Title: INTERNATIONAL CLASSIFICATION OF RADIOGRAPHS OF
advertisement

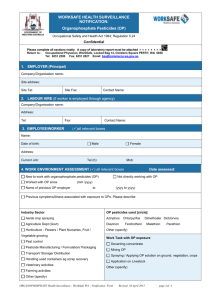
MARK D CURRICULUM FOR THE HEALTH SCIENCES IN SOUTH EASTERN EUROPE Number (unit, topic): U4-T4 Prior review – Status: D ECTS (suggested): Title Occupational Organophosphate Pesticide Poisoning Author(s) Institution Ass. Prof. Ivan Mikov, MD, PhD, Specialist in Occupational Medicine Department of Occupational Medicine, Medical Faculty, University of Novi Sad, Yugoslavia Department of Occupational Medicine, Medical Faculty, University of Novi Sad Futoska 121, 21000 Novi Sad, FR Yugoslavia Tel. + 381 21 613 998, 614 277, Fax: + 381 21 624 128 e-mail: driva@eunet.yu Address for correspondence Keywords Organophosphate pesticides, Organophosphorus compounds, Occupational poisoning, Cholinesterase, Worker, Health surveillance Learning objectives Synopsis (Abstract) Teaching methods Most organophosphate pesticides (OP) are used as insecticides, while a few are used as fungicides, nematocides or plant regulators. Since the removal of organochlorine insecticides from use, organophosphate insecticides have become the most widely used insecticides available today. All OP share a common mechanism of toxicity and can cause similar symptoms. - Introductory lecture with transparencies - Distribution of guidelines concerning Poison Control Centres - Presentation of occupational intoxication with organophosphate pesticide - clinical case report Specific recommendations for teacher . Assessment of students Written exam: multiple-choice questions Occupational Organophosphate Pesticide Poisoning Ivan Mikov, MD, PhD, Department of Occupational Medicine, Medical Faculty, University of Novi Sad, Novi Sad, Yugoslavia Chemical structure Most commercial OP are phosphorothioates since the P=S form is more stable and more lipid soluble than their oxidised form (P=O) - "oxon" which are much more toxic. Conversion occurs in the body, chiefly by the action of liver microsomes. Mechanism of toxicity OP exerts their toxic effect through inhibition (phosphorylation) of acetylcholinesterase enzyme (AChE) activity at nerve endings. AChE inhibition leads to accumulation of acetylcholine. Signs and symptoms of acute poisoning by site of acetylcholine neurotransmitter activity 1. Muscarinic - cholinergic neuroeffector junctions: nausea, vomiting, diarrhoea, salivation, lachrymation, bronchoconstriction, bronchorrhoea, bradycardia, miosis, blurred vision, urinary incontinence etc. 2. Nicotinic effects - skeletal nerve-muscle junctions and autonomic ganglia: muscle fasciculations, loss of reflexes, paralysis 3. Central effects - central nervous system: Headache, dizziness, behavioural disturbances, confusion, hallucinations, convulsions, loss of consciousness, respiratory depression etc. Diagnosis test procedures - Two types of cholinesterase are clinically significant: 1. Specific or true acetylcholinesterase found principally in the nervous system and the red blood cells. 2. Non-specific or pseudocholinesterase found principally in the plasma and the liver. The organophosphorus compounds inhibit both types, but the level of depression of specific or the red blood cell cholinesterase (RBC AChE) is a more reliable indicator of clinically significant reduction of cholinesterase activity. High RBC AChE inhibition is diagnostic of acute OP poisoning. - Severity of poisoning: Mild (RBC AChE > 40%) Moderate (RBC AChE 20% - 40%) Severe (RBC AChE < 20%) - Regeneration of cholinesterase There is regeneration of cholinesterase primarily by the synthesis of new enzyme, which takes place at the rate of approximately 1% per day. Treatment of acute poisoning - Airway protection - Skin decontamination - Atropine - administer i.v. or i.m. until signs of atropinization appear, effective only against muscarinic manifestations. - Pralidoxime - administer less than 48 hours after poisoning, reactivator of AChE. Warning: pralidoxime may actually be hazardous in poisonings by cholinesterase -inhibiting carbamate compounds - Seizure control and the other supportive therapy - Observation - ensure that symptoms do not recur as atropinization is withdrawn Chronic effects - Orgnophosphate-induced delayed neuropathy (distal symmetric sensorimotor neuropathy) - Central nervous system dysfunction - Dermatitis Prevention of poisoning - Personal protective equipment (respiratory protection, impervious protective clothing) - Preventive hygiene activities (consumption of food and smoking must not occur in work areas potentially contaminated with pesticides, washing of hands, face and neck prior to breaks, daily showers at the end of shift) - Health surveillance of workers Medical aspects of the occupational health program should parallel the hygiene activities. Preplacement medical examinations should include measurement of RBC AChE activity for determination of a preexposure baseline because of high interindividual variability. Periodic medical examination should be made available on at least an annual basis. But, measurement of RBC AChE activity in workers exposed to organophosphate pesticides should be available at more frequent intervals depending on workplace hygienic surveys. References: 1. Moretto A, Lotti M. Toxicity of pesticides. In: Stacey NH (ed.). Occupational toxicology. Bristol: Taylor& Francis, 1995:177-204. 2. Reigart RJ, Roberts RJ. Organophosphate insecticides. In: Reigart RJ, Roberts RJ. Recognition and management of pesticide poisonings. Washington DC: U.S. Environmental Protection Agency, 1999: 34-47. 3. Mikov M, Jovanovic D, Jokanovic M, Mikov I, Mihajlovic G. Pesticide protection, first aid and management of poisoning. Belgrade: Nova prosveta, 1997, 46pp. (in Serbian) 4. Legaspi JA, Zenc C. Occupational health aspects of pesticides. In: Zenc C (ed.). Occupational medicine. New York: Mosby, 1994: 617-46.