selection criteria - Hurley Medical Center
advertisement

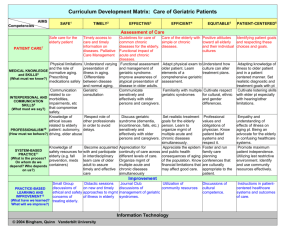
HURLEY MEDICAL CENTER GERIATRIC FELLOWSHIP PROGRAM GERIATRIC RESIDENCY SELECTION CRITERIA POLICY: Medical graduates appointed to the Geriatric Fellowship Program at Hurley Medical Center must meet the following criteria. 1. Candidates must submit a medical degree prior to the start of the residency program. 2. Candidates must present documentation of graduation from an ACGME accredited Internal Medicine residency program in good standing. 3. Candidates must submit three letters of recommendation. 4. Candidates must submit official medical school transcripts. 5. Candidates must submit a personal statement and curriculum vitae. 6. Where applicable, candidates must submit proof of a valid ECFMG certificate and a valid TOEFL certificate. 7. Where applicable, candidates must submit one of the following visas: J-1, Immigrant, or any other visa deemed acceptable for residency training at Hurley Medical Center. 8. Candidates must submit proof they have passed the USMLE examination parts 1, 2 and 3 with a score of at least 78. Exceptions can be made for candidates whose school does not require passing USLME. 9. Candidates must participate in interviews with appropriate residency training program faculty who will assess professionalism, teamwork, clinical abilities, interpersonal skills, humanistic quality, academic performance and communication skills. 10. Candidates must meet all eligibility and selection criteria of resident’s guidelines established by the Accreditation Council for Graduate Medical Education. 11. Candidates must apply through ERAS. I:IntMed\Geriatric Program\Resident Candidate Criteria HURLEY MEDICAL CENTER GERIATRIC FELLOWSHIP PROGRAM ACUTE GERIATRICS TEACHING PROGRAM A: ACUTE GERIATRICS CURRICULUM An acute geriatrics curriculum requires a different paradigm from the traditional teaching of ward medicine. This paradigm recognizes that hospitalized elderly patients often present with unusual symptoms that challenge normal diagnostic methods, experience a high rate of iatrogenic illness, and face serious risk of functional decline and personal indignity while in the hospital. Primary teaching goals therefore, are to understand the interaction of acute hospitalization with the physiologic changes of aging, to make accurate diagnosis of atypical symptoms, and to implement care that prevents primary topics in an acute geriatrics curriculum that are used to generate bedside and didactic teaching sessions. Understand common physiologic changes of aging ● ● ● ● ● ● ● ● ● Diminished cognitive reserve Immune system senescence Decline in musculoskeletal and autonomic function Reduction in pulmonary compliance and reserve Diminished GI motility Reduction in renal and hepatic pharmacodynamics capacity Loss of skin function and integrity Common sensory deficits (e.g. diminished hearing and vision) Risks of bladder incontinence due to changes in prostate, pelvic muscle, and neurologic function Understand the interaction of hospitalization with elderly persons ● ● ● ● ● ● ● Detrimental effects of immobilization on continence, skin integrity, and musculoskeletal functions Understand the high risk for functional decline and institutionalization Know the common causes of delirium, falls, and procedure complications Risk assessment and prevention of polypharmacy and nosocomial infections Recognize loss of personal dignity caused by hospital environment Recognize indications for selection of nasogastric, gastroostomy, or jejunostomy tube feeding Understand the risks and benefits of enteral feeding, including positive and negative effects on aspiration risk and quality of life Accurate diagnosis of atypical symptoms ● ● ● ● ● Raise awareness of subtle presentation of serious illness in the elderly (e.g., lower incidence of chest pain in acute myocardial infarction, high prevalence and atypical symptoms of depression) Know the common manifestations of drug toxicity in elderly patients (e.g., weakness, delirium, falls, incontinence) Maintain high suspicion for skin and soft tissue infections in bed-bound population Recognize delirium as a presentation of systemic infection or hemodynamic compromise Detect the functional decline caused by dehydration, malnutrition, and bed rest Implementation of standards of care ● ● ● ● ● ● ● ● B: Preservation of functional independence with early mobility Methods for risk assessment and treatment of delirium and pressure ulcers Daily medication review for necessity and toxicity Regular use of interdisciplinary team process to address all medical, social and functional issues needed for successful discharge planning Understand the proper use of alternatives to physical restraints Prevention of iatrogenic illness from procedures, catheters, and foreign hospital environment Develop skills at leading family conferences, particular in planning end-of-life care Legal and ethical aspects of end-of-life decision-making, including substituted judgement, power of attorney for health care and use of do-not-resuscitate, do-not-hospitalize, and hospice care orders. KEY ELEMENTS OF AN ACUTE GERIATRICS TEACHING PROGAM This section outlines the personnel and structural components of an acute geriatrics-teaching program. This outline can be adapted to match the needs of the local residency environment. ● Faculty Supervision– The presence of a teaching physician with expertise in geriatrics is an essential element. These supervisory physician acts as role models to underscore the risks of iatrogenic illness, place high priority on patients’ functional status, and provide daily mentorship on managing the care of frail persons with complicated medical and social problems. ● Interdisciplinary Team Experience– The residents should meet regularly (daily if