presentation describing the project.
advertisement
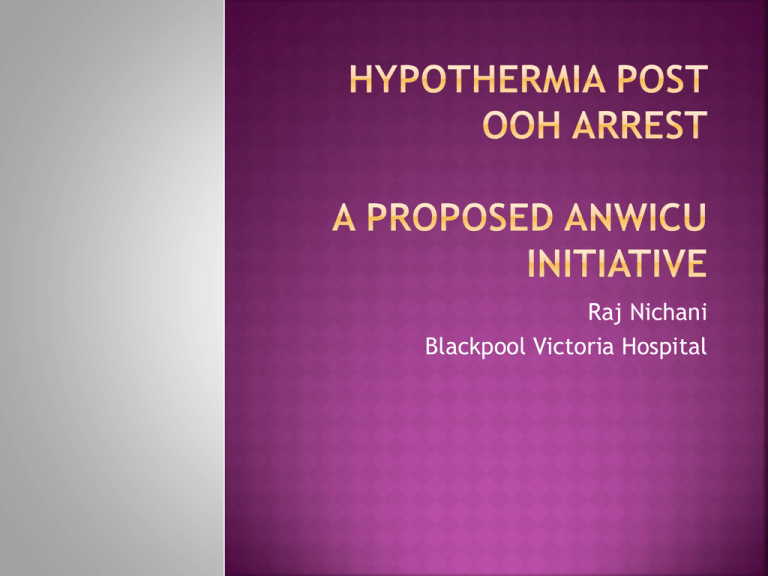
Raj Nichani Blackpool Victoria Hospital Strengthen collaboration across the region Spread good practice Develop exists. on the tremendous potential that Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-ofhospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–563. The Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–556. How good are we with putting this evidence into clinical practice. Do we achieve similar results outside the settings of RCT’s. Audit Good of our practice in Blackpool success with the use of therapeutic hypothermia Outcomes 12 10 died during cooling inadequately cooled not cooled 8 6 4 2 VF ie d D VF su rv iv ed 0 cooled All survivors were discharged with good neurological recovery What was everyone else doing across the region/nationally with cooling? Were basic minimum standards being achieved? Was any particular method better/more eficient? Were other hospitals having similar outcomes? Are patients being subjected to unacceptable variations in practice? Source Do of variation these variations influence outcome? Clear and defined Unequivocal Key individuals met and agreed on basic standards. All 4 hospitals represented Proforma and Database created If a patient meets the criteria for cooling following cardiac arrest then this should be initiated as soon as possible and definitely within 6 hours of cardiac arrest. Aim for a target core temperature of 32-34˚C Core temperatures should be monitored continuously during cooling and re-warming The duration of cooling should be for 24 hours from commencement of induced hypothermia and not when target temperature is reached. Re-warming should be at a rate of 0.3-0.5 ˚C per-hour to 36.5˚C. Central database Hopefully Data move to a Web based system anonymised prior to submission , processed and fed back Time to initiation of cooling 10 9 8 7 6 5 4 3 2 1 0 hours hospital Hospital Hospital Hospital A B C D Target temp reached 8 7 6 5 YES NO 4 3 2 1 0 hosp A hosp B hosp C hosp D 8 7 6 5 4 hours 3 2 1 0 hospital Hospital Hospital Hospital A B C D Feedback to hospital D 10 9 8 7 6 5 4 3 2 1 0 all hosptals hospital D JANMARCH APRJUN JULSEPT OCTDEC Clinically relevant Collaborative numbers Trainee Audit – Larger patient involvement Potential to spread to other regions Generating a large valuable local database of patients. Tremendous source of useful data on regional practices, patient outcome – Inform decision making. Are we cooling non VF arrests / in hospital arrests What is the outcome in a wider spectrum of post VF/VT patients? Benefits vs Costs Incentive for units to drive up their performance. Funding Links of resources with other networks - The European Resuscitation Council Hypothermia After Cardiac Arrest Registry Study Group Dr Tom Owen Dr Rachel Markham Dr Dominic Sebastian Dr Alison Quinn Dr Tina Duff Dr Neil Moreland Dr Richard Morgan Dr Tom Hurst Dr Brendan McGrath