Digestive
advertisement
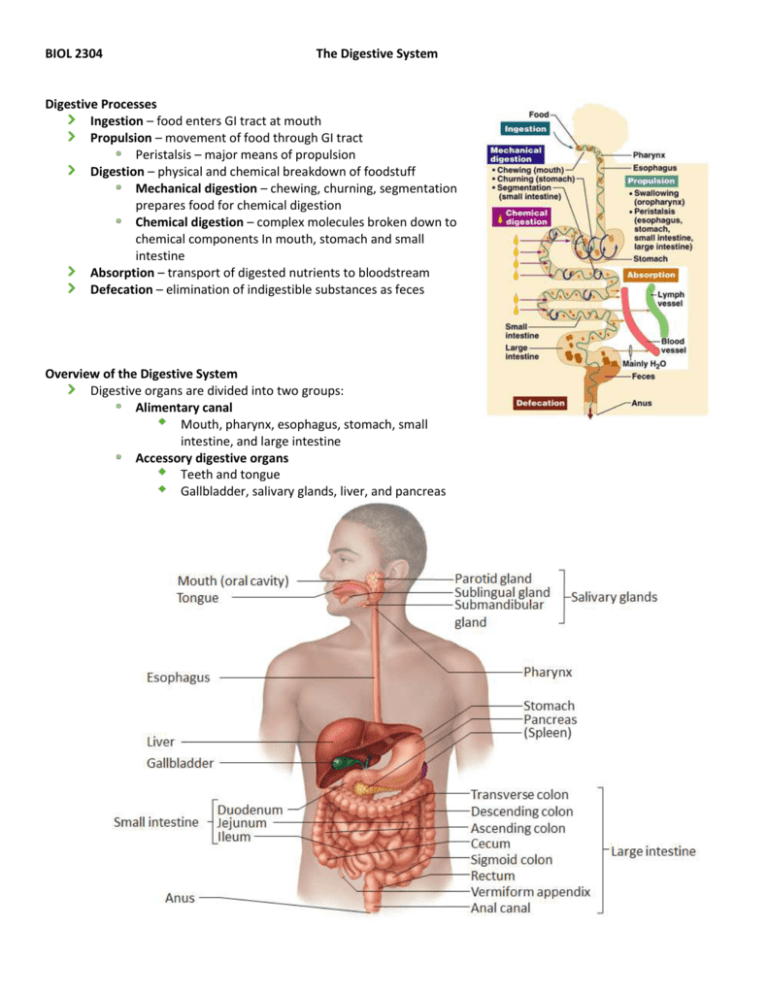
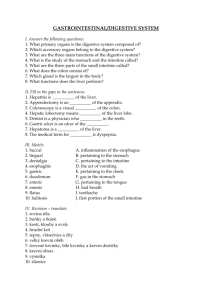
BIOL 2304 The Digestive System Digestive Processes Ingestion – food enters GI tract at mouth Propulsion – movement of food through GI tract Peristalsis – major means of propulsion Digestion – physical and chemical breakdown of foodstuff Mechanical digestion – chewing, churning, segmentation prepares food for chemical digestion Chemical digestion – complex molecules broken down to chemical components In mouth, stomach and small intestine Absorption – transport of digested nutrients to bloodstream Defecation – elimination of indigestible substances as feces Overview of the Digestive System Digestive organs are divided into two groups: Alimentary canal Mouth, pharynx, esophagus, stomach, small intestine, and large intestine Accessory digestive organs Teeth and tongue Gallbladder, salivary glands, liver, and pancreas Digestive Tract Smooth Muscle Movement Peristalsis Major means of propulsion Adjacent segments of the alimentary canal relax and contract Segmentation Rhythmic local contractions of the intestine Mixes food with digestive juices Peristalsis Segmentation Histological Organization of Digestive Tract Mucosa - lines digestive tract (mucous epithelium) Epithelium – lines the lumen, moistened by secretions of mucosal glands Lamina propria – loose areolar tissue Muscularis mucosa – layer of smooth that creates folds called rugae Submucosa - layer of dense irregular connective tissue, vascularized (blood and lymphatic), innervated – nerve plexus, submucosal glands Muscularis externa –smooth muscle arranged in circular and longitudinal layers Adventitia or Serosa – outer membranes made of connective tissue, collagen, and elastin Digestive Tract Membranes Peritoneum – the serous membrane within the abdominal cavity Parietal peritoneum – lines the body wall Visceral peritoneum – covers digestive organs Peritoneal cavity – the fluid filled space between the parietal and visceral peritonea Digestive Tract Membranes Mesentery – a double layer of peritoneum Holds organs in place Sites of fat storage Provides a route for circulatory vessels and nerves Mesenteries Greater omentum – a fatty “apron” of peritoneum Attaches the greater curvature of the stomach to the dorsal body wall Covers the transverse colon and a large part of the small intestine Lesser omentum attaches to lesser curvature of stomach Oral cavity Lined by oral mucosa – stratified squamous, not serosa Hard and soft palates form roof of oral cavity Uvula – guards opening to pharynx; assists in some voice production The Oral Cavity Floor of cavity – tongue Mechanical processing Assistance in chewing and swallowing Sensory analysis by touch, temperature, and taste receptors Functions include: Analysis of material before swallowing Mechanical processing by the teeth, tongue, and palatal surfaces Lubrication Limited digestion Salivary glands (three pairs) Parotid, sublingual, and submandibular Produce saliva – watery solution includes electrolytes, buffers, glycoproteins, antibodies, enzymes Functions include: lubrication, moistening, and dissolving; initiation of digestion of complex carbohydrates (salivary amylase) Teeth Function in mastication of bolus Contain three layers Enamel covering crown Dentin forms basic structure Root - periodontal ligaments hold teeth in alveoli 20 primary teeth AKA deciduous teeth 32 teeth of secondary dentition The Pharynx Oropharynx and laryngopharynx Common passageway for food, liquids, and air Lined with stratified squamous epithelium, no serosa External muscle layer Consists of superior, middle, and inferior pharyngeal constrictors Pharyngeal constrictor muscles assist in swallowing The Pharynx Glottis – the space in between the vocal folds Epiglottis – a flap of cartilage at the root of the tongue that is used to cover the opening of the windpipe during swallowing The Esophagus Muscular tube – begins as a continuation of the pharynx Carries solids and liquids from the pharynx to the stomach Passes through esophageal hiatus in diaphragm Joins the stomach inferior to the diaphragm Cardiac sphincter – closes lumen to prevent stomach acid from entering esophagus The wall of the esophagus contains mucosal (stratified squamous), submucosal, and muscularis layers The Esophagus Epithelium is stratified squamous epithelium When empty, mucosa and submucosa form longitudinal folds Mucous glands – primarily compound tubuloalveolar glands Muscularis externa Skeletal muscle