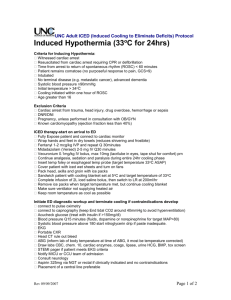
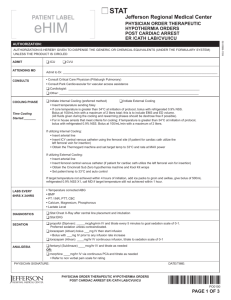
Supplemental Figure 1. Therapeutic hypothermia protocol for CODE
advertisement

Supplemental Figure 1. Therapeutic hypothermia protocol for CODE ICE and STEMI on ICE patients 1. Temperature monitoring a. Place an esophageal temperature probe (preferred) or rectal temperature probe b. When a Foley catheter is inserted, use a temperature-sensing catheter if available 2. Hypothermia induction a. Pre-hospital hypothermia protocols may vary among EMS systems; most use ice packs and/or IV saline (chilled or room temperature) i. On arrival at hospital, place core temperature probe if needed ii. Apply external cooling (circulating water) pads if prehospital cooling was performed b. If no pre-hospital cooling, initiate cooling with ice packs and chilled saline while preparing for external cooling pad use c. For direct transfer to cath lab: i. Continue ice packs and saline, if initiated ii. Place temperature probe iii. Apply external cooling pads d. For direct transfer to CVICU: i. Apply external cooling pads ii. Place temperature probe iii. Consider ice packs and saline if not hypothermic on arrival e. Target temperature should be maintained at 32-34 ºC for 24 hours from the time of the initial cardiac arrest 3. Neuromuscular blockade (recommended for all therapeutic hypothermia patients) a. Vecuronium 0.1 mg/kg IV bolus b. Repeat vecuronium 0.1 mg/kg IV bolus in one hour if needed (may be earlier if patient demonstrating evidence of inadequate paralytic effect) c. Initiate continuous infusion cisatracurium 3 mcg/kg/min, titrated to trainof-four (TOF) 4. Sedation a. Place a bispectral index (BIS) monitor. b. Fentanyl 100 mcg IV x1, then start infusion at 100 mcg/hr, titrating to BIS ≤50 c. Fentanyl 100 mcg IV q5 minutes PRN d. Midazolam 2 mg IV q5 minutes initially until unresponsive to painful stimulation and for BIS ≥ 50 e. Midazolam 2 mg IV bolus q5 minutes PRN 5. Cardiovascular/hemodynamic considerations a. Sinus bradycardia is the anticipated rhythm; unnecessary to treat unless clinical sequelae are present. If treatment is necessary, consider increasing target temperature or temporary pacing b. The electrocardiogram may show Osborn waves and/or QT-prolongation; these do not require specific treatment c. Ventricular fibrillation caused by hypothermia is rare at temperatures ≥ 32ºC d. Mean arterial pressure target is 80-90 mmHg to maintain adequate cerebral perfusion pressure; recommend norepinephrine as the vasopressor of choice for hypotension; consider adding vasopressin as needed if SVR remains < 1200 e. Consider early ventricular mechanical support for cardiogenic shock f. For hypertension, consider treatment with nitroglycerin or nicardipine infusion g. Arterial line placement and central venous access is recommended. Consider PA catheter placement for hemodynamic instability or heart failure h. Avoid hypovolemia; hypothermia may induce diuresis 6. Metabolic considerations a. Oxygen consumption decreases by ~8% per ºC fall in temperature b. Anticipate hypokalemia during hypothermia; not necessary to treat unless level is below 2.8 mEq/L or arrhythmias are present c. Hyperglycemia is common during hypothermia due to decreased insulin release; liver glycogen stores may also be reduced i. Vasoconstriction may cause finger-stick accuchecks to be inaccurate ii. Recommend target glucose less than160 mg/dL while hypothermic d. Target magnesium level is 2 mEq/L or greater; if level is below target, give magnesium sulfate 4 grams IV and consider further supplementation e. Hypophosphatemia may occur due to increased renal excretion i. May increase infection risk and reduce ability to wean from mechanical ventilation 7. Acid-Base Disturbances a. Hypothermia shifts the oxyhemoglobin dissociation curve, resulting in oxygen saturation at a lower oxygen partial pressure and less tissue oxygen extraction b. CO2 production is decreased, leading to an initial respiratory alkalosis during cooling. This can cause cerebral vasoconstriction and decreased cerebral perfusion pressure c. Lactic acidosis may occur during mild hypothermia d. Knowledge about the normal partial pressures of gases at varying temperatures is limited i. In hypothermia, PO2 and PCO2 are overestimated, pH is underestimated ii. To correct, subtract 5mm Hg PO2 and 2mm Hg PCO2 and add 0.012 pH units for each degree below 37ºC iii. General consensus is not to correct arterial blood gases for temperature iv. To avoid respiratory alkalosis, target PCO2 should be 45-50 and pH 7.35 8. Neurological considerations a. Consider electroencephalography if seizures are suspected b. BIS and TOF monitors are recommended to improve sedation 9. Other considerations a. Hypothermia impairs leukocyte function, increasing risk of infection b. Hypothermia impairs platelet function, possibly increasing risk of bleeding c. Document bowel sounds every 2-4 hours and gastric residuals per nursing protocol d. Avoid medications labeled “do not refrigerate” (e.g.mannitol) which may precipitate if cooled 10. Rewarming Phase a. Rewarm slowly using the external pads at a rate of 0.25ºC per hour b. Leave external cooling pads on for a minimum of 12 hours after normothermia is achieved. If temperature is labile, continue to use external cooling pads to maintain normothermia c. Anticipate hypotension during rewarming phase secondary to vasodilation d. Anticipate a rise in potassium levels, a drop in glucose levels, and a decrease in arterial pressure during rewarming e. Neuromuscular blockade may be discontinued when patient temperature ≥ 36 ºC. Wait at least two hours before weaning sedation. 11. Caregiver/Family Education a. Educate caregiver/family at the level of their understanding of the following: i. Indications and rationale for therapeutic hypothermia ii. Indications and rationale for sedation and paralytics iii. Effects of therapeutic hypothermia on body systems and measures implemented to support or protect body systems iv. Length of time patient will be cooled v. Risks associated with rewarming and steps taken to support patient during rewarming b. Consult the Palliative Care Service, regardless of the expected outcome