Recommendation to Scottish Clinical Virologists Consultant Group

Antenatal rubella susceptibility screening in Scotland:
A Scottish Clinical Virologists Consultant Group Report
Introduction
Rubella virus usually causes a mild illness, but if acquired by women in early pregnancy can lead to congenital rubella syndrome, leading to serious birth defects. A single dose of the measles, mumps, rubella (MMR) vaccine which contains the live attenuated rubella strain RA 27/3, induces long-lasting immunity in more than 95% of recipients. Rubella has a basic reproduction number (R
0
) of 7-8 (the average number of secondary infectious cases that are produced by a single index case in completely susceptible population).
The critical vaccination coverage required to block transmission is therefore
85-87%.
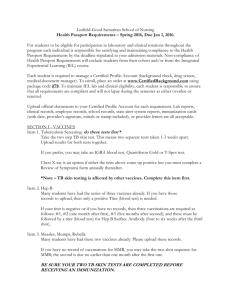
MMR uptake rates in Scotland, are currently 97.1 per cent in children reaching the age of five and has been equal or greater than 87% between
1995 and 2011. MMR is an excellent public health intervention which offers protection from measles, mumps and rubella.
96.0
94.0
92.0
90.0
88.0
86.0
84.0
82.0
80.0
MMR1 uptake at 2 years
MMR2 uptake at 5 years
MMR2 uptake reported at 5 years from 2006 only
78.0
76.0
1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012
Year
Both the UK National Screening Committee and the Joint Committee on
Vaccination and Immunisation have advised that antenatal rubella screening should be replaced with an assessment of vaccination history. A working group has been set up to arrange implementation of transition to assessment of vaccination history.
UK National Screening Committee
The policy position of the UK National Screening Committee’s (UK NSC) on rubella susceptibility screening in pregnancy states:
12
10
8
6
4
2
0
‘Screening for rubella susceptibility does not meet the UK NSC criteria for a screening programme. The UK has a very low incidence of congenital rubella syndrome but increasing reports of susceptibility in pregnant women. In this context there is concern that the current approach based on screening all pregnant women and vaccinating those found to be susceptible is not the optimum approach to preventing outbreaks of rubella infection.
MMR is an excellent public health intervention and an alternative strategy, which may be better placed to protect the population, is being considered by the UK NSC and JCVI.
The present arrangements for antenatal screening and post partem immunisation should continue until other arrangements ar e in place.’
Joint Committee on Vaccination and Immunisation
The Joint Committee on Vaccination and Immunisation (JCVI) on Wednesday the of 6th February 2013 minutes regarding antenatal rubella screening (3):
‘The committee was informed that there have been initial discussions about the implementation of JCVI/NSC advice to replace antenatal screening for rubella via susceptibility testing with an assessment of vaccination history. A working group would be convened by PHE Immunisation and Screening with i mplementation by the NHSCB.’
The last case of congenital rubella syndrome was diagnosed in 1999 in
Scotland. All diagnoses of rubella are now imported cases, of which there have been 30 in total between 2000-2012 inclusive.
Rubella vaccine for school girls introduced, 1970
MMR vaccine introduced, Oct 1988
MR schools camapign, 1994
MMR 2nd dose introduced, Oct 1996 year
Figure 3: Rubella notifications and laboratory reports, Scotland, 1988-
7000
MMR vaccine introduced, Oct 1988
6000
MR Campaign, 1994
5000
4000
3000
2000
2nd dose MMR introduced, 1996
Lab reports
Notifications
1000
0
Year
Despite on going clinical notifications of rubella, there have been small numbers of laboratory confirmed cases (see Table 1). This is likely to be due to significant numbers of misdiagnoses of other rash causing illnesses. These include those possibly due to parvovirus B19, enterovirus, human herpesvirus-6 and -7, measles, cytomegalovirus, Epstein-Barr virus, streptococcal, meningococcal and syphilis rashes.
Table 1: Laboratory Confirmed Cases Scotland 2000-2012
Year Vaccine Uptake* (%) Notifications
Laboratory
Confirmed
2000 93.2 349 5
2001
2002
88.5
87.8
234
292
2
7
2003
2004
2005
2006
2007
86.8
88.3
89.9
92.1
92.1
130
222
141
153
146
1
1
4
0
0
2008
2009
2010
2011
2012
92.6
93.6
93.2
106
93
39
4
0
1
94.0 21 0
95.0 44
* Uptake of one dose of MMR by age 24 months
5
900
800
700
600
500
400
300
200
100
0
Current antenatal rubella susceptibility screening in Scotland
Rubella IgG
<10 IU/ml >/=10 IU/ml
<10IU/ml
2
nd
Rubella IgG test
(on an alternative platform)
Reported:
Rubella antibody detected
>/=10 IU/ml
Rubella antibody NOT
DETECTED
– MMR vaccination recommended post delivery, up to a lifetime maximum of two documented doses
Reported:
Rubella antibody detected
Infectious Diseases in Pregnancy Screening Programme Handbook for
Laboratories - Second Edition, October 2012
The Infectious Diseases in Pregnancy Screening Programme Handbook for
Laboratories - Second Edition, October 2012 from the UK National Screening
Committee and NHS Screening Programmes recommended changes to the laboratory testing of rubella susceptibility (2).
The key changes and revisions include:
removal of the need to confirm the absence of rubella-specific antibodies by repeating the test using a different analytical method.
The IDPS programme has concluded that current assays that test for rubella susceptibility provided by different manufacturers show a wide variation in results when analysing the same specimens, even though results are reported in IU/ml. Some assays have also been reported to lack precision. For these reasons, repeat and confirmatory testing is not considered helpful. (Page 5)
Current practice of rubella susceptibility testing compared to a the recommended change
As an example of the current practice in Scotland an assessment was made of the West of Scotland Specialist Virology Centre (WoSSVC) rubella testing.
