Parents as providers - Skin to Skin Contact
advertisement

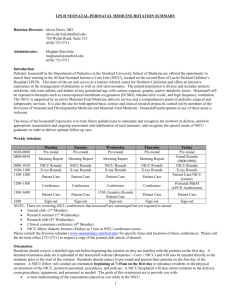
Parents as Primary Providers 4/11/2010 & 2/8/2014 Also called “co-care’, family integrated care, family centered care, etc. Bergman & Bergman 2013 FT, speaks to parents as providers on mother/baby unit Flacking, 2013 PT, analysis of relationship between parenting in a “co-care” environment, duration of KC and level of maternal stress. Maternal stress lower in the 2 co-care units as compared to the two non co-care units. Duration of KC was not related to level of maternal stress. Fraser, D. 2013 PT, editors note in Neonatal Network 32(2), 87-88 and on page 87 she says “integrated care by parent” is a future we face in NICU. Harrison 2010 FT, Case study of congenital heart defect baby and mom who did kc for 80+ mins /day X 14 days. Mom said she like KC because she felt like she was helping her infant and being a mom. Heinemann et al. 2013 PT, qualitative study identifies the advantages and barriers as perceived by parents of staying with infants overnight in NICU. KMC helps parents feel in control and feel needed, both of which increase their presence in NICU. Low staffing levels decrease KMC when they have to wait for transfer help Hendricks-Munoz et al., 2013Kangaroo Care through the day and night is elemental component and the more KC mothers do, the more they want to be primary care providers. 61% of Black mothers NOT told about KC vs 39% of white mothers foreign born nurses implement KC more than US born nurses. 63% of mothers believed "KMC should be provided daily" 90% of mothers compared with 40% of nurses strongly believed "mothers should be partners in care Ludington-Hoe 2010 Review. Says KC is start of paradigm shift to parents as primary providers OR is this In the 30 year article of 2011? Ludington-Hoe, 2013 Review in NAINR that mentions Parents as Primary Providers Ludington-Hoe & Morgan Review for March of Dimes talks about parents as primary providers to date (Sept. 2013) 2013 Lyngstad et al. 2014 PT, R cross over of diaper change in incubator with mom present one day and other day diaper change in KC. HR, SaO2, stress (skin conductance) showed diaper change is stressful and much less stress in KC diaper change. Need to consider the FABRIZI WORK. Nyqvist & Engvall, 2009 Qualitative study of 43 parents, 85 nurses who completed survey and 14 RNs and 4 neonatologists who completed 4 focus groups. Considerable differences were found between parent and professional responses about parent participation in infant care. All listed activities were marked as “optional” by parents, agreement was reached about parents as primary caregivers based on individual assessment of parent’s willingness and ability, with nurses acting as educators and supporters instead of caregivers. Nyqvist,K.H., Engvall, G. (2009). Parents as their infant’s primary caregivers in a neonatal intensive care unit. J Pediatr Nurs 24(2): 153-163. Pallas et al., 2012 Survey of European NICUs and how much they let parents participate in care,what they are allowed to do and how much KC they can do and under what restrictions, frequency, etc. Suczs & Roseman, 2013 PT?? FT?? Describes using KC for phototherapy to continue providing evidence -based family centered therapy. Turnbull & Petty 2013 Westrup, B. 2004 Wiger et al., 2008. PT, Review. Says that Family centered NICU care should allow 24/7 gentle touch and skin to skin contact. See citation in Bergman and Bergman, 2013, but this is seminal work and idea. Aim of this observation and interview study was to learn what facilitates and what obstructs parent participation in their child’s care in the NICU. Management and staff had good ambitions to promote parent participation, but the care, including the conditions for parental participation, was driven by terms of the staff, routines focusing on medicaltechnical care and environment and budgetary constraints instead of the value of parent participation. This is an excellent article. Wiger, H., Hellstrom, A-L, Berg, M. (2008). Conditions for parents’ participating in the care of their child in neonatal intensive care- a field study. Neonatal Intensive Care 21(3): 30-36. Family-Integrated CARE Bracht, M., O’Leary L, Lee SK, and O’Brien K. (2013, Apr). Implementing family integrated care in the NICU: a parent education and support program. Advances in Neonatal Care, 13(2), 115-126. Purpose was to design, develop, implement and evaluate a parent education and support program that enhances family integrated care in NICU. Effectiveness of program evaluated through anecdotal feedback and formal evaluation process at discharge. Mothers were provided with the tools to parent their infants in NICU, recognize their own strengths, increase their problem solving abilities/strategies, and emotionally prepare them to take their infant home. Galarza-Winton, M.E., Dicky, T., O’Leary L, Lee SK, O’Brien, K. (2013, Oct). Implementing family-integrated care in the NICU: educating nurses. Advances in Neonatal Care, 13(5), 335-340. They designed an educational program and then interviewed nurses 6 months after it and learned that nurse related that the education was valuable and that the information on nursing vs parental responsibilities in infant care, the parent experience in the NICU, and developmental care strategies werethe most useful. They need on-going staff mentoring to maximize their ability to facilitate family integrated care. SPECIFIC EDUCATION FOR NURSES FACILITATES FAMILY-integrated care in the NICU Macdonnell K., Christie K, Robson K, Pytlik K, Lee SK, O’Brien,K. (2013-Aug). Implementing family -intergrated care in the NICUI: engaging veteran parents in program design and delivery. Advances in Neonatal Care, 13(4): 262-269. Veteran parents contributed to the development of the program and in the provision of peer-to-peer support . Engagement of parents with prior experience in the NICU care environment is a critical step in the design and implementation of family-integrated care. Single family rooms may not be so good: Pineda RG, Neil J. Dierker D, Smyser CD, Wallendorf M, Kidokoro H, REynotls LC, Walker S, Rogers C, Mathur AM, Van Essen DC, Inder T. (2014-Jan). Alterations in brain structure and neurodevlopmental outcome in preterm infants hospitalized in different neonatal intensive care unit environments. J. Pediatrics 164(1), 52-60. Infants in private rooms were characterized by a diminution of normal hemispheric asymmetry and a trend towards having lower amplitude EEG cerebral maturation scores. AT age 2 infants in private rooms had lower language scores, and a trend toward lower motor scores which persisted after adjustment for potential confounders (CRIB – critical risk index for babies & BAyley III.)