Cardiac Consultation for Infants of Diabetic Mothers
advertisement

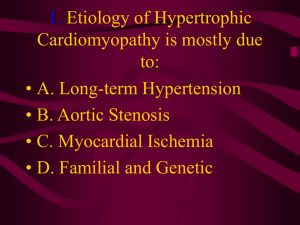
Cardiac Consultation for Infants of Diabetic Mothers Division of Pediatric Cardiology MUSC September 27, 2006 Background Infants of diabetic mothers have an increased risk of cardiac malformations. The magnitude of the risk is similar to that of parents with prior offspring affected by cardiac malformations – somewhere between 2 and 5 times the background rate of cardiac malformations. The risk for malformation is linked most significantly to glycemic control in the first 6 weeks of pregnancy. These data are well known to the high risk obstetrical community, who generally follow these patients very closely and typically thoroughly and accurately evaluate for fetal malformations, including cardiac malformations, by fetal ultrasonography. Hypertrophic cardiomyopathy (HCM) is an additional concern in the IDM. Many studies document differences in the hearts of the IDM in mass and function, in some examples as early as 12 weeks gestation. These changes are believed to be the result of the hyperinsulinemic-hyperglycemic environment of the heart that is accompanied by increased IGF-1 signaling and increased cardiac output demands. HCM in IDMs can therefore be regarded as the end of a spectrum of cardiac responses to the physiologic environment of a diabetic pregnancy. The generally observed outcome of HCM in IDM is complete resolution by 6 months of age, and medical intervention is only infrequently needed. HCM in the IDM does not have an association with arrhythmias, and sudden arrhythmic death in IDMs with HCM and no other signs or symptoms of HCM has not been described. The prevalence of symptomatically affected IDMs with HCM is not well known but does not appear to be high. The incidence of echocardiographicallyidentified asymptomatic and self-limited abnormalities in the IDM population is also not well defined, but in anecdotal experience as well as literature reports, subclinical ‘abnormalities’ are commonly identified that do not usually change the management or outcome of the infant. Suggested Guidelines On the basis of these findings, we suggest the following guidelines for cardiac evaluation in an infant of a diabetic mother. 1. All infants born to mothers with diabetes should undergo a thorough clinical cardiac evaluation after birth by the pediatric or neonatal healthcare provider, with special attention paid to the four-limb blood pressures and the second heart sound. 2. The mother’s chart should be reviewed and the results of any fetal ultrasonography and fetal echocardiography should be noted. 3. A cardiology consultation should be requested if there is a symptom or sign referable to the heart – tachypnea, a loud (3/6) systolic murmur, a diastolic 4. 5. 6. 7. murmur, central cyanosis, low oxygen saturation on pulse oximetry, or a low PaO2 on an arterial blood gas. An infant with a cardiac murmur who is hemodynamically stable and has no respiratory problems should be followed with periodic clinical examination during the hospital stay. If a cardiology evaluation is thought necessary in such infants, it is best performed closer to the time of hospital discharge, to allow for the disappearance of transient clinical findings from transitional circulation. An urgent or ‘stat’ evaluation should not be requested in such patients. If there are clinical findings that raise the possibility of a cardiac disease but the infant is hemodynamically normal, and the findings of fetal ultrasonography or fetal echocardiography rule out a serious cardiac malformation, it is often appropriate to send the patient home and refer to the cardiology clinic on an elective basis. If a higher than normal level of vigilance is desired for infants of diabetic mothers, routine pulse oximetry prior to discharge should be considered as a possible back-up screen to physical examination for the question of cardiovascular malformation. Mandated early (1 week) follow-up can serve to increase surveillance for evolution of murmurs or tachypnea indicating a symptomatic degree of HCM.