Gta – Draft – 03 - University of Illinois
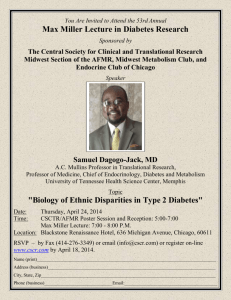
advertisement

September 14, 2007 TO: Mark Schneiderhan, Chair Senate Committee on Educational Policy FROM: Margaret Grosch Director, Programs and Academic Assessment I am submitting for review and action by the Graduate College Executive Committee the attached Proposal to Establish the Master of Science in Clinical and Translational Science. This proposed program was approved by the School of Public Health Committee on Educational Programs on December 17, 2006 and by the School of Public Health Executive Committee on January 8, 2007. This proposal was approved by the Graduate College Executive Committee on September 7, 2007. Below are additional comments relayed to you at the request of the Graduate College Executive Committee (GCEC). The proposal for an MS in Clinical Translational Science presented by SPH was approved by a vote of 5-1-1. A broad majority expressed strong support for the purpose and concept of the proposal came from all disciplinary divisions. Some committee members felt that the complex nature of the proposal made it difficult to grasp. A minority expressed skepticism about whether the proposed program could indeed bridge the distance between research and clinical practice, even with the addition of a new GCLS 512 course on the Logic of Experimental Biology. Arguing against this point of view were several basic scientists who acknowledged that traditionally the research mindset fully develops only over a number of years, but the creation of the new course was a first attempt to accelerate this process. Further, the new course will be taken not only by the Clinical Translational MS students, but will be available to incoming students in the Graduate Education in Medical Sciences during their first and second years, in the hope that will expedite their development as bench scientists. Clearly it was the opinion of the GCEC that the proposal was significantly improved, and represents a valuable experiment in addressing the difficulties of combining clinical and basic science perspectives into a single research degree. Attachment Cc: J. Zwanziger B. Neuberger L. Sandlow C. Hulse Revised 2/17/2016 1 Internal Approval Routing Form August, 2006 Title of Program/Center: Master of Science in Clinical and Translational Science 1. Review and Approval by Department X Date: 3/19/07 2. Review and Approval by College X Date: 1/8/07 3. Analysis of Needed Resources by Academic Affairs: Adequacy, □ Date: _______ Appropriateness, Availability 4. If Program is Graduate, Review by Graduate College Executive Committee X Date: 9/7/07 5. Review by Senate Committee on Educational Policy X Date: 9/19/07 6. Final Review by Academic Affairs for Academic and Fiscal Soundness □ Date:_______ Comments: Revised 2/17/2016 2 REQUEST FOR A NEW UNIT OF INSTRUCTION BACKGROUND 1. Name of Institution: University of Illinois at Chicago 2. Title of Proposed Program: Master of Science in Clinical and Translational Science 3. Contact Person: Charles Evans 3.1. Telephone: 217-333-3079 3.2. Email: cevans4@uillinois.edu 3.3. Fax: 217-244-5763 4. Level of Proposed Unit __ Undergraduate Certificate (1-2 years) Certificate __ Undergraduate Certificate (2-4 years) __ Associate __ Post-Baccalaureate __ Post-Master’s Certificate __ First Professional Certificate __ Baccalaureate X_ Masters __ First Professional __ Doctorate1 5. Requested CIP Code (6-digits) __To be assigned_______ 6. Proposed Date for Enrollment of First Class: August 2008 7. Location Offered2: On-Campus _X__ Off-Campus ___: Region Number(s)______ or Statewide___ 1 To assist staff in specialized areas of instruction, IBHE will retain two outside consultants to review all new doctoral program proposals. 2 Institutions may request approval to offer a program, simultaneously, on- and off-campus, including statewide. However, assessments of program objectives and outcomes should be developed that address all of the locations and modes of delivery for which the institution is seeking approval. Note that “on-campus” approval extends to the entire region in which the main campus is located. New off-campus programs to be offered outside the institution’s region require approval. Revised 2/17/2016 3 MISSION, OBJECTIVES AND PRIORITIES 8. Mission 8.1. Describe specific objectives and measurable contributions the program will make to the university’s mission, paying particular attention to the program’s consistency with the university’s focus statement and priorities. Such objectives and contributions may include: serving a distinct student population; occupational and student demand for the program; collaborating with and/or supporting other programs at the institution; meeting the needs of business, employers, and/or society; and increasing the number of graduates in a high demand or emerging field of study. Summary of Program The development of the proposed Master of Science in Clinical and Translational Science is part of the NIH funded Clinical Research Training Program (CRTP) and is intended to train clinicians, primarily post-doctoral or post-residency fellows and junior faculty, to become leaders in clinical research. The MS would draw clinically-trained students from across UIC as well as clinicians from collaborating institutions into an interdisciplinary degree program that aims to help build the clinical research community in Chicago. There exists widespread consensus in the biomedical research community that there is currently a shortage of qualified researchers and mentors in clinical research. There is a growing need for skilled clinical investigators to apply accelerating advances in basic science and biotechnology to clinical practice, “ from the bench to the bedside” as well as to translate clinical science into practice, “from study to practice” so that these advances improve population health. Through didactic coursework, a series of workshops and seminars, and a mentored research project, the MS in Clinical and Translational Science will help develop a new generation of skilled clinician-investigators focused on improving patient health through research. Graduates of the MS program will understand the basic analytical tools used by biostatisticians and epidemiologists, supplemented by a broad array of relevant electives that will provide the basic concepts and theories consistent with each student’s goals and objectives. They will be able to communicate their insights effectively, write wellconceived and persuasive grant applications and ensure the ethical treatment of their subjects. Finally, as apprentice clinical investigators, they will learn how to participate in a broader multidisciplinary research community that includes basic and social scientists, as well as clinicians from other areas of clinical practice. Graduates of the MS in Clinical and Translational Science will have the skills to direct a broad range of Revised 2/17/2016 4 clinical studies, including the translation of scientific knowledge into clinical practice, and will be able to interact effectively with all of the complementary disciplines with which clinical investigators need to collaborate. National and Local Demand for Leaders in Clinical and Translational Research The National Institutes of Health (NIH) 2002 Roadmap for Medical Research called for a “re-engineering” of clinical research, recognizing the urgent need for trained researchers in the fields of clinical and translational science and the importance of supportive and accessible institutional environments to attract and retain skilled researchers. Despite the obvious value and complexity of clinical research, there have been, until recently, few well-defined training programs for clinical investigators. Addressing the future of clinical research and ensuring a sufficient pool of adequately prepared clinical researchers has been identified as a priority not only by the NIH, but also the Institute of Medicine and the Association of American Medical Colleges. In conjunction with the 2002 Roadmap, the NIH recently issued a Request for Applications for the Institutional Clinical and Translational Science Award (CTSA). Through this award, institutions are expected to improve clinical research across disciplines. Its scope is defined as follows: “The purpose of this initiative is to assist institutions to forge a uniquely transformative, novel, and integrative academic home for Clinical and Translational Science that has the consolidated resources to: 1) captivate, advance, and nurture a cadre of well-trained multi- and inter-disciplinary investigators and research teams; 2) create an incubator for innovative research tools and information technologies; and 3) synergize multidisciplinary and inter-disciplinary clinical and translational research and researchers to catalyze the application of new knowledge and techniques to clinical practice at the front lines of patient care” (NIH Institutional Clinical and Translational Science Award RFA-RM-06-002). In September 2006, UIC was notified by the NIH that the program’s application for a CTSA planning grant had been accepted. The proposed MS in Clinical and Translational Science is a vital part of this funded initiative to build clinical research capacity at UIC and is an integral part of competing for further CTSA funding. The NIH Roadmap for Medical Research identifies the crucial areas of clinical and translational research as being burdened by growing barriers between clinical and basic research, regulatory obligations, increases in the cost and complexity of conducting research, and lack of resources. With basic researchers making enormous progress in the biological and other natural and social sciences, skilled clinical investigators are needed now more than ever to translate that knowledge into deliverable applications for human health. The Institute of Medicine’s Clinical Research Roundtable addressed this concern Revised 2/17/2016 5 in their 2001 Roundtable Report, stating that “…clinical advances will not emerge from today’s science without trained clinical investigators, and an adequate supply of these investigators will be needed to take advantage of the wealth of data being generated by basic science laboratories around the world” (Developing the Clinical Investigator Workforce: Clinical Research Roundtable Symposium 1). Clinical researchers work in a variety of settings including private industries, academic centers, and government agencies. Demand is expected to rapidly increase over the coming years, contributing to concerns that there will be a shortage of skilled researchers to fill these positions (See Section 8.4 for more information on employment projections). Apart from institutional barriers that discourage researchers from entering the field, there are additional factors contributing to high demand. The average age of clinical researchers is rising, and there are not enough young researchers to fill these positions. In addition, advances in biotechnology and the pharmaceutical industry require welltrained researchers to conduct thorough and high quality clinical trials prior to introducing a product into the marketplace and to monitor its subsequent performance. Funding for clinical research is also expected to rise; the NIH alone has committed to allocating approximately one third of its budget to clinical and translational research and training programs. New training programs are needed in order to ensure that the field of clinical and translational research grows rather than diminishes over the next generation. The proposed MS in Clinical and Translational Science helps fill the growing demand for highly trained clinical investigators. UIC Demand for Clinical and Translational Research The University of Illinois at Chicago is the largest public research university in the city of Chicago, and institutional emphasis on research is steadily growing: between 1998 and 2005, research expenditures increased from $96.8 million to $237 million, an increase of 145%. UIC is one of only six academic centers in the country that hosts a full complement of health science colleges (Medicine, Pharmacy, Nursing, Public Health, Dentistry, and Applied Health Sciences) enabling it to fulfill its mission. This breadth provides an advantage to the university to be at the forefront not only of research, but research education as well. In response to the NIH Roadmap initiative and growing concern over a looming shortage of clinical researchers, the Provost charged the Deans of the UIC Health Sciences colleges with the task of developing a university-wide plan to encourage and support the growth of clinical and translational science. The Council of Health Science Deans has endorsed the approach proposed in the planning grant including the development of an MS program in Clinical translational Science. More broadly, the program follows from a key component of UIC’s mission (see http://www.uic.edu/homeindex/admin_scope.shtml): Revised 2/17/2016 6 To train professionals in a wide range of public service disciplines, serving Illinois as the principal educator of health science professionals and as a major healthcare provider to underserved communities. The NIH Roadmap outlines nine central functions that institutions must serve in working toward the goal of transforming clinical and translational research, and one of these key areas is research education, training, and career development. The proposed MS in Clinical and Translational Science, associated with an extensive Translational Research Seminar Series (see 2006-2007 seminar schedule in Section 9.3), directly respond to this educational component as mandated by the NIH by building the educational infrastructure at UIC and increasing clinical research competence. Appropriately trained clinical and translational researchers will become increasingly critical to the continued growth of UIC, especially with increased NIH funding for clinical and translational research and training programs. The University of Illinois at Chicago does not currently offer a distinct Masters level degree specifically designed to provide clinicians across all six health science colleges with a broadly defined set of clinical and translational research skills. As part of the NIH funded Clinical Research Training Program, the MS in Clinical and Translational Science will fill this gap by appealing to professionals in each of the health science colleges. The goal of the CRTP is to train clinicians, primarily post-doctoral or post-residency fellows and junior faculty, to become skilled practitioners in clinical research, thereby providing opportunities for talented clinicians who have had limited research