They offer rubella susceptibility testing on the ARCHITECT i2000SR (Abbott
Laboratories, USA). For those with <10/IU/ml a second test is offered in the form of rubella IgG Vidas testing ( bioMérieux, Marcy l'Etoile, France). In 2012 the WoSSVC tested 14,138 patients for rubella IgG. 87.1% (12,312) were determined to have detectable rubella antibody on initial testing (>/= 10
IU/ml). 1,826 samples were then tested for rubella IgG by Vidas. 1039 (57%) were immune on the second test. In total, 13,351 (94.4%) were found to be rubella immune after a second test in those who were non-immune ( <10IU/ml rubella IgG) by Abbott Architect.
Current and proposed future protocol (based upon the cost of provision of one MMR dose to all patients with an undetectable rubella IgG, which would induce long-lasting immunity against rubella in more than 95% of recipients)
Architect Rubella
IgG
(14,138)
<10IU/ml
1,826 (12.9
% )
>/=10 IU/ml
12,312 (87.1%)
Current : Vidas
Rubella IgG
1,826 x £4.78 =
£8728.28
Vidas <10 IU/ml =
Rubella antibody NOT
DETECTED
(750, 5.3% of total)
1 dose MMR =
750 x £5.52= £4140
Final cost:
£12,868.28
Proposed : Rubella antibody NOT DETECTED
1 dose MMR =
1826 x £5.52 = £10,079.52
Rubella antibody detected
Vidas >10 IU/ml
= Rubella antibody
DETECTED
(1076, 7.6% of total)
Final Cost:
£10,079.52
The second rubella IgG VIDAS test with the additional cost of vaccinating the
5.3% who remain rubella IgG undetectable costs £2,788.76 more than the proposed algorithm.
Laboratories no longer offering a second rubella IgG test
West Midlands Public Health Laboratory, Birmingham
Sheffield Virology Services
Public Health Laboratory, Cambridge
Regional Virus Laboratory, Belfast
Evidence on the provision of MMR vaccination on a postnatal ward
The Southern General Hospital had 253 patients who had an undetectable rubella antibody in 2012. In the same year 151 doses of MMR were administered on their postnatal wards. The equivalent of 59.7% (151/253) of postnatal women received 1 dose of MMR in 2012. Many women would have
2 past documented doses of MMR and some individuals would be expected to have declined the offered vaccine. This provides evidence that MMR can be provided successfully postnatally and evidence can be collected to provide auditable data on it’s provision.
The screening of postnatal women is not the optimal use of resources due to:
1. The low incidence of congenital rubella syndrome (the last case in
Scotland was diagnosed in 1999).
2. Screening in pregnancy does not contribute to the reduction of risk in the current pregnancy.
3. Testing may falsely reassure some women that they are not susceptible to rubella infection.
4. The lack of impact of screening on the immunity of the whole adult population.
Table 2: The advantages and disadvantages of the current and proposed antenatal screening protocols
Current 1 st and 2 nd line rubella IgG testing
Less MMR administration on
Proposed single rubella IgG test
More individuals vaccinated postnatal ward
Less MMR side effects inc: o mild form of measles lasts 2-3 days o mild form of mumps o that lasts for 1-2 days
idiopathic thrombocytopenic purpura (1 in 40,000 vaccinations) o Anaphylaxis
(long term immunity in >95% of recipients), reduced risk of congenital rubella syndrome
Improved herd immunity to rubella in Scotland
Less financial cost to NHS
Faster turnaround time for antenatal results
Reduced laboratory staff time
Potential for standardised testing across Scotland
No requirement for microbiology laboratories to send samples away for a second line test
Preparation for replaced of rubella screening with an assessment of vaccination history
More vaccinations to be performed on postnatal ward
Higher cost to NHS
Testing does not improve population immunity
No evidence that any assay is more accurate
Greater risk of falsely reassure some women that they are not susceptible to rubella infection
Conclusion
The benefits of the current recommendation from the UK National Screening
Committee and NHS Screening Programmes - Infectious Diseases in
Pregnancy) outweigh the risks.
Scottish Clinical Virologists Consultant Group Recommends that:
1. A single test for rubella IgG should be offered as part of antenatal screening in Scotland.
2. MMR should be offered to all patients with rubella IgG <10 IU/mL, who do not have two previous documented doses of the vaccine.
3. The first dose of MMR should be administered on the post natal ward prior to discharge.
4. If no previous documented history of MMR a second dose should be administered by the patients General Practice one month later.
Implementation of these recommendations will provide a more cost effective protocol for the NHS in Scotland and will increase MMR vaccine provision.
Produced on behalf of the Scottish Clinical Virologists Consultant Group by:
Dr Eleri Wilson-Davies
Consultant Medical Virologist
West of Scotland Specialist Virology Centre,
Level 5, New Lister Building,
Glasgow Royal Infirmary,
10-16 Alexandra Parade,
Glasgow, G31 2ER.
Tel: 0141 201 8736
Main laboratory Tel: 0141 201 8722
References
1. Health Protection Scotland: Immunisation & Vaccines; rubella http://www.hps.scot.nhs.uk/immvax/rubella.aspx
2. Infectious Diseases in Pregnancy Screening Programme Handbook for
Laboratories - Second Edition, October 2012. UK National Screening
Committee and NHS Screening Programmes - Infectious Diseases in
Pregnancy http://infectiousdiseases.screening.nhs.uk/standards