General exam formDC 6-07 - MidWest Clinicians` Network
advertisement

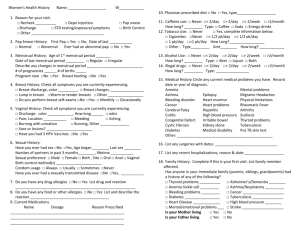
GENERAL EXAM FORM Revised 04/22/05, 06/15/07 Date __________________________ Name: _____________________________________ Age: ______ Sex:_______ Smokes________ PPD______ Allergy: ____________________________________Alcohol _____________Illicit Drugs_________________ Meds: Changed since last visit No change since last visit B/P_____/______ P______ Regular Irregular RR______ Labored Non-Labored Temp ______ Weight_________ Height _______ Last Pap___________ Hyst _________ Tubal ________________ HgbA1c __________ Blood Sugar ____________ Fasting / Random Microalbumin ________ BMI _________ Last Retinal Eye Exam _______________ Last Testicular Exam _________________ Chief Complaint/HPI: Pain Scale:___________ Peak Flow __________ (avg. of 3) Pulse Ox ____________ ____________________________________________________________________________________________________ ____________________________________________________________________________________________________ ____________________________________________________________________________________________________ _______________________________________________Signature of Screening Nurse______________________________ Review of Systems Legend ( О = Positive Finding / = Negative Finding Blank = Not asked) Constitutional: fever, chills, fatigue, wt change____#, night MS: bone pain rating_____(1-10 scale), location _________, sweats duration________, radiates _________, quality (sharp, achy, HEENT: visual changes, hearing loss, rhinorrhea, sore throat, dull, throbbing), intermittent/ constant, myalgias/arthralgia oral ulcers/lesions, dry mouth, postnasal drip, dry eyes, (edema, warmth, erythema) __________, joint__________ allergies (seasonal, ______________) Renal: hematuria, dysuria, increased freq, nocturia, hesitancy, GI: nausea, vomiting, diarrhea ____BM’s/day, watery, bloody, groin pain (colicky), flank pain mucous, melena, BRBPR, constipation, abd pain rating_____ Neuro: paresthesias, imbalance, hand/foot numbness, shooting (1-10 scale), ____quad, sharp, dull, throbbing, crampy, pains ____(1-10 scale), diploplia, dysarthria, hearing loss, _________ radiates _________________worse with dysphagia, anosomnia, amarosis fugax, headache ______(1-10 _____________ positional ____________________ scale), dull, sharp, shooting, constant, intermittent, occipital, Pulmonary: dyspnea (rest/exertion), orthopnea, PND, LE temporal, parietal, frontal, neck, behind eye, duration edema, cough (dry, sputum ____), worse at night, snoring _____________, aggravating/alleviating factors Cardiovascular: chest pain rating ____(1-10 scale), ________________, wake you in the middle of the night; location________, duration_____, radiates _________ sharp, Yes/No. HA associated with; scotomas, tongue biting, nausea, dull, achy, heavy, tight, started suddenly, over hours, over days. postictal, incontinence, witnessed. _________________ positional; worse with climbing stairs, walking, rest, breathing weakness location _____________ duration _______ deeply, lying flat, better with ____________ GU/GYN: dyspareunia, discharge, lesions, nodules, H/O STD Endocrine: polyphagia, polydypsia, polyuria, dry skin, brittle ___________, incontinence, urine/stool (sneeze, laugh, urge, hair, tremors, heat/cold intolerance, depression, irritability, leakiness, hesitancy, dribbling, erectile dysfunction, am hand numbness, nipple discharge (milky, bloody, clear) tumescence, LMP________ duration ______ regular/irregular Hematology: bleeding, easy bruising, petechiae, freq Psychiatric: depression, anxiety, SI, HI, insomnia, change in infections, hemearthosis, lymphadenopathy appetite, difficulty concentrating, anhedonia, grandiose Dermatology: rash, pruritic, moles (changed in color, size), delusions, hallucinations, visual/verbal acne ______________________ ADL’S ___________________________________________ Sexual History: ____________________________________ History: Changes in history: Past Medical history reviewed and updated with patient _________________________________________________ Past family history reviewed and updated with patient _________________________________________________ Past social history reviewed and updated with patient _________________________________________________ Physical Exam General: CV: HEENT: GI: Derm: GU/GYN: Neck: Rectal: Pulmonary: Neuro: Breast: Extremity: Lymph: MS: Signature of Provider ___________________________________________ Process: To be used on initial (non-acute) visit and at discretion of provider for other visits. Filed in chart under progress note in chronological order, with newest on top. GENERAL EXAM FORM Name: _______________________________________ Assessment: ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ Plan: ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ _____________________________________________ Labs Ordered: _________________________SMMC Voucher / Order _________________________SMMC Voucher / Order _________________________SMMC Voucher / Order _________________________SMMC Voucher / Order _________________________SMMC Voucher / Order Diagnostics Ordered: ____________________________DH Voucher / Order ____________________________DH Voucher / Order ____________________________DH Voucher / Order ____________________________DH Voucher / Order ____________________________DH Voucher / Order Medication changes: ____________________________________PAP / ____________________________________PAP / ____________________________________PAP / ____________________________________PAP / ____________________________________PAP / ____________________________________PAP / ____________________________________PAP / ____________________________________PAP / ____________________________________PAP / ____________________________________PAP / ____________________________________PAP / Discontinued Medications: ____________________________________ ____________________________________ ____________________________________ ____________________________________ ____________________________________ ____________________________________ Rx Rx Rx Rx Rx Rx Rx Rx Rx Rx Rx Revised 04/22/05, 06/15/07 Date: ________________________ Referral given to: ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ Referral to Social Service: _______________________ PAP: _________________________________________ Dietician: _____________________________________ Educator:_____________________________________ Stressed importance of keeping referrals/appts Other Instructions: Diet Type: Low Cholesterol Low Salt 2000mg Sodium Diet 1200 Cal ADA ________Cal ADA Other ___________ Activity Changes: Walk 30 min daily Walk as tolerated Continue current routine Other ______________________________________ Monitoring: 1 2 3 4 _________ times daily blood sugars fasting (goal 80-120) before meals (goal less than 120) 2 hrs after a meal (goal less than 140) Mail or bring in to office after 2 weeks Self Management Goals: Stop Smoking Wt loss of _________ pounds per week Other ______________________________________ Patient Response to Teaching and Discharge Instructions listed on this form. Verbalized Understanding Repeats Instructions Other Comments_____________________________ _____________________________________________ Signature of Discharge Nurse_____________________________________ Discharge Instruction: Return for: FU Annual HP Pap Procedure ____________ Other __________ In ______Days_____Weeks_____Months _____Year Refill Routine Meds for: 1 mo 3 mo 4 mo 6 mo 1yr Other _______________ Signature of Provider ___________________________________________ Process: To be used on initial (non-acute) visit and at discretion of provider for other visits. Filed in chart under progress note in chronological order, with newest on top.