Albert Einstein Healthcare Network
advertisement

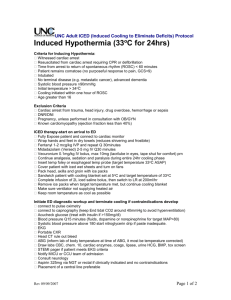
Therapeutic Hypothermia Protocol Albert Einstein Healthcare Network Therapeutic Hypothermia Clinical Guideline Post Cardiac Arrest Subject: Primary Responsibility: Policy Location: INDUCED HYPOTHERMIA Post-CARDIAC AREST Medical Staff Policy Effective Date: Review / Revision Dates: Albert Einstein Healthcare Network: Critical Care/ED Purpose: To provide clinical practice guidelines for the induction and maintenance of mild to moderate controlled, therapeutic hypothermia on adult patients who sustain cardiac arrest and are successfully resuscitated and meet all of the inclusion criteria and do not meet any of the exclusion criteria. Policy Statement: Albert Einstein Healthcare Network will provide induced hypothermia to patients under a safe condition when medically appropriate. Definitions: “Induced Hypothermia” is therapeutic hypothermia after cardiac arrest for the unconscious adult who exhibits return of spontaneous circulation following resuscitation after cardiac arrest. This process involves cooling the patient to 32° Celsius to 34° Celsius with external cooling devices as well as ice-water gastric lavage and cold saline infusions as clinically appropriate. “ROSC” means Return of Spontaneous Circulation. “Mild Hypothermia” is defined as body temperature of 33-36 Celsius (91.4-96.8 Fahrenheit) “Moderate Hypothermia” is defined as body temperature of 28-32 Celsius (82.4-89.6 Fahrenheit) “Refractory Hypotension” is defined as the need for more than 2 vasopressors. 1 TBD Therapeutic Hypothermia Protocol “Passive Rewarming” is defined as the removal of cooling devices to allow the patient to rewarm by environmental influence. “Controlled Rewarming” is defined as controlling the rewarming process by slowly rewarming the patient by a gradual increase in water temperature of the surface cooling pads over a set period of time or at a set interval of degrees Celsius per hour. Procedure: 1. Hypothermia will only be induced on patients meeting inclusion criteria following successful cardiopulmonary resuscitation in the emergency department, prior to arrival in the emergency department or while on a medical or surgical floor or critical care area in accordance with ACLS guidelines. 2. Therapeutic hypothermia will be initiated on patients in a comatose state following return of spontaneous circulation with maintenance of stable perfusing cardiac rhythm for a duration >/= 20 minutes. 3. For patients who maintain return of spontaneous circulation (ROSC) greater than 20 minutes from initial resuscitation and meet inclusion criteria, therapeutic hypothermia protocol is initiated as clinically appropriate. 4. Hypothermia will be induced upon written physician order on appropriate patients as soon as possible by the emergency medicine, critical care or other attending physician or their designee and continued with maintenance of patient temperature within range of 32340 C for a period of 24 hours as clinically appropriate. 5. Hypothermia will be maintained in all procedural areas (MRI testing is contraindicated during hypothermia). 6. Hypothermia will be induced pursuant to applicable clinical practice guidelines. 7. Physician consultations will include Cardiology, Neurology, and Critical Care/Pulmonology. Approved by: Review / Revision Chief Nurse Executive: Date: Legal: Date:_____________ ______________ ___________ Shared Governance: Date:_____________ ______________ ___________ Department of Medicine: Date:_____________ ______________ ___________ 2 Therapeutic Hypothermia Protocol CLINICAL PRACTICE GUIDELINES FOR INDUCED HYPOTHERMIA POSTCARDIAC ARREST Exclusion Criteria: 1. Within 14 days of other major operative procedure (not including cardiac catheterization). 2. Active bleeding or pre-existing severe coagulopathy 3. Shock state (s) unresponsive to pressor/vasoactive agents. 4. Major Head Trauma/multisystem trauma with increased bleeding risk. 5. Known or suspected sepsis (relative contraindication). 