate of grades III/IV intracranial hemorrhages in 5/10 preterm infants treated with CP within the first 24 hrs of life vs. a frequency rate of 0/10 in an untreated control group. McCulloch et al. (38) observed a marked increase in skin blood flow in mechanically ventilated newborns who received CP. In a recent study from Bloomfield et al. (39), 220 newborn infants of all gestational ages with respiratory failure received periextubation CP or no CP to assess its effect on the prevention of postextubation atelectasis. Postextubation atelectasis occurred in 23% of the treated and in 15% of the untreated infants (difference statistically not significant). Moreover, a larger subgroup of infants receiving mechanical ventilatory support beyond 28 days of life could be identified in the group treated with CP. Summary of the Literature Reviewed. CP in mechanically ventilated adult patients is associated with acute changes in the following physiologic variables: a) gas exchange-decrease in PaO2, increase in PaCO2; b) sympathetic output-increases in heart rate and systemic blood pressure; c) lung physiologyincrease in minute ventilation, increase in maximum expiratory flow rate; d) increases in oxygen consumption and oxygen extraction in the vascular periphery (the latter especially in patients who are unable to increase their cardiac output); and e) increases in intracranial pressure. CP administered in pediatric patients is associated with the following: a) a higher rate of atelectasis and a longer hospital stay; b) a higher frequency rate of gastroesophageal reflux; and c) increases in intracranial pressure, cerebral blood flow velocity and a higher rate of intracranial hemorrhage in mechanically ventilated newborn infants. Closing Remarks. In mechanically ventilated children, CP cannot be regarded as a standard treatment modality. CP must be considered as the most stimulating and disturbing intensive care procedure in mechanically ventilated patients and should not be administered in children with low cardiopulmonary reserve attributable to an increased oxygen consumption and increases in intracranial pressure. CP should only be administered to critically ill patients whose respiratory gas exchange and hemodynamics are monitored. CP should be evaluated in controlled studies that consider the length of mechanical ventilatory support, influence on weaning the patient from the ventilatory support, occurrence of atelectases, and length of hospital stay. Variations of response to CP in different age groups because of changing physiologic properties such as closing capacity and chest wall compliance should also be assessed. Back to Top REFERENCES 1. Lewis R: Chest physical therapy. In: Perinatal and Pediatric Respiratory Care. Barnhart SL, Czervinske MP (Eds). Philadelphia, WB Saunders, 1995, pp 218-238 [Context Link] 2. Mellins RB: Pulmonary physiotherapy in the pediatric age group. Am Rev Respir Dis 1974; 110:137142 Bibliographic Links [Context Link] 3. Etches PC, Scott B: Chest physiotherapy in the newborn: Effect on secretions removed. Pediatrics 1978; 62:713-715 Bibliographic Links [Context Link] 4. Asher MI, Douglas C, Airy M, et al: Effects of chest physical therapy on lung function in children recovering from acute severe asthma. Pediatr Pulmonol 1990; 9:146-151 Bibliographic Links [Context Link] 5. Quittell LM, Wolfson MR, Schidlow DV: The effectiveness of chest physical therapy (CPT) in infants with bronchiolitis. Am Rev Respir Dis 1988; 137:406A [Context Link] 6. Webb MSC, Martin JA, Cartlidge PHT, et al: Chest physiotherapy in acute bronchiolitis. Arch Dis Child 1985; 60:1078-1079 Bibliographic Links [Context Link] 7. Graham WGB, Bradley DA: Efficacy of chest physiotherapy and intermittent positive-pressure breathing in the resolution of pneumonia. N Engl J Med 1978; 299:624-627 Bibliographic Links [Context Link] 8. Britton S, Bejstedt M, Vedin L: Chest physiotherapy in primary pneumonia. BMJ 1985; 290:1703-1704 Bibliographic Links [Context Link] 9. Thomas J, Cook DJ, Brooks D: Chest physical therapy management of patients with cystic fibrosis. A meta-analysis. Am J Respir Crit Care Med 1995; 151:846-850 Bibliographic Links [Context Link] 10. Coates AL: Chest physiotherapy in cystic fibrosis: Spare the hand and spoil the cough? J Pediatr 1997; 131:506-508 Buy Now Bibliographic Links [Context Link] 11. Wollmer P, Ursing K, Midgren B, et al: Inefficiency of chest percussion in the physical therapy of chronic bronchitis. Eur J Respir Dis 1985; 66:233-239 Bibliographic Links [Context Link] 12. Kosloske AM, Ball WS, Butler C, et al: Drainage of pediatric lung abscess by cough, catheter, or complete resection. J Pediatr Surg 1986; 21:596-600 Full Text Bibliographic Links [Context Link] 13. Stiller K, Geake T, Taylor J, et al: Acute lobar atelectasis. A comparison of two chest physiotherapy regimens. Chest 1990; 98:1336-1340 Bibliographic Links [Context Link] 14. McMichan JC, Michel L, Westbrook PR: Pulmonary dysfunction following traumatic quadriplegia. Recognition, prevention and treatment. JAMA 1980; 243:528-531 Bibliographic Links [Context Link] 15. Kirilloff LH, Owens GR, Rogers RM, et al: Does chest physical therapy work? Chest 1985; 88:436-444 Bibliographic Links [Context Link] 16. Reines HD, Sade RM, Bradford BF, et al: Chest physiotherapy fails to prevent postoperative atelectasis in children after cardiac surgery. Ann Surg 1982; 195:451-455 Request Permissions Buy Now Bibliographic Links [Context Link] 17. Zach M, Oberwaldner B, Purrer B, et al: Thoraxphysiotherapeutische Behandlung bronchopulmonaler Erkrankungen des Kindesalters. Monatsschr Kinderheilkd 1981; 129:633-636 Bibliographic Links [Context Link] 18. Laws AK, McIntyre RW: Chest physiotherapy: A physiological assessment during intermittent positive pressure ventilation in respiratory failure. Can Anaesth Soc J 1969; 16:487-493 Bibliographic Links [Context Link] 19. Gormezano, J, Branthwaite MA: Effects of physiotherapy during intermittent positive pressure ventilation. Changes in arterial blood gas tensions. Anaesthesia 1972; 27:258-264 [Context Link] 20. Connors AF Jr, Hammon WE, Martin RJ, et al: Chest physical therapy. The immediate effect on oxygenation in acutely ill patients. Chest 1980; 78:559-564 Bibliographic Links [Context Link] 21. Tyler ML, Hudson LD, Grose BL, et al: Prediction of oxygenation during chest physiotherapy in critically ill patients. Am Rev Respir Dis 1980; 121:218A [Context Link] 22. Mackenzie CF, Shin B, McAslan TC: Chest physiotherapy: The effect on arterial oxygenation. Anesth Analg 1978; 57:28-30 Ovid Full Text Request Permissions Bibliographic Links [Context Link] 23. Mackenzie CF, Shin B: Cardiorespiratory function before and after chest physiotherapy in mechanically ventilated patients with post-traumatic respiratory failure. Crit Care Med 1985; 13:483486 Request Permissions Full Text Bibliographic Links [Context Link] 24. Weissman C, Kemper M: The oxygen uptake: Oxygen delivery relationship during ICU interventions. Chest 1991; 99:430-435 Bibliographic Links [Context Link] 25. Weissman C, Kemper M, Harding J: Response of critically ill patients to increased oxygen demand: Hemodynamic subsets. Crit Care Med 1994; 22:1809-1816 Request Permissions Bibliographic Links [Context Link] 26. Horiuchi K, Jordan D, Cohen D, et al: Insights into the increased oxygen demand during chest physiotherapy. Crit Care Med 1997; 25:1347-1351 Ovid Full Text Request Permissions Full Text Bibliographic Links [Context Link] 27. MacLean D, Drummond G, Macpherson C, et al: Maximum expiratory airflow during chest physiotherapy on ventilated patients before and after the application of an abdominal binder. Intensive Care Med 1989; 15:396-399 Bibliographic Links [Context Link] 28. Weissman C, Kemper M, Damask MC: Effect of routine intensive care interactions on metabolic rate. Chest 1984; 86:815-818 Bibliographic Links [Context Link] 29. Klein P, Kemper M, Weissman C, et al: Attenuation of the hemodynamic responses to chest physical therapy. Chest 1988; 93:38-42 Bibliographic Links [Context Link] 30. Zidulka A, Chrome JF, Wight DW, et al: Clapping or percussion causes atelectasis in dogs and influences gas exchange. J Appl Physiol 1989; 66:2833-2838 [Context Link] 31. Venkataraman ST, Orr RA: Mechanical ventilation and respiratory care. In: Pediatric Critical Care. Fuhrman BP, Zimmerman JJ (Eds). St. Louis, CV Mosby, 1992, pp 519-543 [Context Link] 32. Allen JL, Sivan Y: Measurements of chest wall function. In: Infant Respiratory Function Testing. Stocks J, Sly PD, Tepper RS, et al. (Eds). New York, John Wiley & Sons, 1996, pp 329-354 [Context Link] 33. Vandenplas Y, Diericx A, Blecker U, et al: Esophageal pH monitoring data during chest physiotherapy. J Pediatr Gastroenterol Nutr 1991; 13:23-26 Request Permissions Buy Now Bibliographic Links [Context Link] 34. Emery JR, Peabody JL: Head position affects intracranial pressure in newborn infants. J Pediatr 1983; 103:950-953 Full Text Bibliographic Links [Context Link] 35. Perlman JM, Volpe JJ: Suctioning in the preterm infant: Effects on cerebral blood flow velocity, intracranial pressure, and arterial blood pressure. Pediatrics 1983; 72:329-334 Bibliographic Links [Context Link] 36. Ersson U, Carlson H, Mellström A, et al: Observations on intracranial dynamics during respiratory physiotherapy in unconscious neurosurgical patients. Acta Anaesthesiol Scand 1990; 34:99-103 Bibliographic Links [Context Link] 37. Raval D, Yeh TF, Mora A, et al: Chest physiotherapy in preterm infants with RDS in the first 24 hours of life. J Perinatol 1987; 7:301-304 Bibliographic Links [Context Link] 38. McCulloch KM, Ji SA, Raju TNK: Skin blood flow changes during routine nursery procedures. Early Hum Dev 1995; 41:147-156 Full Text Bibliographic Links [Context Link] 39. Bloomfield FH, Teele RL, Voss M, et al: The role of neonatal chest physiotherapy in preventing postextubation atelectasis. J Pediatr 1998; 133:269-271 Full Text Bibliographic Links [Context Link] Key Words: chest physiotherapy; mechanical ventilatory support; children; vital signs; closing capacity; chest wall compliance; suctioning; oxygen consumption; cardiac output; intracranial pressure