training to pursue academic research careers. As shown in Table 1 below, the proposed Masters program is a central part of the framework of educational programs geared towards increasing clinical research training at UIC, as well as constituting an important part of the university-wide response to the NIH Roadmap. Revised 2/17/2016 7 Table 1 An Overview of Clinical Translational Science (CTS) Education Programs Honors Intensive College Program Course Undergraduates X X Pre-doctorate X clinicians Pre-doctorate X PhD students M(D)STP fellows Clinicians in residency and X fellowship Junior faculty X Clinicians in affiliated X institutions Clinicians in communityX based settings Certificate MS Workshops Seminar in Series CTS X X X X X X X X X X X X X X X X X X X X X X X X X Interdisciplinary Collaboration Clinical research must be interdisciplinary in order to yield significant translational results. With this reality in mind, the MS in Clinical and Translational Science has been designed with input from representatives across the six health science colleges (Public Health, Medicine, Pharmacy, Nursing, Dentistry, and Applied Health Sciences). Core courses in the MS curriculum will be offered by the School of Public Health and the College of Medicine; electives will be chosen from a variety of coursework offered by colleges across the university (see Section 9 for more information on required and elective coursework). Administration The MS degree will be administered by the Division of Health Policy and Administration in the School of Public Health, similar to the structure of corresponding programs at Johns Hopkins University, Columbia University, University of Kansas, University of Alabama at Birmingham, and University of Washington. It would replace the current Master of Public Health Science Concentration in Clinical Research. Policy direction for the CTSA program in general, as well as for the education and training component, will be provided by a Policy Advisory Committee to represent the Health Science Colleges, the Medical Center and other collaborating entities. Revised 2/17/2016 8 8.2. Explain how the program will meet regional and state needs and priorities, making specific reference to The Illinois Commitment. Three of the goals of The Illinois Commitment (goals 1, 4 and 5) are of particular relevance to the proposed program. Goal 1. Higher education will help Illinois business and industry sustain strong economic growth. Goal 4. Illinois will increase the number and diversity of citizens completing training and education programs. Goal 5. Illinois colleges and universities will be accountable for providing high quality academic programs and systematic assessment of student learning outcomes while holding students to ever higher expectations for learning and growth. Goal 1 Higher education will help Illinois business and industry sustain strong economic growth. As discussed earlier, the clinical research enterprise is at a crossroads – basic science research is making tremendous progress, but there are widespread concerns that there are not enough skilled clinical investigators to translate basic research breakthroughs into practical applications that will benefit the health of the US population. As the Illinois Commitment states, “The benefits of research need to be brought swiftly to business and industry, to school classrooms, and to patients’ bedsides.” In agreement with this goal, the MS in Clinical and Translational Science is designed to answer this call. Highly skilled clinical and translational researchers are needed in both academic and industry settings. For universities, NIH, the primary source of academic research funding, is committed to shifting a larger portion of its research budget to support clinical and translational research. Universities will need to increase the number of skilled clinical and translational investigators to sustain a growing research program. In addition, clinical and translational researchers will be able to access other sources of research support, particularly from companies that produce pharmaceuticals and medical devices, for studies that apply basic science knowledge to the treatment and diagnosis of disease. The biotechnology and pharmaceutical industries are robust and growing fields in Illinois, and the program can expect them to continue growing as the Baby Boomers age and require more medical care. Illinois is home to two large health care companies, Baxter and Abbott (see Section 8.4 for details), and the program can expect that some graduates of the MS program will find work in these corporations. According to the Illinois Department of Employment Security, Economic Information and Analysis Division, the need for medical scientists and biological scientists in the state is expected to increase by 22% and 25%, respectively, by the year 2012. There is clearly a need for skilled clinician-investigators, and the UIC MS program in Clinical and Translational Science will help Illinois sustain economic and scientific growth in the biotechnology industry, Revised 2/17/2016 9 while also providing trained scientists to further medical research and progress for all citizens. Goal 4 Illinois will increase the number and diversity of citizens completing training and education programs. This program will be open to clinicians across the six health science colleges at the University of Illinois at Chicago, as well as clinicians from neighboring institutions, such as collaborating institutions like the Jesse Brown VA Medical Center. The Recruitment and Admissions Committee has targeted its outreach to those historically underrepresented in research positions, including minorities and women. Over 23 percent of UIC’s student population belongs to disadvantaged minorities, and in five of the six UIC health sciences colleges where the program plans to recruit, there are approximately 400 potential trainees, 18% of whom are under-represented minorities. In addition, the program intends to make the MS accessible to a wide variety of students by scheduling classes at times that could be incorporated into work schedules and by using online modes of delivery for 30-50 percent of the courses required for the degree. Goal 5 Illinois colleges and universities will be accountable for providing high quality academic programs and systematic assessment of student learning outcomes while holding students to ever higher expectations for learning and growth. This program has been specifically designed to meet the needs of students with diverse interests, and will hold students to high expectations for learning and growth. The program’s goal is to provide students with the knowledge and skills necessary to succeed in a dynamic and competitive field. UIC prides itself on not only providing an excellent educational environment for its students and faculty, but also on being responsive to social, student, and workforce needs. The MS in Clinical and Translational Science is a direct response to a NIH initiative calling for a transformation of clinical research and increased educational opportunities for clinical research training. The MS Evaluation Plan (see Section 13) will monitor both immediate and long-term learning outcomes to ensure that students in this program are receiving the best possible education. 8.3. Identify similar programs and sponsoring institutions in the state. Compare these programs with the proposed program. Discuss the possible impact of the proposed program on these programs. Other programs: Impact, competition, resources, uniqueness The following Illinois institutions also offer programs with an emphasis on Clinical Research: (1) Northwestern University – MS in Clinical Investigation; (2) University of Chicago – MS in Health Studies; (3) Rush University – MS in Clinical Research; and (4) Revised 2/17/2016 10 Loyola University – MS in Clinical Research Methods. The tuition costs for these programs is summarized below. Institution Tuition Notes Northwestern University Feinberg School of Medicine MS in Clinical Investigation ($3,963/unit)(10 units)=$39,630 NW employees have a tuition benefit – up to 75% of tuition fees are waived University of Chicago MS in Health Studies for Clinical Professionals ($3,698/course)(9 courses)=$33,282 Fellows or house staff pay 50% of tuition; there are some scholarships, and some students pay through K-awards Rush University MS in Clinical Research Loyola MS in Clinical Research Methods $2,500/year for Rush/Stroger employees. Non-employees: ($2,592/quarter)(8 quarters or 2 years) = $20,736 ~$17,000 to complete the program (24 credit hours) Special fee for Rush and Stroger employees Free for Loyola employees, most trainees are residents or fellows The proposed program at UIC would have the following distinguishing characteristics: (1) The tuition for the proposed MS program is substantially lower (on a per course basis) and is comparable to Loyola’s overall. Faculty and staff at UIC may complete the program free of charge, a benefit unavailable through any other institution. (2) The proposed program offers a broad knowledge base from across UIC, allowing for students to customize a plan of study tailored to their unique skills, interests, background and objectives. Since all of these programs are largely internally oriented, as is the proposed UIC MS program in Clinical and Translational Science, the program does not expect it to have a significant impact on the previously listed programs. The University of Chicago MS currently has 13 students enrolled, 10 of whom are U of C faculty. On average, Northwestern admits 20-30 students into the MS program each year, a majority of whom are NW faculty, junior faculty, or fellows. Rush currently has 11 students enrolled, the vast majority of whom are from Rush or Cook County Stroger Hospital. The proposed MS in Clinical and Translational Research may attract a few non-UIC applicants because it has lower fees and greater flexibility, but such students are likely to be a small minority of the total enrollment in the program. Revised 2/17/2016 11 8.4. Discuss estimated future employment opportunities for graduates of this program. Compare the estimated need for graduates with the estimated number of graduates from this program and existing programs identified in 8.3 above. Where appropriate, provide documentation by citing data from such sources as employer surveys, current labor market analyses, and future workforce projections. Describe any special need for this program expressed by state agencies, industry, research centers, or other educational institutions. Future Employment Opportunities Students in the MS program will primarily be associated with UIC or a collaborating institution. Home departments will be required to commit themselves to support the students while they are in the MS program (see Section 9.1 below). In most cases, students are expected to remain with their departments after graduation, with support during the tenure in the MS program viewed as a skill-enhancing investment which will increase students’ value by enabling them to mount competitive research programs. From a national and/or regional perspective, there will be demand for program graduates both from other academic centers and from the research and development teams of pharmaceutical and medical device manufacturers. There is increasingly strong demand to apply biological research and breakthroughs to advances in clinical care – in other words, to translate knowledge from the “bench to the bedside”. The clinical and translational research enterprise will need individuals with specialized training that builds on their clinical training but also provides them with the basic research skills they will need to conduct clinical and translational research in a multidisciplinary environment. The demand for clinical research in academic centers is also partially due to increased funding in this area by agencies such as the NIH, which has committed to allocating approximately one third of its budget to support clinical and translational research. Clinical investigators are also needed in the for-profit sector for drug discovery and technology transfer initiatives of private industry. The growth of the biotechnology industry has meant the creation of new drug treatments, but there are concerns that there are not enough clinical researchers to run the necessary clinical trials. The greater Chicago area is home to several large companies that rely on skilled medical researchers. Abbott Park, a north suburb of Chicago, is home to the U.S. Corporate Headquarters of Abbott Laboratories, an international health care company that manufactures pharmaceutical, medical, and nutritional products. Abbott employs approximately 65,000 people worldwide, and one of their four US medical research centers is also located in northern Chicago. Another global healthcare company, Baxter International Inc., is based in Deerfield, Illinois and manufactures pharmaceuticals, medical devices, and biotechnology products. Pharmaceutical and biotechnology companies constitute an enormous and growing international industry – Baxter and Abbott alone employ well over 100,000 employees and 2005 sales for the two companies reached $32.1 billion. Growth Projections Revised 2/17/2016 12 Clinical and translational research is a component of a growing employment area. According to the U.S. Department of Labor’s 2006-2007 Occupational Outlook Handbook, the job market for both biological and medical scientists is growing; the “expected expansion of research related to health issues such as AIDS, cancer, and Alzheimer’s disease also should create more jobs for these scientists” (U.S. Department of Labor, Bureau of Labor Statistics, Occupational Outlook Handbook). The Department of Labor also predicts that employment of medical scientists will “grow much faster than average for all occupations through 2014.” The Illinois Department of Employment Security, Economic Information & Analysis Division echoes these national predictions: employment projections for the state of Illinois show increasing job opportunities for trained scientists across all categories. Biochemists and medical scientists, for example, can expect employment opportunities to increase by 22% and 25%, respectively, by the year 2012 (see Figure 3). Because this Masters program provides an opportunity for students to self-design a program of elective study, graduates will be able to fill these new positions in areas along the full spectrum of biological to applied science. Table 2. Illinois Employment Projections State of Illinois Occupational Employment Projections 2002-2012 Base Year Employment 2002 Projected Year Employment 2012 Life, Physical and Social Science Occupations Life Scientists 43,057 48,702 Employment Change (%) 20022012 13.11% 4,585 5,271 14.96% Biochemists and Biophysicists Microbiologists 352 431 22.44% 768 912 18.75% Epidemiologists 44 50 13.64% Medical Scientists 632 789 24.84% Life Scientists ( all other) 1,579 1,824 15.52% Title Source: Illinois Department of Employment Security, Economic Information & Analysis Division. August 2006. Graduates from the proposed MS program will constitute a tiny proportion of the projected growth in demand for this sector. 