first third of length Adventitia – most external layer The Stomach Site where food is churned into chyme – mechanical breakdown of food Breaking of chemical bonds via acids and enzymes, secretion of pepsin and HCl begins protein digestion Bulk storage of undigested food, food remains in stomach approximately 4 hours Anatomy Of The Stomach Cardia – superior, medial portion Fundus – portion superior to stomach-esophageal junction Body – area between the fundus and the curve of the J Pylorus – antrum and pyloric canal adjacent to the duodenum Rugae - ridges and folds in relaxed stomach Microscopic Anatomy of the Stomach Muscularis has three layers Circular and longitudinal layers and oblique layer Epithelium is simple columnar epithelium Mucosa dotted with gastric pits holds gastric glands Microscopic Anatomy of the Stomach Gastric glands of fundus and body Mucous neck cells - secrete a special mucus Parietal (oxyntic) cells - secrete hydrochloric acid and gastric intrinsic factor Chief (zymogenic) cells - secrete pepsinogen Glands produce 1500ml juice per day Small Intestine Longest portion of the alimentary canal Site of most enzymatic digestion and absorption Secretions and buffers provided by pancreas, liver, gall bladder Three subdivisions: Duodenum Jejunum Ileum Ileocecal sphincter - transition between small and large intestine The Duodenum Receives digestive enzymes and bile Main pancreatic duct and common bile duct enter duodenum Sphincters control entry of bile and pancreatic juices The Small Intestine – Microscopic Anatomy Modifications for absorption Circular folds (plicae circulares) - transverse ridges of mucosa and submucosa Villi - finger-like projections of the mucosa, covered with simple columnar epithelium Microvilli - further increase surface area for absorption Lacteals - terminal lymphatic in villus Histology of the Intestinal Wall Absorptive cells - uptake digested nutrients Goblet cells - secrete mucus that lubricates chyme Enteroendocrine cells - secrete hormones Intestinal crypts - epithelial cells secrete intestinal juice Large Intestine Digested residue contains few nutrients Small amount of digestion by bacteria Main functions absorb water and electrolytes compact material into feces Absorb vitamins produced by bacteria Store fecal matter prior to defecation Large Intestine Gross Anatomy of Large Intestine Four areas of the colon Ascending colon Transverse colon Descending colon Sigmoid colon Special features of large intestine Teniae coli – thickening of longitudinal muscularis Haustra – puckering created by teniae coli Cecum – blind pouch, beginning of large intestine Vermiform appendix – Contains lymphoid tissue The Rectum Rectum – descends along the inferior half of the sacrum Anal Canal – the last subdivision of the large intestine Lined with stratified squamous epithelium Last portion of the digestive tract Terminates at the anal canal Internal and external anal sphincters Defecation reflex triggered by distention of rectal walls Microscopic Anatomy of Large Intestine Villi are absent Contains numerous mucus-secreting goblet cells Intestinal crypts – simple tubular glands Lined with simple columnar epithelial tissue Epithelium changes at anal canal, becomes stratified squamous epithelium The Pancreas Pancreatic duct penetrates duodenal wall Endocrine functions - insulin and glucagons Exocrine functions - majority of pancreatic secretions, pancreatic juice secreted into small intestine Carbohydrases Lipases Nucleases Proteolytic enzymes The Pancreas Exocrine function Acinar cells make, store, and secrete pancreatic enzymes Enzymes are activated in the duodenum Endocrine function Produces insulin and glucagon Regulates blood sugar The Liver Performs metabolic and hematological regulation and produces bile Four Lobes: Left, Right, Caudate, Quadrate Histological organization Lobules containing single-cell thick plates of hepatocytes Lobules empty into bile ducts, bile ducts merge to left/right hepatic ducts Left and right hepatic ducts merge to form common hepatic duct Common hepatic meets cystic duct to form common bile duct The Liver The Liver Liver Lobule - basic functional unit Lobule – hepatocytes arranged in hexagonal plates with vessels permeating in spoke-like fashion Bile canaliculi carry bile to bile ductules Bile ductules lead to bile ducts in portal areas The Gallbladder Hollow, pear-shaped organ Stores, modifies and concentrates bile Bile – bile salts help buffer acids and acts as emulsifier for lipid digestion