Furtado - POSTERIOR VITREOUS DETACHMENT
advertisement

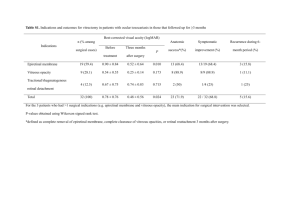
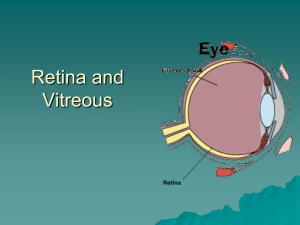
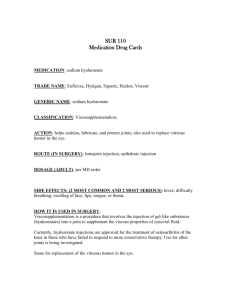
WHEN A PVD IS NOT 'JUST A PVD': POSTERIOR VITREOUS DETACHMENT AND ITS POTENTIAL FOR OCULAR PATHOLOGY Nadine M. Furtado, OD, MSc, FAAO A. Anatomy & Biochemistry of the Vitreous 1) The vitreous is a semi-solid, gel-like structure i. Consists mainly of water (98-99% of total vitreous volume) ii. Three-dimensional arrangement of structural molecules, i.e. collagen and hyaluronic acid, allow for stability of the semi-solid framework 2) Structure of the vitreous body i. Central vitreous – occupies majority of the vitreous body with low collagen concentration ii. Vitreous cortex – thin external layer with high collagen concentration 3) The vitreoretinal interface i. Posterior vitreous cortex & inner layer of the retina are bound together by a macromolecular attachment complex composed of fibronectin & laminin ii. Areas of firm adhesion between the vitreous and the inner retina are seen at locations on the retina where the inner limiting membrane (ILM) is thin, namely the vitreous base, optic disc and macula B. Posterior Vitreous Detachment (PVD) 1) Normal, age-related event defined as the separation of the posterior vitreous cortex from the inner limiting membrane of the retina i. Observed in at least 65% of individuals 65 years of age 2) The vitreous undergoes numerous changes as it ages i. Syneresis is the condensing of collagen into parallel fibrils ii. Synchysis (liquefaction) is the creation of liquefied pockets (lacunae) within the vitreous caused by hyaluronic acid dissociating from collagen fibres a) Increase in the number, size and coalescing of lacunae leads to progressive liquefaction of the vitreous body 3) Stages of a posterior vitreous detachment (Johnson, 2010) i. Stage 0 – No PVD ii. Stage 1 – Perifoveal PVD; vitreous remains attached at the optic disc and midperipheral retina iii. Stage 2 – Macular PVD with no foveal attachment; vitreous remains attached at the optic disc and ________midperipheral retina iv. Stage 3 – Near complete PVD; vitreous remains attached only at the optic disc (possible adhesion ________may still be present at the vitreous base) v. Stage 4 – Complete PVD evidenced by total separation of the vitreous from the retina C. Anomalous Posterior Vitreous Detachment 1) Vitreous liquefaction & weakening of vitreoretinal adhesions must occur simultaneously for a PVD to occur without sequela 2) Vitreous liquefaction in excess of the amount of vitreoretinal dehiscence results in an anomalous PVD 3) The development of an anomalous detachment of the posterior vitreous usually occurs at the sites of strongest vitreoretinal adhesion, and leads to a variety of ocular pathologies i. Traction at the vitreous base can lead to the development of a retinal hole or tear, which has the potential to progress to a rhegmatogenous retinal detachment ii. Vitreopapillary traction occurring at the optic nerve has the ability to cause a vitreous hemorrhage iii. Anomalous PVD at the macula can lead to vitreomacular traction syndrome (see bullet point D) D. Vitreomacular Traction (VMT) Syndrome 1) Vitreomacular Adhesion (VMA) - Perifoveal vitreous adheres to the macula after detaching from the surrounding retina; usually asymptomatic 2) Vitreomacular Traction (VMT) – Vitreous traction forces cause an anatomical disruption of the foveal architecture; always symptomatic (VA and/or metamorphopsia) 06/06/2014 3) Anomalous PVD can lead to various maculopathies i. Focal VMA a) Chronic focal VMA can progress to VMT b) Early VMT can either spontaneously resolve, following a complete PVD, or progress as evidenced by increasing retinal thickening and formation of intraretinal