9. Program Description 9.1. Provide a brief narrative description of the program, including a list of its central academic objectives. Explain how the curriculum is structured to Revised 2/17/2016 13 meet the program’s stated objectives. Provide a complete catalog description for the proposed program, including: program admission and graduation requirements; and curriculum design, including course descriptions. MS in Clinical and Translational Research Mailing Address: MS in Clinical and Translational Research Program Division of Health Policy and Administration School of Public Health (MC 923) 1603 West Taylor Street Chicago, IL 60612-4394 Campus Location: 778A SPHPI Program Code: Telephone: (312) 996Email: ____@uic.edu Web Site: http://www.uic.edu/sph/_____ Program Coordinator: Jack Zwanziger Directors of Graduate Studies: Sylvia Furner The MS in Clinical and Translational Science has been designed for applicants with previous clinical training or those in concurrent clinical degree programs, especially those in fellowship programs in the health sciences, postdoctoral training positions, or junior faculty with clinical responsibilities. The MS in Clinical and Translational Science is intended to train clinicians to become leaders in clinical and translational research. Students, primarily post-doctoral or postresidency fellows and junior faculty, will learn the basic skills used by clinical researchers supplemented by a broad array of relevant electives that will provide the basic concepts and theories consistent with each student’s goals and objectives. Each student will work with his/her advisor and the program director to develop a program of study uniquely tailored to individual interests and future goals. As part of the MS in Clinical and Translational Science, students will learn to communicate their insights effectively, to write well-conceived and persuasive grant applications and to ensure the ethical treatment of their subjects. As apprentice clinical investigators, they will learn how to participate in a broader multidisciplinary research community that includes basic and social scientists, as well as clinicians from other areas of clinical practice. Graduates of the MS in Clinical and Translational Science will have the skills to direct a broad range of clinical studies, including the translation both of scientific knowledge into clinical science and of clinical science into practice. They will be able to interact effectively with all of the complementary disciplines with which clinical investigators need to collaborate. At the end of the program, trainees will not be expert biostatisticians or survey researchers or microbiologists, for example, but they will be able to interact Revised 2/17/2016 14 effectively with all of the complementary disciplines that they as clinical investigators will need to collaborate with to be productive and successful. The MS in Clinical and Translational Science consists of three basic components: 1) a multi-disciplinary didactic program 2) a series of workshops and seminars 3) a research project under the mentorship of senior clinical researchers. Completion of the program will take two years for full-time students. Part-time students will generally take three to four years to complete the program. The vast majority of trainees is expected to be clinicians from across UIC, as well as from neighboring hospitals and institutions. The didactic program will consist of core coursework (18 semester hours) in the following areas: quantitative methods, epidemiology, research ethics, research design, and grant writing. Students, with guidance from the program director and advisor, will select electives from a broad array of relevant courses (14 semester hours)—attached are letters of support from the Deans of the Colleges of Applied Health Sciences, Dentistry, Nursing and Pharmacy regarding access to relevant courses in their colleges. This combination of core and elective coursework will provide students with the skills and knowledge they will need to conduct high quality clinical and translational research. In addition to the didactic coursework, students will attend seminars to provide them with exposure to the broad range of clinical and translational research. The program has initiated a monthly Translational Research Seminar Series to provide a venue in which experienced basic and applied researchers explore a given topic (the 2006-2007 seminar schedule is in Table 2 below). Other seminar series with different relevant focus areas may be developed as well in response to programmatic needs. Students will also attend workshops that enhance their professional skills. The MS will culminate in a mentored research project in which the student will work closely with one or more senior researchers. The mentored research project will give students the opportunity to apply the knowledge they have acquired in classes and workshops. The degree of mentoring will depend on the needs of individual students, some of whom may already have extensive research experience, whereas others may have extremely limited research experience. Admission Requirements In addition to the Graduate College minimum requirements, applicants must meet the following program requirements: Master of Science in Clinical and Translational Science Baccalaureate Degree Required. An applicant must have (1) a post-baccalaureate graduate or professional degree at the doctoral level OR (2) a baccalaureate degree from an accredited U.S. or Canadian school with concurrent enrollment in a clinical degree program. Revised 2/17/2016 15 Grade Point Average 3.0/4.0 for the final 60 hours of undergraduate study and for all cumulative graduate work previously taken. Tests required MS applicants with a graduate or professional degree at the doctoral level (e.g., PhD, ScD, MD, DDS, DNP, DO, DPT, DVM, PharmD) from an accredited U.S. or Canadian school or who are licensed to practice in the United States are exempt from the GRE requirement, but must instead submit scores for the appropriate exams in their profession such as the USMLE for physicians, National Board Dental Examinations Part I for dentists, and NPTE for physical therapists. (For example, current medical residents would submit scores for Part I and Part II of the USMLE. Medical fellows must submit scores for Part I, Part II, and Part III of the USMLE.) Minimum TOEFL Score International applicants must submit TOEFL scores taken within two years prior to admission. The minimum TOEFL score accepted by the Graduate College is 550 (paper-based test) or 213 (computer-based test). The minimum TOEFL scores accepted for admission to the Graduate College for the new TOEFL iBT includes minima for the four subsections, as well as the total score. The required scores are: Reading 19, Speaking 20, Listening 17, Writing 21, and Total 80. The TOEFL examination is not required for students who have completed at least two academic years of full-time study in a country where English is the native language and in a school where English is the language of instruction within five years of the proposed date of enrollment in the University. In addition, the TOEFL examination is not required of non-native English speakers who have a minimum of one year full-time employment in the U.S. or other country where the only official language of the country is English. Applicants must submit a letter from their employer verifying at least 12 consecutive months of employment and describing their English language skills. Letters of Recommendation Three required. One of the letters of recommendation must be from the applicant’s immediate supervisor or clinical program academic advisor specifically committing the applicant’s home department to supporting the applicant during their tenure in the MS program. Personal Statement a career-goal statement outlining (1) reasons for pursuing the MS in Clinical and Translational Science at UIC, including the intended research focus and (2) career goals. Other Requirements Applicants must submit a statement of interest and CV/resume to Susan Lynch via email, slynch2@uic.edu. Formal application to the School is through SOPHAS (Schools of Public Health Application Service), a new service of the Association of Schools of Public Health, which represents the 38 CEPH accredited schools of public health. Applicants must also submit a Supplemental Application directly to the School. Applications are available at: http://www.uic.edu/sph/admissions_apps.htm. Applicants must also include academic transcripts and a resume or curriculum vitae in their application package. Selected applicants will be scheduled for personal interviews. Deadlines Students will be admitted for the fall semester only. Applications must be submitted by May 15 for admission to the School of Public Health for the following fall semester. Applicants with international credentials are strongly Revised 2/17/2016 16 encouraged to submit their applications by January 1 for the fullest consideration. Degree Requirements In addition to the Graduate College minimum requirements, students must meet the following program requirements: Masters of Clinical and Translational Science Minimum Semester Hours Required 48. Course Work Required: 18 core course semester hours consisting of: BSTT 400, BSTT 401, EPID 403, EPID 406, HPA 590 MHPE 512 AND MHPE 534. All course descriptions are contained below. Electives: 14 semester hours. Detailed below. Comprehensive Examination None. Thesis, Project, or Course-Work-Only Options 16 semester hours of required mentored research (IPHS 598), producing a paper that is a scholarly contribution to the field in the form of a journal article, pilot data for a grant application, and a thesis-defense of the paper and data. Other Requirements Each student must maintain regular attendance at seminar series (see 2006-2007 schedule below); successful completion of the required skill development workshops; and a grant proposal based upon the mentored research project. A program coordinator, academic advisor and mentor will counsel students in terms of appropriate coursework and timing, and a research training committee will provide mentorship in designing and conducting the research project. Core Courses (18 credit hours) The core courses and other program requirements are outlined below, including a list of possible electives. Students will work with their mentor and academic advisor to tailor a comprehensive program of study that meets their individual needs and interests. A student may be able to substitute core with alternative courses, if the alternative course is judged to have equivalent content. Judgment on equivalency of substitute courses will be made by agreement of the student’s academic advisor and the program director. CORE COURSES (18 semester hours) Biostatistics (BSTT) BSTT 400 Biostatistics I 4 hours. Descriptive statistics, basic probability concepts, one- and two-sample statistical inference, analysis of variance, and simple linear regression. Introduction to statistical data analysis software. Enrollment restricted to public health students; other graduate, professional and advanced undergraduate students admitted by consent as space permits. Revised 2/17/2016 17 To obtain consent, see the SPH registrar. BSTT 401 Biostatistics II 4 hours. Simple and multiple linear regression, stepwise regression, multifactor analysis of variance and covariance, non-parametric methods, logistic regression, analysis of categorical data; extensive use of computer software. Prerequisite(s): BSTT 400. Epidemiology (EPID) EPID 403 Introduction to Epidemiology: Principles and Methods 3 hours. Introduction to descriptive and analytic epidemiology, and determinants of health and disease in populations. Measures of occurrence, association and statistical testing will be addressed, along with study designs, bias and confounding. Prerequisite(s): Credit or concurrent registration in BSTT 400 and graduate or professional standing; or consent of the instructor. EPID 406 Epidemiologic Computing 3 hours. Hands-on course for students using SAS and other computer tools for epidemiologic analysis. Addresses theoretical and practical issues in statistical programming for epidemiology students. Prerequisite(s): BSTT 400 and EPID 400; or BSTT 400 and EPID 403; or consent of the instructor. Health Policy and Administration (HPA) HPA 590 Grant Writing 1 hour. Students will learn how to write a grant application through the guidance of a mentoring committee. They will formulate a research proposal which will be presented to a panel of researchers who will critique the proposed study. Medical Education (MHPE) MHPE 512 Ethics in Clinical Research. 1 hour. Survey of key ethical issues involved in conducting research with human subjects, including informed consent, confidentiality, access and equity. Course Information: Extensive computer use required. Requires completion of an online course in human subjects research, to be supplemented by classroom discussion of the topics raised in that course and others. Same as HPA 512. Prerequisites: Approval of the department. Students must be enrolled in the Master of Science in Public Health program. MHPE 534 Research Design & Grant Writing. 