6. Hemodynamically significant cardiac dysrhythmias or QTc interval greater than 470 ms before hypothermia initiation 7. Not to be initiated if Return of Spontaneous Circulation (ROSC) time was greater than 60 minutes from initiation of CPR 8. Arrest (VT/VF, asystole, PEA) secondary to sepsis. 9. Clinical indicators of a coagulation disorder. TH may be initiated without platelet count as long as the patient does not have a history of hematologic disorder or other condition associated with thrombocytopenia such as malignancy, immunosuppression/chemotherapy or severe liver disease with concurrent bleeding. 10. Comatose state or minimal pre-morbid/pre-arrest cognitive status. 11. “Do not resuscitate” status or terminal illness prior to cardiac arrest. 12. Greater than 6 hours elapsed from time of ROSC. Inclusion Criteria: 1. Hypothermia must be started ASAP after ROSC. 2. Persistent coma as evidenced by no eye opening to pain after resuscitation (no waiting period required). GCS less than 8 or not obeying verbal commands 3. ROSC from pulseless state (e.g. ventricular tachycardia / fibrillation, asystole, PEA) 4. ROSC within 60 minutes from time of initiation of CPR 5. Patient requires mechanical ventilation. 6. Blood pressure can be maintained greater than or equal to MAP 70-80 mm HG spontaneously, with intravascular volume and stable dosing of vasoactive/inotropic agents. 7. Pregnancy NOT a contraindication to TH. Focus of care is to preserve life of the mother. Immediately reportable conditions during therapeutic hypothermia: 1. Ventricular tachycardia or fibrillation 2. Asystole 3. Sustained SVT 4. Refractory hypotension: Rewarming cautiously, treat initially using fluid challenges. 5. Uncontrolled bleeding. 3 Therapeutic Hypothermia Protocol 1. If patient successfully resuscitated from additional interval of VT/VF during hypothermia protocol, 24-hour interval of maintenance hypothermia is re-started from that point. 2. Rewarming is begun at 24 hours after reaching patient target temperature during hypothermia protocol. a. During rewarming, the goal is to increase the temperature at 0.33° Celsius per hour over a span of eight to twelve hours or until the patient reaches normothermia (36.5° Celsius). b. Rewarming is controlled by the approved cooling device or is performed by passive rewarming in emergent situations. c. Controlled rewarming is preferred due to the variable environmental influence of passive rewarming which may allow the patient to rewarm too quickly placing them at higher risk for hyperkalemia and hypotension. ***TO FACILITATE TRANSFER TO CCU/ICU, NOTIFY BED-BOARD AND CCU SENIOR/ICU SENIOR AS CLINICALLY APPROPRIATE.** Materials: To be available in all areas initiating therapeutic hypothermia 1. Internal temperature monitoring device such as esophageal temperature probe. 2. Module for Temperature monitoring 3. Approved cooling device 4. Peripheral nerve stimulator 5. Nasogastric Tube 6. Lubricant 7. 60mL cath-tip syringe 8. Rectal thermometer 9. Triple lumen catheter and sterile materials for insertion 10. Arterial line kit and sterile materials for insertion 11. Cold (approximately 4 degrees Celsius) Normal Saline as ordered. Chilled normal saline will be prepared upon identification of potential candidates meeting inclusion criteria by the following method. In a washbasin, fill halfway with an ice/water mixture, immerse two, one-liter bags of normal saline for a period of 15-20 minutes. At the end of this interval, the temperature of the normal saline is approximately 3-4 degrees Celsius. **STEPS 1-10 SHOULD BE COMPLETED AND STEPS 11 & 12 INITATED IN EMERGENCY DEPARTMENT PRIOR TO TRANSFER TO CRITICAL CARE UNIT** ******Item 11 not utilized for patients receiving therapeutic hypothermia induction in ED via thermosuit.******** A. Initial Cooling Phase: 1. Once hypothermia eligibility is confirmed, and hypothermia orders obtained, obtain all the above materials. 4 Therapeutic Hypothermia Protocol 2. Maintain ventilator support as ordered to keep oxygen saturation ≥92% unless otherwise ordered. 3. Insert internal temperature monitoring probe (such as esophageal temperature probe) or alternative temperature monitoring device. 