occupational diseases
advertisement
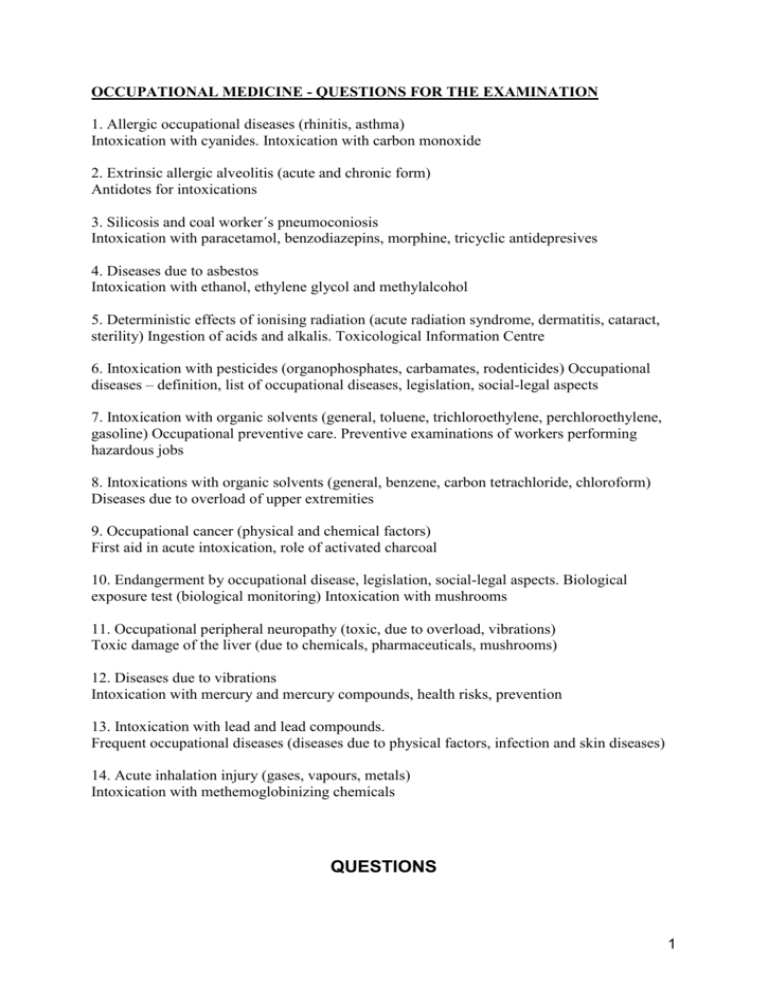
OCCUPATIONAL MEDICINE - QUESTIONS FOR THE EXAMINATION 1. Allergic occupational diseases (rhinitis, asthma) Intoxication with cyanides. Intoxication with carbon monoxide 2. Extrinsic allergic alveolitis (acute and chronic form) Antidotes for intoxications 3. Silicosis and coal worker´s pneumoconiosis Intoxication with paracetamol, benzodiazepins, morphine, tricyclic antidepresives 4. Diseases due to asbestos Intoxication with ethanol, ethylene glycol and methylalcohol 5. Deterministic effects of ionising radiation (acute radiation syndrome, dermatitis, cataract, sterility) Ingestion of acids and alkalis. Toxicological Information Centre 6. Intoxication with pesticides (organophosphates, carbamates, rodenticides) Occupational diseases – definition, list of occupational diseases, legislation, social-legal aspects 7. Intoxication with organic solvents (general, toluene, trichloroethylene, perchloroethylene, gasoline) Occupational preventive care. Preventive examinations of workers performing hazardous jobs 8. Intoxications with organic solvents (general, benzene, carbon tetrachloride, chloroform) Diseases due to overload of upper extremities 9. Occupational cancer (physical and chemical factors) First aid in acute intoxication, role of activated charcoal 10. Endangerment by occupational disease, legislation, social-legal aspects. Biological exposure test (biological monitoring) Intoxication with mushrooms 11. Occupational peripheral neuropathy (toxic, due to overload, vibrations) Toxic damage of the liver (due to chemicals, pharmaceuticals, mushrooms) 12. Diseases due to vibrations Intoxication with mercury and mercury compounds, health risks, prevention 13. Intoxication with lead and lead compounds. Frequent occupational diseases (diseases due to physical factors, infection and skin diseases) 14. Acute inhalation injury (gases, vapours, metals) Intoxication with methemoglobinizing chemicals QUESTIONS 1 OCCUPATIONAL DISEASES 1. Which occupational diseases are the most common ? 2. Which have the worst prognosis ? 3. Which may occur in miner ? in nurses ? in bakers ? 4. What is “biological monitoring” ?, 5. What questions are important for work history ? LEAD 1. 2. 3. 4. 5. Is lead present in glazes for ceramics? What is the target of inorganic lead toxicity? What is the target of organic lead toxicity? What laboratory tests from blood and urine prove lead intoxication? What chelates are used for treatment? MERCURY 1. Does ingestion of mercury from a thermometer represents a danger for humans? 2. What is the trias for chronic toxicity of mercury? 3. What chelate is used for treatment? CYANIDE 1. 2. 3. 4. What is the lethal dose of cyanide salts? What is the smell of hydrogen cyanide ? Why a “therapeutic methemoglobinemia” is done ? Is there a “no risk” therapy of intoxication ? METHEMOGLOBINAEMIA 1. What is metHb ? 2. What symptoms are typical for 40 – 50 % metHb ? 3. What pharmaceuticals are used to treat the “blue patient “ ? CARBON MONOXIDE 2 1. When does the production of COHb occur ? 2. How many times is the affinity of hemoglobin for CO higher than for O2 ? 3. What is the lethal concentration of COHb ? 4. What is the half-life of COHb after the patient is placed in the normal room air ? 5. And with normobaric oxygen? PESTICIDES 1. What are the muscarinic symptoms, for which exposures are they typical ? 2. Can atropin reverse all symptoms of organophosphates poisoning? 3. What are the “acetylcholine esterase reactivators “ ? 4. How can you prove superwarfarin rodenticide granules ingestion ? 5. What is the antidote for this intoxication ? SILICA 1. At which worksites silica exposure represents a real risk ? 2. What structure has the silicotic nodule ? 3. What size of nodules is the borderline between simple and complicated silicosis ? 4. What means “egg shell” in silicosis ? 5. What is the treatment of silicosis ? ASBESTOS 1. Which asbestos induced disease develops only after high asbestos exposure ? 2. What is “asbestos body” and where can it be found? 3. What sounds can be heard by auscultation in asbestosis? 4. What ventilatory impairment is typical for asbestosis? 5. Is incidence of mesothelioma influenced by smoking? 