2 hours. Introduction to the skills necessary to plan a research project and write a research grant proposal using a systematic approach. Course Information: Same as HPA 534. Prerequisite(s): Approval of the department. Revised 2/17/2016 18 MENTORED RESEARCH COMPONENT (16 semester hours) Interdisciplinary Public Health (IPHS) IPHS 598 Research in Public Health Sciences - M.S. 0 - 16 hours. Individual research in public health directed by a faculty member. Directed toward the thesis requirements for the Master of Science degree. Satisfactory/Unsatisfactory grading only. May be repeated. Students may register in more than one section per term. Prerequisite(s): Consent of the instructor. Elective Courses (14 credit hours) With input from their advisor and mentor, students will choose appropriate electives that are tailored to their unique backgrounds, skill levels, areas of interest, research focus, and future goals. Students will be able to select from a broad list of elective courses because of the enormous range in prior research experience and educational programs, as well as in career objectives. Consistent with educational theory for mature learners, the MS combines a prescriptive component—that defines the basic program skills—with a broad set of options. Students, their academic advisors and their mentors will select electives to provide the student with the required set of skills. To focus this process the program has identified two exemplary subject areas, Psychosocial/Behavioral Sciences and Human Applications of Basic Sciences, as examples of areas that many of the students will select. For each, a possible set of electives has been identified, but they should be regarded as exemplary only since the electives will be chosen based upon the specific interests and educational needs of each student. a) For students with primary interests in the Psychosocial/Behavioral area: One or more introductory courses in social and/or behavioral sciences such as HPA 460 Introduction to the Economics of Health and Healthcare and/or CHSC 401 Behavioral Sciences in Public Health. One or more methods courses such as BHIS 504 Methods in Qualitative Inquiry, NUSC 548 Methodological Issues for Cross-Cultural Research, and/or HPA 557 Measurement in Health Services Research. One or more applied methods courses, such as PMAD 573 Principles of Economic Evaluations of Health Care Interventions, CHSC 447 Survey Planning and Design, and/or MHPE 535 Translating Research Into Practice. HPA 460 Introduction to the Economics of Health and Healthcare 2 hours. Introduces principles of economic analysis, with examples from public health Revised 2/17/2016 19 and medical care. Examines how consumers and companies decide what to buy or sell, why markets determine a product' s price, and when public intervention improves welfare. CHSC 401 Behavioral Sciences in Public Health 3 hours. Provides grounding in the social and behavorial sciences to analyze public health issues. Includes analysis of individual, community, institutional, and societal factors influencing health and illness. Prerequisite(s): Enrollment restricted to public health students; other graduate, professional and advanced undergraduate students admitted by consent as space permits. To obtain consent, see the SPH registrar. BHIS 504 Methods in Qualitative Inquiry 3 hours. Qualitative research methods to account for systematic description of environments where quantitative methods are not sufficient. Prerequisite(s): BHIS 500 and BHIS 510 or consent of the instructor. NUSC 548 Methodological Issues for Cross-Cultural Research 3 hours. Conceptual, methodological and ethical issues for research with varied racial/ethnic backgrounds. Applies acculturation, translation, immigration, and health behavior issues to clinical, community, and international settings. Prerequisite(s): NUSC 511; and consent of the instructor. HPA 557 Measurement in Health Services Research 3 hours. Presents measurement, reliability and validity theory and assessment using correlation, internal consistency, factor analysis and others. Application in developing, analyzing, and reporting behavioral and/or organizational measures. Prerequisite(s): BSTT 400 and BSTT 401; or consent of the instructor. PMAD 573 Principles of Economic Evaluations of Health Care Interventions 3 hours. Principles, models and practical methods for the economic evaluation of health care services with an emphasis on pharmaceutical care. Same as HPA 573. Previously listed as PMAD 571. Prerequisite(s): Graduate standing; and consent of the instructor. CHSC 447 Survey Planning and Design 3 hours. Theory and applications of sample survey planning and design for conducting research in health sciences and related fields. Addresses three major topics: survey design and planning, sampling and data collection procedures. Same as PA 447. Prerequisite(s): Graduate or professional standing and BSTT 400 or the equivalent. Recommended background: Credit in CHSC 446 or the equivalent. MHPE 535 Translating Research into Practice 3 hours. Current theory and practical reality related to the adoption and use of new scientific findings in patient care. The influence of research on public policy. Same as HPA 535. Extensive computer use required. Prerequisite(s): Graduate or professional standing; and approval of the department. Revised 2/17/2016 20 b) For students with primary interests in the Human Applications of Basic Sciences area courses will build upon a foundation of the biological sciences learned in their clinical training and permit somewhat greater specialization. Students are strongly recommended to take GCLS 512, Logic in Experimental Biology, as well the relevant science theory such as GCLS 501. For example, students interested in infectious diseases may, in addition to GCLS 512, be asked to read a Molecular Biology textbook (eg. Watson, Molecular Biology of the Gene) to get the required background and then GCLS 511 Molecular Genetics 3 cr GCLS 504 Research Methods I, 2 cr GCLS 505 Research Methods II, 1 cr MIM551 Immunology, 2 cr GCLS 501 Biochemistry 3 hours. Fundamental properties of biomacromolecules, the thermodynamics underlying basic biochemical processes and the properties of enzymes, including the kinetics of operation, and regulation, illustrated with important examples. Restricted to students enrolled in a graduate program offered through the Colleges of Medicine or Pharmacy or the departments of Bioengineering or Biological Sciences or consent of the instructor. GCLS 502 Molecular Biology 3 hours. Core molecular biology course covering basic principles of gene expression, genome replication and molecular interactions important to biological processes in prokaryotes and eukaryotes. Restricted to students enrolled in a graduate program offered through the Colleges of Medicine or Pharmacy or the departments of Bioengineering or Biological Sciences or consent of the instructor. GCLS 503 Cell Biology and Integrative Physiology 4 hours. Advanced course on fundamental aspects of cell biology; basic concepts will be integrated with key examples of human physiology which span gene, protein, cell, tissue, organ and whole body function. Credit is not given for GCLS 503 if the student has credit in BCHE 561 or ANAT 585 or MIM 585 or PHYB 585. Restricted to students enrolled in a graduate program offered through the Colleges of Medicine or Pharmacy or the departments of Bioengineering or Biological Sciences or consent of the instructor. GCLS 504 Research Methods I 1 TO 2 hours. Lectures, demonstrations, and discussions concerned with principles and practical aspects of modern quantitative biochemical, molecular biological, physiological and biophysical methodology such as separation techniques and studies of biomembranes. May be repeated. Students may register for more than one section per term. Restricted to students enrolled in a graduate program offered through the Colleges of Medicine or Pharmacy or the departments of Bioengineering or Biological Sciences or consent of the instructor. Revised 2/17/2016 21 GCLS 505 Research Methods II 1 TO 3 hours. Lectures, demonstrations, and discussions concerned with principles and practical aspects of modern quantitative biochemical, molecular biological, physiological and biophysical methodology such as bioimaging and biochemical analysis. May be repeated. Students may register for more than one section per term. Restricted to students enrolled in a graduate program offered through the Colleges of Medicine or Pharmacy or the departments of Bioengineering or Biological Sciences or consent of the instructor. GCLS 511 Molecular Genetics 3 hours. Core molecular genetics course covering classical and molecular principles of microbial and Mendelian genetics. Systems covered include bacteria, bacteriophage, animal viruses, yeast, Drosophila, mouse, and human. The goals of this course are to ensure that graduate students have a broad base of knowledge in the molecular genetics of prokaryotic, eukaryotic, and viral genetic systems. Students will gain an understanding of the principles, terminology and techniques of molecular genetics important for most aspects of biomedical research. Students will acquire fundamental skills that are necessary for reading current literature, critical analysis and for use in their own research. GCLS 512 Logic in Experimental Biology 2 hours. This course explores some of the central philosophical issues of scientific research in modern experimental biology. Examples are taken from genetics, biochemistry, molecular biology, developmental biology, neurobiology and microbiology. The course is designed to make sense of explanatory strategies, concepts and ways of reasoning employed by life science researchers. It is intended to augment historical explanations of scientific change with an account of epistemic norms and standards that are operative in science. Logic in Experimental Biology will use specific case studies from the current literature as well as a primary text, Philosophy of Experimental Biology, by Marcel Weber. Contents of Philosophy of Experimental Biology: 1. Introduction; 2. Reductionism and the nature of explanations; 3. Discovery: solving biological problems; 4. Scientific inference: testing hypotheses; 5. Experimental systems: a life of their own?; 6. Model organisms: of flies and elephants; 7. Reference and conceptual change: out of Mendel’s garden?; 8. Developmental biology and the genetic program: explaining ontogeny; 9. Scientific realism: in search of the truth. MIM 551 Advanced Immunology 2 hours Concepts in immunochemistry, immunogenetics, molecular immunology, cellular immunology and immunopathology at the intermediate level. These lists are not exhaustive, and students will work with their advisor and primary mentor to tailor a comprehensive program of study that meets their individual needs and Revised 2/17/2016 22 interests and that are found to be suitable for the program. All students will have to select electives to full the Graduate College requirement to have completed at least nine (9) credit hours of 500-level courses excluding thesis or independent study. Mentored Research (16 credit hours) Each student’s mentorship committee will be led by an experienced clinical investigator who will have the primary responsibility to guide trainees in conducting clinical and translational research in their areas of interest. Trainees will complete a research project in the second year of the program (for full-time students) that will culminate in a thesis judged to be a scholarly contribution to the field in the form of a journal article. The research project will also provide pilot data for a grant application. The intensity and modalities of mentoring may vary based on students’ prior research experience, but all students are required to complete 16 semester hours of research with both of the above outputs. The paper and grant proposal will provide the opportunity to assess the student’s ability to integrate and apply the knowledge and skills acquired. The mentoring committee and a reviewer nominated by the program director will review and evaluate the paper and the thesis defense. The student’s grant proposal will be evaluated by the faculty member teaching HPA 590. Table 2. 2006-2007 Translational Research Seminar Schedule DATE SPEAKER(S) TITLE 9/27/06 Thomas Prohaska, PhD University of Illinois at Chicago 10/25/06 Garth Rauscher, PhD University of Illinois at Chicago “Overcoming Barriers in Translational Research and Practice” “Transdisciplinary Strategies for Understanding Disparities in Breast Cancer” Elizabeth Wiley, MD University of Illinois at Chicago 11/22/06 Lisa Sharp, PhD University of Illinois at Chicago “Experiences in a SocioEnvironmental Approach to the Problem of Asthma in Chicago” Jay Shannon, MD Cook County Bureau of Health Services 1/24/07 David Carley, PhD University of Illinois at Chicago “Rational Drug Discovery for Sleep-Related Breathing Disorders” 2/28/07 Marian Fitzgibbon, PhD University of Illinois at Chicago 3/28/07 John Sweeney, PhD University of Illinois at Chicago “From Efficacy to Effectiveness: Developing Obesity Prevention Interventions for Children” “Translational Cognitive Neuroscience” Revised 2/17/2016 23 4/25/07 Theodore Mazzone, MD University of Illinois at Chicago “Computerized Diabetes Education: Translating Research into Practice” Ben Gerber, MD, MPH University of Illinois at Chicago 5/23/07 Susan Gapstur, PhD, MPH Northwestern University TOPIC: TBD Vince Freeman, MD, MPH University of Illinois at Chicago 9.2.1. Explain what students are expected to know and/or be able to do upon completing the program. Students earning an MS in Clinical and Translational Science will have the skills and knowledge required to conduct high quality clinical research. They will be able to communicate their insights effectively, write well-conceived and persuasive grant applications, and ensure the ethical treatment of their subjects. Finally, as apprentice clinical investigators, they will learn how to participate in a broader multidisciplinary research community that includes basic and social scientists, as well as clinicians from other areas of clinical practice. At the end of the program, trainees will not be expert biostatisticians or survey researchers, for example, but they will be able to interact effectively with the complementary disciplines with which clinical investigators need to collaborate. Core knowledge gained Upon completion of this program, students will demonstrate knowledge in the following areas: The full range of study designs and their strengths and weaknesses The application of statistical and epidemiologic methods to clinical research The ability to use standard statistical programming packages to generate needed data The responsible conduct of clinical research The content for an NIH grant application Specific skills/competencies to be demonstrated Upon completion of this program, students will be able to: Responsibly conduct clinical research Define a researchable question Design a research study Write a persuasive grant application Describe the analytical methods pertinent to their research Revised 2/17/2016 24 Participate in a broader, multidisciplinary research community that includes basic and social scientists, as well as clinicians from other areas of clinical practice TABLE 4. Core Competencies and Related Courses Competencies Courses (credit hours) 1. Applying appropriately basic epidemiologic terminology/concepts to clinical research EPID 403 (3) EPID 406 (3) 2. Using statistical programming to analyze data 3. Demonstrating an understanding of study designs (e.g., cohort), when to employ various designs, relevant strengths and weaknesses, and interpretation of results 4. Applying basic statistical concepts and techniques to data analysis BSTT 400 and BSTT 401 (8) 5. Demonstrating knowledge of the requirements for responsible conduct of clinical research MHPE 512 (1) 6. Defining a researchable question MHPE 534 and HPA 590 (3) 7. Designing a study 8. Writing a persuasive grant application In addition, through elective coursework, students will acquire the relevant theory and methods identified as being needed for their particular needs and interests. 