4. Ensure peripheral IV patency, if not present or patent, place new peripheral IV. 5. Insert and maintain multiple (2) large-bore peripheral IV catheters. 6. Obtain and document core temperature (e.g. esophageal or rectal) prior to hypothermia induction. 7. Obtain baseline labs (if not previously done) as ordered. a. CBC, Platelets, PT, PTT, Metabolic profile, CPK-MB, Troponin, Lactate, Fibrinogen, D-Dimer, ABG (notify respiratory of patient temperature) 8. Obtain EKG (if not previously done). *****If patient receiving therapeutic hypothermia induction in ED via thermosuit skip to step # 16. ***** 9. After establishing GI access with insertion of nasogastric or orogastric tube, lavage stomach with 500-750 mL ice water as needed to lower body temperature by the following method. Instill 500-750 mL ice water through GI access and leave in place for 30 min. Place GI access to suction and aspirate to empty stomach contents. Re-instill 500-750 mL ice water and leave in stomach for 30 min. Repeat as needed to assist in lowering body temperature. 10. Rapidly administer cold (4 degrees Centigrade) normal saline infusion using pressure infuser bags as ordered. Cold NSS should be administered as rapidly as possible through the largest-bore IV access available in a given patient. Volume of cold NSS administered per physician order. Volume of chilled NSS administered is weight-based. If patient admission weight is greater than 60 kg, 2 L chilled NSS to be administered rapidly IV on initiation of protocol. If patient admission weight 60 kg or less, 1.5 L chilled NSS to be administered rapidly on initiation of protocol. 11. If cardiac arrest is complicated by or presents with congestive heart failure or pulmonary edema, reconsider use of chilled saline rapid infusion to avoid additional complications associated with fluid overload. 12. Utilize surface cooling device on patient (per manufacturer’s instructions). 13. Attach cooling pad (s) to approved cooling device (per manufacturer’s instructions). 14. Activate cooling system with temperature set to 33° Celsius. 15. Utilize additional surface cooling as appropriate to reach target temperature. Additional surface cooling may consist of application of towels to patient torso and legs after towel saturated with cold water. 16. Monitor and record vital signs (blood pressure, temperature, heart rate, rhythm, oxygen saturation, respiratory rate) unless otherwise indicated: a. Continuously monitor temperature and document once per hour. b. Every 15 minutes times 4 c. Every 30 minutes times 2 5 Therapeutic Hypothermia Protocol d. Every hour 1) Maintain Mean Arterial Pressure (MAP) ≥70-80 mm Hg with IV vasopressors and inotropes as ordered. 2) Monitor patient for arrhythmias (most common is bradycardia). If significant dysrhythmias, Hemodynamic instability or bleeding develops, then active cooling should be discontinued. 17. Protocol start/stop times and re-warming phase are documented in progress notes and in nursing documentation/electronic flowsheet. 18. Administer medications as ordered. a. Sedation: 1) Obtain and document Sedation/Agitation Scale score (SAS) with vital signs during sedation administration. 2) Bolus with sedation as ordered and then titrate continuous sedation infusion to a SAS of 2-3 unless otherwise ordered. SAS goal prior to initiating neuromuscular blockade is SAS-1. i. Sedation/Agitation Scale: Sedation-Agitation Scale (SAS): 1-7. SAS-7: Dangerous agitation: Pulling at airway/catheters, climbing OOB, threat to staff/ others SAS-6: Very agitated: Requires restraint, frequent verbal limit-setting, biting ETT. SAS-5: Agitated: Anxious/physically agitated, calms to verbal instructions. SAS-4: Calm and cooperative: Calm, easily arousable, follows commands. SAS-3: Sedated: Difficult to arouse, awakens to verbal stimuli or gentle shaking. May follow simple commands then drift off to sleep. SAS-2: Very sedated: Arouses to physical stimuli, does not communicate or follow commands. May move spontaneously. SAS-1: Unarousable: Minimal/no response to noxious stimuli, does not communicate/follow commands. With documented depression