cystic spaces c) VMT can further advance to the development of a full-thickness macular hole (involves all retinal layers) Operculated holes should be properly assessed to ensure complete detachment of the operculum (ensure no adhesion and/or traction) Presence of focal VMA on an operculated hole can only be conclusively determined by ensuring that multiple OCT scans are analyzed, of which at least two are at perpendicular angles ii. Concomitant Disease a) Increased occurrence of an incomplete PVD in association with neovascular AMD & diabetic retinopathy, suggesting a possible role of VMT in the progression of these diseases iii. Foveal Retinoschisis a) VMA that occurs over a broad area can lead to retinal thickening and a schisis-like separation of the internal retinal layers b) This thickening can lead to the formation of intraretinal cysts; they are usually contained within the retina and do not disrupt the ILM c) Persistent force and traction can cause dehiscence of the ILM from the underlying retina, resulting in a lamellar hole (partial-thickness hole not extending through all layers of the retina) iv. Epiretinal Membrane (ERM) a) Vitreous cortex remnants on inner retina possibly play a role in promoting cellular proliferation and the subsequent development of an ERM b) An ERM can adhere to the ILM and cause retinal thickening / edema c) Tractional forces can cause inward pulling of the underlying retina and lead to a macular pucker, at which point patients are usually symptomatic (↓VA and/or metamorphopsia) E. Pharmacologic Vitreolysis 1) Defined as the use of a pharmacologic agent to induce separation of the posterior vitreous from the inner retina 2) Ocriplasmin i. Recently approved for pharmacologic vitreolysis via intravitreal injection ii. Contains proteolytic activity against fibronectin & laminin, the molecules which allow the vitreous to adhere to the inner retina 3) MIVI-TRUST Study (Microplasmin for Intravitreous Injection – Traction Release without Surgical Treatment) i. Objective was to investigate enzymatic vitreolysis of vitreomacular adhesion with ocriplasmin ii. Intravitreal injection of ocriplasmin resolved VMT and closed macular holes in significantly more participants when compared to injection of a placebo Selected References Benz MS, Packo KH, Gonzalez V, et al. A Placebo-Controlled Trial of Microplasmin Injection to Facilitate Posterior Vitreous Detachment before Vitectomy. Ophthalmol 2010;117:791-97. De Smet MD, Gad Elkareem AM, Zwinderman A H. The vitreous, the retinal interface in ocular health and disease. Ophthalmologica 2013; 230(4):165-78. De Smet MD, Gandorfer A, Stamans, et al. Microplasmin Intravitreal Administration in Patients with Viteomacular Traction Scheduled for Vitrectomy (The MIVI I Trial). Ophthalmol 2009; 116(7):1349-55. Duker JS, Kaiser PK, Binder S, et al. The international vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmol 2013;120(12):2611-19. Johnson MW. Posterior vitreous detachment: evolution and complications of its early stages. Am J Ophthalmol 2010;149(3):371-82. Sebag J. Anomalous posterior vitreous detachment: a unifying concept in vitreo-retinal disease. Graefes Arch Clin Exp Ophthalmol 2004;242(8):690-8. Stalmans P, Benz MS, Gandorfer A, et al. Enzymatic vitreolysis with ocriplasmin for vitreomacular traction and macular holes. New Engl J Med 2010;367(7):606-15. Stalmans P, Delaey C, de Smet MD, e al. Intravitreal injection of microplasmin for treatment of vitreomacular adhesion: results of a prospective, randomized, sham-controlled phase II trial (The MIVI-IIT trial). Retina 2010; 30(7):1122-7. Stalmans P, Duker JS, Kaiser P, et al. OCT-based interpretation of the vitreomacular interface and indications for pharmacologic vitreolysis. Retina 2013;33(10):2003-11. 06/06/2014