9.3. Describe the strategies to be incorporated into the proposed program to promote student learning. As adult learners, students will be able to combine a didactic component with broad choice in elective courses, focused skill-building workshops and extensive mentored research. Didactic coursework will lay the groundwork of essential knowledge and skills for clinical research, and workshops and seminars will provide supplementary professional training. The mentored research project is the culminating educational experience of the MS. The Didactic Contents of the MS The didactic portion of the MS occupies the first year of the program if taken on a full time basis (two years on a part-time basis). It is designed to provide trainees with an understanding of the analytical tools used by biostatisticians and epidemiologists and the application to health of the relevant concepts and theories explored in elective Revised 2/17/2016 25 coursework. As illustrated in Table 4 above, the Clinical Research Training Program’s Curriculum Committee has identified competencies required by clinical investigators, and these competencies have been mapped to existing courses. Core coursework covers the following areas: quantitative methods, epidemiology, research design, grant-writing, and research ethics. As mentioned earlier, students may be able to substitute core courses with courses judged to have equivalent content, with the agreement of the program director and their advisor. A collection of electives will be chosen by students and primary advisors based on prior experience, current interests, and career goals. Trainees will receive eighteen credit hours for the required coursework, and fourteen credit hours for electives. Mentored Clinical Research Training In conducting a research project, students are expected to integrate the knowledge gained through courses and workshops over the first year of the program. As outlined below, the intensity of the mentoring component will vary based upon students’ prior research experience. During the first year of the program, trainees will develop a preliminary research plan with the help of the Program Director and their primary mentor. At the beginning of the summer between the first and second year, the trainee will submit a research plan and identify the members of a proposed mentoring committee with the full range of disciplines needed to successfully complete their research project. Students will draw from a substantial pool of potential research areas and mentors at UIC. Members of mentoring committees must have been the PI on at least one externally funded clinical research study and previously have worked in a mentoring capacity. The committee and research plan will then be reviewed by the Research Training Committee and modified, if necessary, prior to the beginning of the second year. It is the program’s intention through this iterative process to ensure that the trainee’s research project, and therefore membership on mentoring committees is not just an obligation, but also scientifically interesting. The mentoring committee will provide a model of clinical research conducted by a multidisciplinary team. Each committee must review the trainee’s progress at the end of the fall and spring semester and will grade the research paper at the end of the year. The student’s research plan will form the basis for the grant-writing course, in which trainees will formulate a research idea as part of their mentored research study. Trainees will learn how to draft effective sections of a grant proposal, ranging from “specific aims,” through “background and significance,” “preliminary studies,” and “research design and methods.” They will develop a budget, IRB submission and address other sections required for an NIH grant application such as the inclusion of women, minorities and children. The intention is that the grants written by the trainees will be submitted for subsequent funding. The program recognizes that students’ individual mentoring needs may vary depending on their level of research experience and knowledge. With this in mind the mentored research component can be modified to best suit a student’s needs and skill base. The Revised 2/17/2016 26 intensity of the mentoring component will be at the discretion of the Program Director and the advisor, who may tailor the mentoring requirements to each individual’s circumstances. Workshops and Seminars Workshops and seminars are a central part of the MS program, providing students with opportunities to gain professional skills, network, and learn about issues critical to success in clinical research. Workshops will address a variety of skills needed for success as a clinical researcher. The monthly Translational Research Seminar Series will expose trainees to the full range of clinical research being conducted at all of the Health Sciences Colleges at UIC. This ongoing seminar series will not only facilitate the education of the program’s trainees, but will also help foster a clinical research community across the Health Sciences Colleges. The knowledge trainees acquire through the required coursework will be supplemented by the special workshops to provide them with the professional skills necessary to be leaders in clinical research. They include: Professional Communication: This workshop will teach trainees how to write abstracts, posters, presentations (including use of PowerPoint software) and journal articles. The workshop will focus on the best techniques to use in communicating ideas through each medium. The workshop will consist of four weekly three-hour sessions. Community-based Research: This experience will provide instruction on the issues raised by community-based research. Workshops will consist of a combination of sessions by researchers and members of community organizations who have conducted community-based research and discussions of the code of conduct expected of UIC researchers working in community settings. Students will also visit community organizations to observe community-based research. Trainees will be expected to attend these workshops and seminars as part of their MS requirements. Additional Resources Through a department-supported clinical and translational research listserv, students will be kept abreast of relevant university wide events, including, but not limited to, medical seminars, conferences, workshops and guest speakers. After completion of the MS, participants may elect to stay on the listserv to keep informed of continuing education and professional opportunities, research awards, and support services offered to Clinical and Translational Investigators at UIC. In addition to information sharing, this listserv would help in promoting a cross-disciplinary community of clinical and translational research. Revised 2/17/2016 27 In addition to the listserv, a university-wide clinical and translational research website will be developed that will highlight current events and links to researchers with specific interests. Revised 2/17/2016 28 RESOURCES 10. Complete Table I to show student enrollment projections for the program. Enrollment projections In generating Table 1, the following assumptions were made: 1) annual admission cohorts of 10 students of whom a. 2 are full time (12+ credit hours/semester; finish in two years) b. 4 are part time (8+ credit hours/semester; finish in 3 years) c. 4 are part time (6+ credit hours/semester; finish in 4 years) Table I Student Enrollment Projections for the New Program Number of Program Majors (Fall headcount) Annual Full-Time-Equivalent Majors Annual Credit Hours in EXISTING Courses1 Budget Year 10 2nd Year 20 3rd Year 28 4th Year 32 5th Year 32 6.67 13.33 18 20 20 160 320 432 480 480 0 0 0 0 0 0 2 6 10 10 Annual Credit Hours in NEW Courses Annual Number of degrees Awarded 11. Complete Table II (even if no new state funding is requested in the budget year). Show all sources of funds, both state and non-state, and reallocations. Provide a narrative budget that includes the following: Projected increments in total resource requirements (line 1) in terms of projected staff requirements, equipment and instructional materials, library requirements, and contractual services for internships, practica, or clinical placements. Explanation of required new state resources (line 6) in the budget year in terms of assumptions and factors used to construct line items 7 through 11. If resource requirements in the budget year include non-recurring costs (e.g., Revised 2/17/2016 29 one-time equipment purchases), describe how these resources will be reallocated in subsequent years. Table II TOTAL RESOURCE REQUIREMENTS FOR THE NEW UNIT Current Budget 2nd Year Year Year $26,240 $37900 $40900 3rd Year $43900 4th Year $43900 1 Total Resource Requirements 2 Resources Available from Federal Sources1 0 0 0 0 0 3 Resources Available from Other Non-State Sources1 0 0 0 0 0 4 Existing State Resources2 $ $26240 $69,058 $83,386 $92,051 5 Resources Available through Internal Reallocation3 $26,240 $11660 $3000 $3000 $0 6 New State Resources Required4 0 0 0 7 Breakdown: New State Resources Required FTE Staff5 8 Personal Services 9 Equipment and Instructional Needs 0 0 10 Library 11 Other Support Services6 1 These lines reflect funds available (not incremental funds) from non-state sources in any given year 2 Existing state resources in each successive year are equal to the sum of the previous year’s existing state resources (line 4); plus resources made available through internal reallocation (line 5); plus new state resources (line 6). If state resources allocated to a program in any given year (line 4) exceed state resource requirements needed to support Revised 2/17/2016 30 the program in the following year, state resource requirements should be reduced with a negative dollar adjustment on line 5. The sum of lines 2 through 6 will always equal line 1. 3 Numbers can be either positive (allocated to the program) or negative (allocated away from the program). 4 Reflects the level of state funding requested in the referenced year. Dollars reported are incremental. 5 Reflects the number of FTE staff to be supported with requested funds. Not a dollar entry. 6 Other dollars directly assigned to the program. Do not include allocated support services. Table II was generated making the following assumptions: The MS in Clinical Translational Science will assess the tuition differential currently charged of graduate students in the public health programs (MS, PhD, MPH, DRPH). The costs associated with the program include possible additional sections in core courses, costs for the mentoring program, and non-instructional costs such as administration and supplies. 1) an average of 6 students in all the core courses in year one and 10 students, thereafter. 2) Instruction for all additional sections for core courses is above load and faculty are reimbursed. 2) The program is assessed a per student basis of the cost of an incremental section divided by the maximum class size, for example a core course with athe costs of an additional section of $10,000 and a maximum class size of 20 has a per student cost of $500. 3) MS students will be dispersed enough in the electives so that they do not trigger the need for an additional section. 4) The mentoring program will cost $1000 per student per semester during the research period (2 semesters for FT and 8+ credit hour students; 3 semesters for 6+ credit students). 5) Epidemiology and Biostatistics classes have maximum enrollments of 50 and additional sections costs $13000. 6) MHPE classes have maximum class sizes of 20 and additional sections costs $13,000. 7) HPA 590 requires a senior faculty as instructor costing $15,000 for an additional section and is limited to 20 students. 8) Non-instructional costs are administration ($10,000) and supplies ($1000). 