of consciousness/increased sedation level (i. e. SAS-1), initiate neuromuscular blockade as early as possible during induction phase. Initiate bispectral index (BIS) monitoring as quickly as possible in ICU or CCU for patients receiving sedation/analgesia alone as well as patients receiving sedation/analgesia with neuromuscular blockade. Titrate sedation/analgesia throughout therapy to maintain BIS value between 50 and 60 on linear scale. If BIS value sustained above 60 for greater than 15 minutes re-bolus with sedative agent at dose equal to infusion rate. If BIS value remains greater than 60, administer additional bolus and increase infusion rate. Neuromuscular blockade: Follow clinical practice guidelines for monitoring/maintenance of neuromuscular blockade (NMB) therapy. Goal of neuromuscular blockade therapy is determined primarily by degree to which clinical endpoints (ventilator synchrony, eliminating shivering, etc...) are met. Obtain/document baseline train of four prior to paralytic administration if possible. 6 Therapeutic Hypothermia Protocol Once paralytics are administered a standard goal of treatment is 2 twitches. Degree to which clinical endpoints are met is primary when titrating NMB therapy. Bolus with paralytic as ordered, initiate infusion and titrate to abolish and prevent shivering and/or to maintain respiratory rate at set rate of ventilator or prevent patient-ventilator dys-synchrony. Obtain and document train of four: o 15 minutes after paralytic bolus o 15 minutes after every dosage change o A minimum of every 2 hours until clinically stable o Every 4 hours to goal of less than 2 twitches while continuous paralysis is maintained unless otherwise ordered. o Note: Train of four neuromuscular responsiveness is diminished during hypothermia. If patient has no train of four responses and meets clinical endpoints, decrease NMB infusion dose per order set and reassess train of four and clinical endpoints (shivering/ventilator synchrony). Administer lacrilube ointment as ordered to both eyes while sedation/analgesia and neuromuscular blockade is being administered during TH. Prepare for and assist in insertion of arterial line for blood pressure monitoring as ordered. Prepare for/assist in use of flo-trac arterial line for cardiac output monitoring as clinically appropriate. Prepare for and assist in insertion of pre-sep triple lumen catheter central venous catheter. Prepare for/assist in use of CVP/SCVO2 monitoring if not already ordered. Prepare for and assist in insertion of Pulmonary artery catheter as ordered. Place a nasogastric tube to low intermittent wall suction (except when giving medications) DVT prophylaxis B. Maintenance Hypothermia Phase: 19. Obtain and document a second route of temperature every 2 hours (e.g. rectal or temporal). 20. Watch and document trends in water temperature of the cooling pads at a minimum of 2 hours. a. Significant increases and decreases in water temperature in the cooling pads may indicate changes in patient’s core temperature, which may prompt further investigation for cause. 21. Perform full skin assessment every 2 hours paying special attention to potential injury that can occur from the cooling pads. 22. Perform ordered labs at 6 hours, 12 hours, and 18 hours after initiation of protocol as ordered. a. CBC, Platelets, PT, PTT, Metabolic profile, CPK-MB, Troponin, Serum Lactate, Liver Function Tests, Surveillance Blood Cultures , ABG (notify respiratory of patient temperature) as ordered 7 Therapeutic Hypothermia Protocol 1) Hypothermia commonly causes hypokalemia, when patients are rewarmed, Hyperkalemia may occur. 2) All ABG measurements must be analyzed at the patient’s actual body temperature. Arterial CO2 should continue to be maintained between 35-45. 3) Blood cultures are drawn at 12 hours after the initiation of cooling due to infection that may be masked during the cooling phase. C. Rewarming Phase: Begin 24 hours after patient reaches target temperature (32-340 C. Controlled Rewarming (Preferred): 23. Keep surface cooling device in place. 