6. What are the “geographic-like” opacities in the radiograph of the chest? ASTHMA 1. What is the target lung structure affected in asthma? 3 2. 3. 4. 5. What sounds can be heard during asthma dyspnoea? What is the mechanic explanation for the sounds? What ventilatory disturbance is typical? Can dyspnoea due to asthma develop at the workplace? SOLVENTS 1. 2. 3. 4. What is the common toxicity of all organic solvents? What solvent is the most abused? Is milk appropriate for first aid? What is the most important danger in case of small ingestion of petroleum distillates? 5. What are the metabolites of toluene, benzene, trichloroethylene? HEPATOTOXICITY 1. What is typical for chemicals causing obligatory hepatic toxic injury? 2. Which mechanisms play role in facultative hepatotoxic chemicals? 3. Is prognosis of centrizonal hepatic injury better than for periportal damage? 4. With which hepatic cells damage is usually related liver cirrhosis? CANCER 1. What is the percentage of cancer due to occupational exposure? 2. What laboratory method is useful for biological monitoring of exposure to carcinogens? 3. Can wood dust be carcinogenic? 4. What malignancy causes benzene? 5. What malignancy is typical for vinyl chloride? 6. What malignancy is typical for dyes production (aromatic amines)? 7. What is the most frequent cancer due to ionizing radiation? ACUTE INHALATION INJURY 1. 2. 3. 4. Which chemicals have more pronounced warning properties? What is the latency period before ARDS (lung oedema) develops? Is high concentration of gasoline vapours dangerous ? What metals cause the metal fume fever? 4 5. Can metal vapours cause lung edema and pneumonitis? EXTRINSIC ALLERGIC ALVEOLITIS 1. What vegetal products can represent a risk of EAA ? 2. What animal products can represent a risk of EAA ? 3. What is the target lung structure affected in extrinsic allergic alveolitis? 4. What imitates the acute form? 5. What are the symptoms of the chronic form? 6. What sounds are typical in auscultation? 7. What inorganic chemicals cause EAA? 8. Where are there used? TREATMENT OF INTOXICATIONS WITH PHARMACEUTICALS 1. What means “primary elimination “? 2. When induction of vomiting and gastric lavage are contraindicated? 3. What non-specific complications are common in severe intoxications? 4. If there is an antidote – is it preferred to extracorporal elimination ? 5. What is called “universal antidote “ ? 6. At what dose is it given? 7. For which kind of drug intoxication is indicated a forced diuresis ? 8. From what compartment is a drug or chemical removed by hemodialysis or hemoperfusion ? 9. Which extracorporal method is used for severe salicylates intoxication? 10. Which is used for theophylline? 1. 2. 3. 4. 5. 6. 7. Are benzodiazepins toxic for liver and kidneys? What antidote is used for treatment of this intoxication? What is the hepatotoxic dose for paracetamol? What is the treatment of severe paracetamol overdose? What treatment is indicated for severe digoxin intoxication? What is the main risk of morphine derivates intoxication? What is the appropriate treatment of this symptom? 5 ALCOHOLS 1. What are the metabolites of ethanol? 2. Can the elimination rate be accelerated by forced diuresis? 3. What is the mean lethal dose of an alcohol distillate? 4. What is the lethal level of ethanol? 5. What are the main risks in a severe intoxication? 6. What treatment is appropriate? 7. What are the sources or ethylene glycol? 8. What is used for first aid? 9. What organ damage causes the final metabolite? Which metabolite is it? 10.What level of ethanol in blood is recommended for treatment ? 11.What metabolic disturbance causes the final metabolite of methanol? 12.What extracorporal method is indicated in case of intoxication with methanol ? MUSHROOMS 1. Which are the amatoxin-type mushrooms and how they look like ? 2. When is typically the inset of symptoms? 3. How many caps of a. phalloides represent the lethal dose ? 4. What antidote is used ? 5. What colour has a. muscaria and what a. pantherina ? 6. What are the typical symptoms and when they begin ? 7. Is there an antidote for treatment of this intoxication ? 8. What are the symptoms of psilocybe intoxication ? 9. What is the hallucinogenic dose ? 6 7