12. Describe the institutional resources available to develop and maintain a quality program. Include the following elements in your discussion: Revised 2/17/2016 31 Faculty qualifications, evaluation, and reward structure; Adequacy of library and related resources; Adequacy of student support services, support staff, equipment, and other resources; and, Demonstration of teaching/scholarship effectiveness and course evaluation; Faculty Qualifications The proposed MS program draws from a broad faculty base. Faculty for the core courses are current faculty in the School of Public Health and the College of Medicine and the core courses are drawn from existing, formally accredited programs (MPH and MHPE). As a result, the required courses and the corresponding faculty have been evaluated and have evolved in response to these evaluations. The faculties listed below are those currently associated with the core courses and they are a well-qualified, indeed distinguished, group. Faculty from SPH who will be teaching in the program include: Craig Beam, PhD, Iowa State University, Biostatistics Richard Campbell, PhD, University of Wisconsin Madison, Sociology Hua Yun Chen, PhD, University of Michigan, Biostatistics Susan Curry, PhD, University of New Hampshire, Psychology Donald Hedeker, PhD, University of Chicago, Behavioral Sciences Domenic Reda, PhD, University of Illinois at Chicago, Biostatistics Deborah Rosenberg, PhD, University of Illinois at Chicago, Epidemiology Garth Rauscher, PhD, University of North Carolina Chapel Hill, Epidemiology Faculty from COM who will be teaching in the program include: Georges Bordage, MD, PhD, Université Laval, Michigan State University, Educational Psychology Timothy Murphy, PhD, Boston College, Biomedical Sciences For the mentored research component, trainees will draw from a substantial pool of potential research areas and mentors at UIC. Members of mentoring committees must have been the Principal Investigator on at least one externally funded clinical research study and previously have worked in a mentoring capacity. The pool of potential clinical research mentors at UIC is impressive in its size, scope and diversity. Given space limitations it is impossible to review all of the areas of particular strength, and certainly not the contributions of all of these investigators. Research across the six health sciences colleges is strong in many areas, including the management of chronic conditions, women’s health, disability and rehabilitation. The Research Training Committee, which will guide and evaluate the mentored research component of the program, will meet with every trainee to collaboratively identify his or her mentors. The Research Training Committee consists of senior researchers with extensive experience in both research and mentoring. It has the following members: Phillip T. Marucha, DMD, PhD, University of Connecticut, Dentistry and Immunology Revised 2/17/2016 32 Phyllis E. Bowen, PhD, Cornell University, Nutrition Daniel M. Corcos, PhD, University of Oregon, Movement Science Jay L. Goldstein, MD, University of Illinois at Chicago, Medicine David Henry, PhD, University of Illinois at Chicago, Psychology James P. Lash, MD, University of Chicago, Medicine Mariann R. Piano, RN, PhD, University of Illinois at Chicago, Nursing Science Glen T. Schumock, PharmD, University of Washington, Clinical Pharmacy Richard B. Warnecke, PhD, Duke University, Sociology Evaluation of Faculty Competence and Performance School of Public Health Within the School of Public Health, faculty evaluation is carried out primarily through the Annual Performance Report and the promotion and tenure review. In 1999 the school instituted a teaching evaluation program which includes additional review that is focused on the teaching component of faculty performance. Annual Performance Report: At the end of each academic year, all tenured and tenure track faculty complete and submit to their division director the Annual Performance Report. Upon completion of review at the division level, the reports are forwarded to the dean and the senior associate dean for review. The report addresses the research, teaching and service components of faculty responsibility. The administration uses these reports to evaluate faculty performance for determination of merit salary increases and to monitor progress toward achieving tenure or promotion. College of Medicine Similarly, faculty evaluation in the College of Medicine is based upon an Annual Faculty Evaluation, Formal Evaluation of Teaching, and Promotion and Tenure Review. 1) Annual Faculty Evaluation: At the end of each academic year, all tenured and tenure track faculty complete and submit to their department head/chair a written report of productivity, including current, completed, and proposed research, publications submitted, teaching activities as described below, and service to the University. The administration uses these reports to evaluate faculty performance for determination of merit salary increases and to monitor progress toward achieving tenure or promotion. 2) Formal Evaluation of Teaching: The UIC College of Medicine is committed to the principle that a faculty appointment is a calling to scholarly excellence, and that teaching is a valid and essential form of scholarship. In an effort to move away from undervaluation of teaching, the COM has introduced mechanisms to better evaluate teaching contribution and quality. These mechanisms include new categories for documentation, including Instructional Innovations, Student Ratings of Instruction, Peer Ratings of Instruction (including both observation of teaching activities and instructional document review), Instructional Self-Review, and Information from Former Students. These evaluation procedures also help to assure that faculty teaching activities are accorded their appropriate importance in the promotion and tenure process. Revised 2/17/2016 33 Evaluation of faculty teaching activities is the responsibility of the department head/chair in collaboration with the faculty candidate. The department head/chair identifies whose teaching activities are to be evaluated for the promotion and tenure process, discusses the procedure for evaluation of teaching with the faculty candidate, assures that student evaluations of teaching are obtained, and the data are appropriately summarized, assigns responsibility for peer evaluation of teaching, assigns responsibility for peer evaluation of teaching products developed, summarizes a candidate’s contribution to curriculum and other products, instructs candidates to finalize personal statements on teaching activities, and solicits letters of evaluation from former students/residents/trainees. The faculty candidate becomes thoroughly familiar with the process for documenting teaching, discusses assembly of a portfolio with the department head/chair, maintains a file to build a portfolio of all professional activities related to teaching (annual listing of all teaching related activities, listing of recognitions received for teaching activities, listing of all individual advisees/trainees, graduate students, residents, fellows, etc. with dates and types of interactions, copies and descriptions of instructional innovations, descriptions of all contributions to curriculum development), facilitates arrangements for peer review of teaching, and develops a personal statement of teaching that explains his/her philosophy of education, place of teaching in career goals, progress toward those goals, and plans for future teaching activities. This data is then submitted for promotion and tenure review, along with additional evidence of additional scholarship, research, and service. Demonstration of teaching/scholarship effectiveness and course evaluation Teaching Evaluation: In examining teaching effectiveness at the School of Public Health, the program assesses the various dimensions of each faculty member’s teaching portfolio. In addition to student evaluation of faculty performance (described below), the program also uses peer evaluation and administrative evaluation of faculty teaching and advising. For assistant professors, peer evaluation of classroom teaching is conducted at the end of the second and fifth appointment years. This timing was based on the usual timing of tenure consideration (year six). The division director and faculty member meet to select one or two faculty reviewers per course. Administrative evaluation of teaching for assistant professors is conducted in years three and six. These reviews are timed to coincide with the Mid-Probationary Tenure Review and the Tenure Review. For tenured faculty, the peer evaluation and the administrative evaluation are conducted every five years subsequent to the granting of tenure. This timing was based on the likelihood of the implementation of a campus-wide post-tenure review system. As described above, the College of Medicine is also committed to excellence in teaching and has implemented mechanisms for capturing the quality of teaching and learning among faculty throughout the College. These data include an Annual Report of Faculty Teaching Effort, Teaching Documentation (includes instruments for students, peers, administrators and faculty to evaluate teaching), Supervision and Advising (includes documentation of faculty supervision and advising efforts involving students, residents, Revised 2/17/2016 34 fellows, and others), Product Development (includes a report and assessment of contributions to teaching methods, courses, programs, curriculum), and a Faculty Statement/Self-Assessment. Student Evaluation of Teaching and Advising: The School of Public Health assessment of teaching effectiveness is a crucial aspect of faculty review both for purposes of promotion and tenure and for annual performance evaluation. Teaching, a major responsibility of faculty, requires a multidimensional evaluation approach. The "teaching portfolio" consists of the following: Course Evaluation Questionnaires (CEQs) Student Evaluation of Academic Advising Course Evaluation Questionnaires (CEQs) are completed by students through an online process near the end of the semester. Students are asked to assess, among other things, the overall quality and value of the course, the appropriateness of its content, and the performance of the faculty teaching the course. Faculty members receive their results electronically, which allows them time to review their feedback and modify, if necessary, the course prior to its next offering. All CEQ forms are analyzed and a summary report for each faculty member is generated. The summary report, along with the original forms, is returned to the division for distribution to faculty and administrators. In addition, copies are kept in the Reference Center and are available for students and other faculty to review. These evaluations are then used to identify problem areas either in the design of the courses or in the teaching approach used by the faculty member. The College of Medicine employs similar procedures to measure student evaluation of courses and instructors. Students complete systematic and standardized evaluations of faculty teaching for every class and the department head/chair summarizes these forms for each faculty member for purposes of course improvement, as well as for faculty evaluation and promotion and tenure review. Students rate teachers on qualities such as clarity and organization, enthusiasm, knowledge and analysis, accessibility and responsiveness to student questions, and overall teaching effectiveness. Students are also provided the opportunity to include open ended comments regarding both teacher and course quality. Course evaluations are administered at the end of each course -- in the classroom for on-campus courses and online via Blackboard for online courses. Students respond anonymously on evaluations administered in the classroom. All student identifiers are removed from online responses. Student responses are compiled, resulting in reports including both quantitative summaries and qualitative comments. These reports are evaluated by the department head/chair and also provided to faculty members to inform course modification and adaptation of teaching style in order to improve the learning experience for students. Mentor Evaluation: Each student will meet with the Research Training Committee annually to monitor mentor quality and effectiveness. Trainees will be encouraged to discuss concerns about mentor fit and progress of the mentored research project, and modifications to the mentoring/thesis examining committee will be recommended when Revised 2/17/2016 35 necessary. Upon completion of the MS program each trainee will evaluate the mentors on their mentoring committee and the Program Director will provide this feedback to committee members. The Program Director will use this information in assessing the suitability of a clinical investigator for future service on mentoring committees. Please see Section 13 for more information on program evaluation. Faculty Reward Structure: In the School of Public Health and the College of Medicine, faculty are rewarded for excellence in teaching, research, and service, based on the results of the various evaluation measures described above. A faculty member’s annual evaluation – and hence salary increase – depends upon performance in teaching, research, and service. In the longer run, promotion is dependent on performance in these three dimensions Adequacy of library and related resources University Library System: The University Library of the University of Illinois at Chicago, consisting of the Richard J. Daley Library, the Science Library, and four sites of the Library of the Health Sciences, provides collections for students in all curricular areas, for graduate programs, and for faculty research. Library holdings number more than 2.2 million books and bound periodicals and over 4 million other items. The Library also offers access to 41,000 electronic journal titles (26,000 via subscription, 15,000 via full-text aggregated databases), over 250 databases/electronic resources, and over 52,000 electronic books. Library of the Health Sciences: The Library of the Health Sciences has four sites: Chicago, Peoria, Rockford, and Urbana. The Library of the Health Sciences contains comprehensive collections supporting teaching, research, and clinical programs in the Colleges of Medicine, Dentistry, Nursing, Pharmacy, and Applied Health Sciences; the School of Public Health, the UIC Hospital, Outpatient Care Center, and other medical center enterprises. The Library has over 2,500 print journal subscriptions and provides access to 32 databases, over 8,400 electronic journals, and over 2,900 electronic books in the health sciences. Key databases include Web of Science, Current Protocols, Embase, Clinical Evidence, MDConsult, Firstconsult, UpToDate, Stat Ref, Clinical Pharmacology, Access Medicine, EBM Reviews, Faculty of 1000, International Pharmaceutical Abstracts, Online Metabolic and Molecular Basis of Inherited Diseases, Health and Psychosocial Instruments, Biobase's Proteome Library, and Psychinfo. In addition, the Library provides training in PubMed which is free through the National Library of Medicine/NIH. Students in the MS program will primarily use the Library of the Health Sciences (LHS). LHS does subscribe to the following relevant journals in the clinical sciences and health services research in print format at one site and also electronically at all sites: JAMA, NEJM, Annals of Internal Medicine, Medical Care, HSR, Journal of Health Economics, and Health Affairs. The Library currently spends $2.4 million on health sciences related materials at the four LHS sites. Revised 2/17/2016 36 Library faculty and School of Public Health faculty find that library resources are adequate currently to support the MS program. Currently the library spends approximately $40,000 per year to support clinical and translational science as construed in the program proposal. Students in the MS program will primarily use LHS. Its collections, especially its journal collection, provide the necessary resources. LHS subscribes to relevant journals in the two primary areas of the program: clinical science (e.g., JAMA, NEJM, Annals of Internal Medicine) and health services research (e.g., Medical Care, Health Services Research, Journal of Health Economics, and Health Affairs). Computer Facilities for Instruction and Research The Academic Computing and Communication Center (ACCC) of UIC provides computing and networking services to the UIC community for use in instruction and research. The ACCC provides the following services for use by all UIC faculty, students and staff without charge: Public Personal Computer Labs and Instructional Facilities: There are 15 public personal computer laboratories (520 machines in total), six of which are