24. Set approved cooling device machine to re-warm over 12 hours (approximately 1 degree C every 3 hours) to a temperature of 36.5 °Celsius. 25. Continuously monitor vital signs (temperature, BP/HR/RR). Document once per hour and as clinically appropriate. 26. If NMB/sedation not titrated off at this stage discontinue NMB first. a. Recovery of neuromuscular function is documented when train of four returns to four twitches on the originally documented stimulus (Hz) level and patient may trigger ventilation and exhibit brainstem reflexes/response to stimulation. 27. Maintain patient temperature with cooling devices at 36.5° Celsius for an additional 24 hours. 28. Monitor and record Glasgow Coma Score every 2 hours for 48 hours. 29. Monitor closely for hyperkalemia during rewarming phase. a. Hypothermia commonly causes hypokalemia, when patients are rewarmed, Hyperkalemia may occur. Post-rewarming phase: MAINTAINING NORMOTHERMIA: Rebound hyperthermia is a risk factor for further neurologic damage post cardiac arrest. Cooling unit will be maintained on patient in “monitor” mode at conclusion of rewarming phase. If patient temperature increases to greater than 37.7 degrees Centigrade, cooling measures to maintain normothermia will be initiated. Patient Management. 1. Normothermia will be maintained continuously for up to 72 hours at which time the need for ongoing temperature control will be reassessed. 2. Should the patient subsequently develop a refractory fever over the next 24 hours, reinduction of normothermia will be considered at the discretion of the Physician team. 3. Administer acetaminophen per physician order. 8 Therapeutic Hypothermia Protocol References: 1. Andrews, J. P. (2005). Hot or cold? Warm heart, cold brain. Hospital Medicine, 66(2). 80-83. 2. American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, "Part 7.5: Postresuscitation Support." Circulation 112, 11/28/2005 IV84-IV-88. 06/19/2006 < http://circ.ahajournals.org/cgi/content/full/112/24_suppl/IV-84 >. 3. Commichau, C., Scarmeas, N., Mayer, S.A. (2003). Risk factors for fever in the neurologic intensive care unit. Neurology, 60, 837-841. 4. Diringer, M.N., Reaven, N.L., Funk, S.E., Uman, G.C. (2004). Elevated body temperature independently contributes to increased length of stay in neurologic intensive care unit patients. Critical Care Medicine, 32 (7), 1489-1495. 5. Fekberg, R.A., et al. “ Hypothermia after cardiac arrest: Feasibility and safety of an external cooling protocol.” Circulation. 104. 7/31/2001 1799-1804. 2/17/2006 <http://circ.ahajournals.org/cgi/content/full/104/15/1799>. 6. Keresztes, P.A., Brick, K. (2006). Therapeutic hypothermia after cardiac arrest. Dimensions in Critical Care Nursing, 25(2), 71-76. 7. Kochanek, P.M., et al (2004). Therapeutic hypothermia in resuscitation: The Safar vision. ITACCS, 49-52. 8. Lasatar, M. (2005). The role of thermoregulation in cardiac resuscitation. Critical Care Nursing Clinics of North America, 17, 97-102. 9. Ly, H. Q., et al, (2005). A pilot study: The noninvasive surface cooling thermoregulatory system for mild hypothermia induction in acute myocardial infarction (The NICAMI Study) American Heart Journal. 933, e9-e13. 10. Maramarrom, B. V., Wijdicks, E.F.M. (2005). Postresuscitation encephalopathy: Current views, management, and prognostication. The Neurologist, 11(4), 234-243. 11. Nordmark, J., Rubertsson, S., (2005). Induction of mild hypothermia with infusion of cold (4°C) fluid during ongoing experimental CPR. Resuscitation, 66,357-365. 12. The Hypothermia After Cardiac Arrest Study Group, (2002). Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. The New England Journal of Medicine. 346, 549-563. 13. Varon J, Acosta, P. Therapeutic hypothermia: Past, Present and Future. Chest 2008; 133: 1267-1274. 14. Zeitzer, M. B. (2005) Inducing hypothermia to decrease neurological deficit: literature review. Journal of Advanced Nursing 52(2), 189-199. 15. Holzer M. Targeted temperature management for comatose survivors of cardiac arrest. N Engl J Med. 2010; 363: 1256-1264. 16. McKean S. Induced moderate hypothermia after cardiac arrest. AACN Advanced Critical Care. 20(4):342-353. 9