instructional facilities that are available for public use when they are not being used for a class. There are both PCs and Macs in the labs and all are connected to the ADN-ii network and to the ACCC's local area network. Consulting: The ACCC provides free general consulting on issues related to the ACCC systems, the ADN-ii network, micro-computing and electronic mail among other things. Seminars: The ACCC offers free short courses on various topics of general interest (e.g., Word Perfect, MS Windows 95, Internet Tools). Electronic Mail: The ACCC provides all faculty, students and staff with free access to electronic mail. Instructional Support: The ACCC strongly encourages the use of its facilities for instructional purposes and provides assistance to faculty who wish to integrate computers and computing into their courses. There are currently several hightechnology lecture centers on campus that the ACCC supports, including one located in the SPH building at 1603 West Taylor Street. To help faculty better use the digital classrooms, the ACCC supports multimedia centers, which are available to faculty who wish to develop their own class materials and need access to multimedia equipment, software and expertise. Software: The ACCC offers a wide variety of software on all of its machines. It also distributes some personal computer and workstation software at reduced cost under university site licenses. Revised 2/17/2016 37 No charge is made for using ACCC facilities, but there is a small charge for each page printed on an ACCC printer. (Minimal charges are also made for the purchase of personal copies of the microcomputer software packages the ACCC distributes under university-site license agreements.) Each member of the UIC community has a monthly "educational allotment" applied automatically to his or her charges. Students will probably find that their educational allotment covers all of their printing needs. SPH Computer Laboratories: The School of Public Health operates three personal computer labs. One lab, located on the fifth floor of the SPH-West building has 26 Pentium class personal computers, a laser printer, a display device, a projection screen and a white board. An overhead projector is available on request. All of the computers in the lab are connected to the UIC ACCC’s local area network via ethernet connection. This connection provides a wide variety of software, as well as email and Internet access. Two more computer labs are located in the SPHPI building at 1603 West Taylor Street, where the MS program will be officially housed. The larger of the two labs is equipped with 31 hard-wired terminals and a high capacity laser printer, a display device, a projection screen and a white board. The smaller lab is located in the SPH Reference Center and has 17 hard-wired terminals and a high capacity laser printer. The labs are available for public use when not being used by a class. A valid UIC identification card is needed to enter the SPH after normal business hours and on weekends. College of Medicine Computer Laboratories: The College of Medicine operates the Edelstone Computer Center, located in the Edelstone lounge. This lab is open 24 hours a day, 365 days a year, and is staffed by support personnel during regular business hours. It is equipped with Windows Pentium personal computers and Apple iMacs, as well as three printers and a scanner. The lab and the classrooms are set up for wireless networking. Students in the College of Medicine also have access to three additional computer labs in the Benjamin Goldberg Research Center (BGRC). These labs offer a total of 52 Pentium class personal computers, 2 Mac personal computers, 2 printers and a projector for classroom use. Advising and Counseling Services Both the student’s faculty academic advisor and mentors will play a key role in assisting the student throughout the academic program. The advisor works with the student in developing and approving his/her course of study in a program proposal, including the selection of appropriate and relevant electives. In addition, the academic advisor will monitor research progress and ensure the appropriateness of the mentoring committee. Mentors will work closely with the student on planning, defining and carrying out the research project and in developing the final MS NIH-format research proposal. In addition, mentors will provide advice that is specific to the student’s field and/or home department. All MS students will be able to obtain assistance from the CRTP student academic coordinator, in addition to the dean’s office of student academic services. The School of Revised 2/17/2016 38 Public Health Student Handbook is an excellent resource to guide the student through his/her degree program, and specific MS program materials that clearly outline division and school-wide requirements will be available at orientation and from advisors. The School of Public Health, through funding from the Health Careers Opportunity Program, provides study review sessions for some of the core courses, in particular Epidemiology and Biostatistics. These sessions supplement the regular course instructional support. If specialized counseling needs are identified for a student, there are several resources available. First, a student can meet with his/her faculty advisor or program director. In many cases the student will be referred to the associate dean for student affairs, who then advises students and faculty of the campus services that may be appropriate to the given situation. Students can use all of the counseling services available throughout the university. This includes the Academic Center for Excellence, which provides courses, workshops, academic advising and counseling to help students improve their academic performance. Additionally, there is the University Counseling Service, which provides staff psychologists who are experts in clinical psychology and academic learning skills. Other services available to the student include the Office of Disability Services and the Student Health Service. Support Staff The School of Public Health employs three administrative support staff in the Health Policy and Administration Division. Two support the HPA academic programs and one provides administrative support to the entire Division. This number of state-funded staff is relatively stable. The school also supports both its academic and research missions with temporary staff. This includes extra help, undergraduate students and hourly employees. Funding from the NIH under the Clinical Research Training Program also provides resources for a Project Coordinator whose role is to support students and the Program Director. Equipment and Other Resources Space: The MS in Clinical Research program will be housed on the 7th floor of 1603 West Taylor Street (School of Public Health-Psychiatric Institute or SPHPI). This building provides modern, well-furnished and well equipped teaching, research, conference, and study facilities for faculty, students, staff, and community groups and organizations. The Office of the Dean of SPH and its administration, the Community Health Sciences Division, the Epidemiology and Biostatistics Division, and the Health Policy and Administration Division are housed in the School of Public Health building. The SPHPI building also offers an auditorium, a multi-purpose activity room for special events, a parenting room, the Alan W. Donaldson Student Lounge, and a café. Revised 2/17/2016 39 College of Medicine courses will be taught in class or online via the Blackboard Academic Suite. Online courses will be supported by the Department of Medical Education’s (DME) Online Development and Support Group. The College of Medicine teaching facilities include one large lecture room (998 A & B), equipped with a state-ofthe-art electronic whiteboard and Internet connection, one smaller conference room, and one in-house library equipped with Internet interface connections (for laptops) and a computer station also connected to the Internet and containing the library’s database. The Abdul W. Sajid Health Professions Education Memorial Resource Library was created in 1994, in memory of the late Abdul W. Sajid, former head of DME. Retired and former faculty members, including, George Miller, Abdul Sajid’s estate, Christine McGuire, Reed Williams, Annette Yonke, and Arther Elstein donated many of the holdings in the library, which contains 9,079 items (1,011 books, 7,692 reprints, and 915 other items). The library also contains four bound collections of medical education journals: Academic Medicine, Medical Education, Teaching & Learning in Medicine, and Medical Teacher. Student Lounges and Study Areas: In SPHPI, a cafè, vending machine area and a parenting room are located on the first floor. In addition, The Alan W. Donaldson Student Lounge as well as other lounge areas are provided for student use and are located on the first floor. Two group study rooms and five smaller interview rooms are also located on the first floor. Students may reserve these rooms by signing the reservation sheet located on the doors to each room. Common areas are also located on floors six, seven and eight of SPHPI. 13.1. Describe the program’s assessment plan, which should include the following elements: Statement of program objectives and intended learning outcomes; End- or near-end-of-program assessment of student learning, in addition to course-by-course assessment such as: (1) evaluation of capstone experiences (senior projects, recitals, exhibits, portfolios, etc.); (2) preand post-testing (value-added assessment) Multiple performance measures, if necessary, that reflect the uniqueness of the academic program and discipline such as: (1) standardized or other comprehensive examinations; (2) certification examinations; Feedback from key stakeholders (current students, alumni, employers, graduate schools, etc.); and Evidence of a formal feedback/improvement mechanism, i.e., that the program/unit has a regular review process in place and that the results of this process are used to improve curriculum, instruction, and learning. Overview of Program Assessment Plan Revised 2/17/2016 40 There will be multiple methods of ongoing evaluation for the MS in Clinical and Translational Science. Primary evaluation activities include: 1) Assessing student achievement as compared to the learning objectives for the program; 2) Examining student, graduate, and faculty satisfaction with the courses, curriculum, and teaching methods; and 3) Providing a feedback loop for implementing changes needed to continuously improve the program. Program assessment will also focus on the success of the program as measured by its attractiveness to candidates, the backgrounds and disciplines of those who attend the program, how well the program meets student needs, and graduates’ success postgraduation (as measured by involvement in clinical research, awards, and publication). Statement of Program Objectives and Intended Learning Outcomes The MS in Clinical and Translational Science is intended to train clinicians to become leaders in clinical and translational research. Students will learn the basic skills used by clinical researchers supplemented by a broad array of relevant electives that will provide the basic concepts and theories consistent with each student’s goals and objectives. Graduates of the MS in Clinical and Translational Science will be able to: have the skills to direct a broad range of clinical studies, particularly those that translate scientific knowledge into clinical practice; understand the basic analytical tools used by biostatisticians and epidemiologists; communicate their insights effectively; write well-conceived and persuasive grant applications; and ensure the ethical treatment of their subjects. Finally, as apprentice clinical investigators, they will learn how to participate in a broader multidisciplinary research community that includes basic and social scientists, as well as clinicians from other areas of clinical practice. At the end of the program, trainees will not be expert biostatisticians or survey researchers, for example, but they will be able to interact effectively with the complementary disciplines with which clinical investigators need to collaborate. Through didactic coursework, a series of workshops and seminars, and a mentored research project, the MS in Clinical and Translational Science will help to build a new generation of skilled clinician-investigators focused on improving population health through research. Measures of Student Learning Outcomes Students’ learning outcomes will be assessed initially on a course-by-course-basis when they are assigned a grade. The assessment of the more global goals of the program—the ability to integrate and apply to clinical research—will be assessed in the two culminating products of the program, the Masters thesis and the research grant application developed in HPA 590. Both of these products will require students to review and summarize Revised 2/17/2016 41 clearly what the state of the relevant areas of scientific knowledge and how this applies to clinical research. They will also need to be able to formulate clear research questions and develop analytic approaches including study design, ethical treatment of research subjects, epidemiology and biostatistics to answer these questions. Both the thesis and grant application will assess their written communication skills and their thesis defense will test their verbal ability to communicate scientific information clearly and persuasively. Feedback From Key Stakeholders (current students, alumni, employers, graduate schools, etc.) Throughout the program, there will be several opportunities to measure student and program success. For each course completed, students will complete Course Evaluation Questionnaires (CEQs), which provide students an opportunity to give feedback regarding the course content, the quality of faculty teaching methods, course materials and assignments, and relevance. In reviewing and modifying each course, these CEQs will be taken into consideration by the planning committees. Faculty will also be asked to complete evaluation forms regarding their impressions of the effectiveness of the curriculum and teaching methods. (See Section 12 for more information on student and teaching evaluation methods.) Upon completion of the MS, students will complete a Graduate Exit Survey, asking them to assess the overall quality of the curriculum and faculty, whether they found the program to be relevant and helpful toward their career path, and if the program fulfilled their expectations. In the years after graduation, the effectiveness of the in their new roles will be evaluated through questionnaires, one-on-one interviews, and observations of teaching and other professional activities. Other data will include the numbers and impact of published refered papers (frequency of citations) as well as abstracts, presentations, and participation in student advising. Finally, assessment process will include Alumni Surveys to determine what skills and knowledge acquired from the program are most valuable to trainees in their current professional roles, and what needs were not served through the program. These results will be reported periodically to the Curriculum Development Committee to guide change in the curriculum, teaching methods and faculty of the program. Evidence of a Formal Feedback / Improvement Mechanism An annual summary of trainees’ learning outcomes collected through direct measures and surveys will be reported to the Executive Committee and to Internal and External Advisory Committees to gauge the program’s progress. The Internal and External Advisory Committees will provide feedback and guidance for program improvement. The Internal Advisory Committee will assess progress the program has made towards meeting the identified objectives and will recommend corrective action when needed. The External Advisory Committee will be responsible for a comprehensive review of the program’s progress and guidance regarding any needed programmatic changes. In addition, the Curriculum Development Committee will identify trainee feedback and any modifications needed to improve the program. The recommendations from the various Revised 2/17/2016 42 committees will be discussed by the Executive Committee and will be incorporated into the program decision-making in the areas of curriculum, instruction, assessment, resources, and others as they are applied. Figure 2. Educational Evaluation for the MS in Clinical and Translational Science EDUCATIONAL EVALUATION REPORTING: Formative; Summative PROGRAM ADVISORY COMMITTEES EXECUTIVE COMMITTEE CURRICULUM COMMITTEE Clinical Research Training Program Internal Advisory Committee Members Sylvia Furner, PhD School of Public Health Sarah Kilpatrick, MD, PhD College of Medicine Christine Wu, PhD College of Dentistry JoEllen Wilbur, PhD College of Nursing Renee Taylor, PhD College of Applied Health Sciences William Beck, PhD College of Pharmacy Clinical Research Training Program External Advisory Committee Members Daniel Clauw, MD University of Michigan James Gordon, EdD, PT University of Southern California Philip Greenland, MD Northwestern University David Meltzer, MD, PhD University of Chicago Thomas Pearson, MD, PhD University of Rochester Second, the program is required to include the proposed MS program in the education programs reviewed by the Council on Education for Public Health (CEPH), the Revised 2/17/2016 43 accrediting body for the School of Public Health. Because the unit of accreditation for CEPH is the school, all degrees awarded from the school are considered to be from an accredited school/program, including those that come on line in the interim between regular accreditation reviews. Once the program is approved, the program will notify CEPH of the additional degree. CEPH will generally acknowledge this program and will review it in depth at the time of the next regular accreditation review. Thus, the MS in Clinical Research will be CEPH-accredited from the start and will be required to undergo a detailed review to identify program deficiencies. Third, IBHE will periodically assess the success of the program in meeting its objectives. This scrutiny will incorporate the broader perspective of the educational needs and priorities of the State of Illinois. 13.2. Identify measures to be used to assess and improve student learning, curriculum, and instruction. Evidence of success should include, but not be limited to, such specific outcomes as the following: Percent pass rate of graduates on end-of-program certification examinations; Enrollment of graduates in graduate and/or professional programs or other subsequent education; Percent of graduates employed in the field; Career advancement achieved by program graduates; Graduate/employer satisfaction with the program; Retention and graduation rates and time-to-degree completion; Percent of students involved in faculty research or other projects; and Percent of graduate students presenting or publishing papers. Baseline Data During the first year of the program, the following information will be gathered to establish baseline data: number of applicants, applicant backgrounds and disciplines, number of offers and number of acceptances. Through personal statements and interviews the program will assess student expectations and needs, so that it can examine how closely these were met upon completion of the program. The program will also work with potential trainees to develop a needs assessment through focus groups, questionnaires, and individual interviews. This information will be used to gauge the appropriateness and effectiveness of individual courses as well as the overall curriculum in meeting student needs, wants and expectations. Curriculum Evaluation Individual course evaluation will be performed using CEQs (Course Evaluation Questionnaires), as well as supplemental questions designed to address identified student expectations and needs. In addition, faculty will also be asked to complete evaluation forms regarding their impressions of the effectiveness of the curriculum and teaching Revised 2/17/2016 44 methods, as well as their perception of student progress. Seminars and workshops will be evaluated using Continuing Education evaluation forms and outcomes interviews. Immediate Outcomes At the end of each academic year, the following factors will be taken into consideration when evaluating program and student outcomes: student grades, attrition, pass rate and program completion. Through a questionnaire developed by the Evaluation Team, there will be an examination of whether the program met students’ perceived needs, and a request for student feedback on how the program could be improved upon or modified. These evaluations will include the following questions: 1. Did the program provide clear, concise objectives and goals? 2. Did the program promulgate the goals and objectives broadly as well as specifically to the applicants (pool)? 3. Do the candidates understand the goals and objectives? 4. Does the program address the stated goals and objectives? 5. Do the candidates accomplish the goals and objectives? 6. Does the program make a difference? Results from these various instruments will be compiled and presented to the Executive Committee, the Curriculum Development Committee, and the Advisory Committees. Longer Term Outcomes After graduation, the program will periodically follow up with graduates to assess their continuing success. Through exit and graduate surveys, the following information will be gathered to measure program success: projects funded, awards received, career advancement, and publications (including the numbers and impact of published refereed papers, frequency of citations, presentations and participation in student advising). Follow-up surveys will determine what skills and knowledge acquired from the program are most valuable to trainees in their current professional roles, and what needs were not met through the program. The program will evaluate the effectiveness of these trainees in their leadership roles through questionnaires, one-on-one interviews, and observations of teaching or other professional activities. As another way to measure program success, the program will identify a comparison group for the trainees by identifying the applicants who were accepted but did not attend or who dropped out shortly after starting the program. The program will follow up with this group as well as the MS group to compare each cohort’s performance, in terms of publications, scientific presentations and research funding (controlling for seniority), to study the program’s impact on its graduates. These results will be reported periodically to the Executive Committee to be used as support for changes in the curriculum, teaching methods, and faculty of the program. Revised 2/17/2016 45 A major goal of the CRTP is to increase clinical research capacity at UIC, and with this in mind, the program will track research funding and types of research funded at the university in the years following implementation to measure the effect of the CRTP on overall university activity in the fields of clinical and translational research. The program will be interested to see if it enables UIC faculty to upgrade their clinical research skills and provide new career opportunities for those whose inadequate training had hindered them before. UIC also hopes that the CRTP and its components, including the MS in Clinical and Translational Science, will support a “cultural” change in clinical departments to place higher importance on clinical research as part of the spectrum of valuable research. If the CRTP does successfully address the common challenge of creating multidisciplinary collaborations so crucial to clinical research, the program will explore the mechanisms though which this occurred. The program expects that demonstrated success at attracting candidates and increasing clinical capacity and research funding will encourage University Departments to commit the resources needed to allow trainees to enroll in the MS. OFF-CAMPUS PROGRAMS ONLY – Does not apply to this program. 14. In addition to responding to the above questions, if all or part of the proposed program is to be delivered off-campus and/or via the Internet, provide the following: Not applicable. 14.1. Describe the program’s mode(s) of delivery. 14.2. Describe the process for assuring the quality of the off-campus program in the following areas: (a) faculty qualifications and evaluation; (b) student access to necessary library resources; (c) where appropriate, student and faculty access to technical support, including computing. Has this program been approved for on-campus delivery? SOURCES Gwynne, Peter. “Job Market Outlook: Hot Careers for 2006” ScienceCareers.org November 11, 2005. Accessed from http://sciencecareers.sciencemag.org/career_development/previous_issues/articles/2005_ 11_11/job_market_outlook_hot_careers_for_2006/ on July 19, 2006. Zerhouni, EA. Translational and Clinical Science – Time for a New Vision. NEJM. 2005;353(15):1621-1623. Overview of the NIH Roadmap. NIH Roadmap for Medical Research. Available at http://nihroadmap.nih.gov/overview.asp. Accessed June 7, 2006. Buttrick, PM. CTSA Planning Grant Application. Revised 2/17/2016 46 Sung, NS, et al. Central Challenges Facing the National Clinical Research Enterprise. JAMA, 2003;289(10):1278-1287. Institute of Medicine Clinical Research Roundtable. Developing the Clinical Investigator Workforce: Clinical Research Symposium I. Washington, DC: National Academy of Sciences; 2001. Association of American Medical Colleges Task Force II on Clinical Research. The Role of Medical Schools and Teaching Hospitals in Maintaining a Robust Clinical Research Enterprise. Available at http://www.aamc.org/research/clinicalresearch/crtfcharge.htm. Accessed June 27, 2006. Association of American Medical Colleges. Task Force on Clinical Research: Executive Summary. Institutional Clinical and Translation Science Award - Request for Applications Number RFA-RM-06-002. Available at http://grants.nih.gov/grants/guide/rfa-files/RFA-RM-06002.html. Accessed October 17, 2005. The Illinois Commitment. A Citizens’ Agenda for Illinois Higher Education. State of Illinois Board of Higher Education. Available at www.ibhe.state.il.us. Accessed September 20, 2006. Zwanziger, J. K30 Proposal. PHS 298/2590. Bureau of Labor Statistics, U.S. Department of Labor, Occupational Outlook Handbook, 2006-07 Edition, Biological Scientists. Available at http://www.bls.gov/oco/ocos047.htm. Accessed August 10, 2006. Bureau of Labor Statistics, U.S. Department of Labor, Occupational Outlook Handbook, 2006-07 Edition, Medical Scientists. Available at http://www.bls.gov/oco/ocos008.htm. Accessed August 10, 2006. Illinois Career Information System. Biological Scientist. Available at http://www.ilworkinfo.com/icrn.htm. Accessed August 10, 2006. Illinois Department of Employment Security, Economic Information & Analysis Division. State of Illinois Occupational Employment Projections 2002-2012. Accessed August 10, 2006. MeetingsNet, April 4, 2001. Shortage of Clinical Trials Investigators Predicted. Available at http://meetingsnet.com/news/meetings_shortage_clinical_trials/index.html. Accessed June 27, 2006. Revised 2/17/2016 47 American College of Physicians. Is there a crisis looming in clinical research? ACP Observer. 2005. Available at http://www.acponline.org/journals/news/may05/research.htm. Accessed June 27, 2006. Revised 2/17/2016 48 Letter of Support from Medical Education, College of Medicine University of Illinois at Chicago College of Medicine Department of Medical Education September 6, 2006 To Whom It May Concern: As Head of the Department of Medical Education at the UIC College of Medicine and as a member of the Executive Committee of the UIC Clinical Research Training Program, I enthusiastically support the proposed MS in Clinical and Translational Science at UIC. In particular, I agree to the inclusion of MHPE courses in both core and elective courses. The National Institutes of Health and the Association of American Medical Colleges have identified clinical research training as a priority area for medical schools around the country, and I strongly support this program as part of a university-wide plan to increase clinical and translational research capacity. The College of Medicine has demonstrated a strong commitment to medical research – research programs have grown by over 20% per year over the past seven years, and we are ranked among the five fastest growing medical schools in terms of total funding awarded by the NIH over the past ten years. However, the research field is quickly changing, and there will be an increasing need for skilled clinician-researchers. The proposed MS in Clinical and Translational Science will broaden the training and skill sets of junior faculty and provide the College with new avenues for research and funding, while allowing us to remain competitive in the fields of medical education and research. The College of Medicine is pleased to offer our support and cooperation for the proposed MS in Clinical and Translational Science at UIC. Sincerely, Leslie J. Sandlow, MD Professor & Department Head Senior Associate Dean for Medical Education Revised 2/17/2016 49