possible) with a team of PT/OT therapists, social worker, home care staff, and nursing staff to discuss the acute and postacute plan of care. Integration of an interdisciplinary approach into daily rounds helps residents gain appreciation for the valuable role of every discipline in the successful care of elderly hospitalized patients. This meeting allows team members to hear regularly about the needs of the elderly patients and provides an invaluable team experience for the interns. ● Case-Based Teaching Rounds– On a daily basis, an attending physician and supervising medical resident alternate in leading a 30-minuet case-based discussion on a topic of acute geriatrics care. This prepared classroom session is held in the early morning before work rounds and is evidence-based whenever possible. Topics for this teaching session are chosen from the curriculum described in section A. ● Bedside Teaching Rounds– The teaching physician performs bedside rounds with housestaff daily. These rounds usually last for two hours and focus on history and physical examination skills and on practical advice for the management of frail elderly persons with acute illness. Bedside teaching remains the cornerstone for the management of acute geriatric problems such as delirium, pressure ulcers, functional decline, and pain management. It is preferable that the teaching physician also be the physician of record, although this is not possible for all patients. ● Didactic Conferences– A weekly schedule of department-wide didactic sessions should include regular leadership by physicians with expertise in geriatrics. Conferences at which geriatricians maintain a strong presence include: 1) 2) 3) Morning report – These weekly one-hour sessions are joined by geriatrics faculty and internal medicine faculty and focus on recent geriatrics literature that pertain to the presented case. Residents’ Noon Lectures – Each year, geriatrics faculty conduct four conferences that are devoted to distinctive syndromes in geriatric medicine. Department of Medicine Grand Rounds- Faculty from the division of geriatric medicine offer an average of two clinical presentations per year. These are devoted to recent progress in the field of geriatric medicine. II A. POST-ACUTE/REHABILITATION TEACHING PROGRAM Post-Acute/Rehabilitation Curriculum A primary goal of a post-acute teaching program is to change residents’ thinking from a traditional diseasebased model of diagnosis and treatment to one that emphasizes functional recovery and the successful transition of patients back into the community. To achieve this goal, curriculum topics for the didactic and bedside teaching sessions are chosen from three categories of functional, social, and medical issues. Functional Issues ● ● ● ● ● Understand common conditions in older people, which benefit from rehabilitation Understand the community discharge options for people with functional impairment Develop history and physical exam skills that focus on functional assessment Understand the role of assistive devices and orthotics for various functional deficits Gain an appreciation of function so that functional improvement becomes a major part of residents’ clinical decision making Social Issues ● ● ● ● Appreciate the importance of patients’ home situation and caregivers in discharge planning Learn to function as a physician leader on an interdisciplinary team and to value the role of all other professional staff Develop interviewing skills that thoroughly assess the social environment and all resources that are available for a patient after discharge Learn to construct social and medical systems that provide adequate safety and follow-up care Medical Issues ● ● ● ● ● ● ● ● ● ● Understand the major categories of hip and knee orthopedic repairs and their implications for issues such as total hip precautions and weight-bearing status Know standard of care for DVT prophylaxis after orthopedic procedures Demonstrate understanding of pharmacology appropriate for the elderly by prescribing simplified medical regimens with minimal polypharmacy and toxicity Recognize the etiology and presentation of major stroke syndromes, their etiology, and optimal treatment Refine residents’ neurologic and musculoskeletal physical diagnosis skills Recognize and treat common post-acute complications such as nosocomial infections and procedural complications Understand the appropriate prevention and treatment of pressure ulcers Learn to manage post-acute care of bladder/bowel dysfunction Recognize multi-factorial causes and atypical nature of depression Understand the strengths and weaknesses of a post-acute/rehabilitation setting in the continuum of care for frail older patients. B. Key Elements of a Post-Acute/Rehabilitation Teaching Program ● Patients- Patients in the inpatient post-acute setting generally belong to three major categories: patients with new neurologic deficits, patients with recent orthopedic procedures, and patients with general deconditioning and loss of function due to a recent hospital admission. In addition to their rehabilitation issues, these patients usually have numerous active medical issues such as bladder dysfunction, deep venous thrombosis (DVT) prophylaxis, nosocomial infections, depression, delirium, and polypharmacy. ● Faculty Supervision- Residents work under the direct daily supervision of a physiatrist physician and with physician with expertise in geriatric medicine that has clinical responsibility for the patients. This allows residents to receive daily instruction on practical geriatric and rehabilitation issues from a physician skilled in these areas. ● Interdisciplinary Team Experience- Residents participates in weekly meetings where they interact with all disciplines of the professional staff involved in patients’ care. Such staff includes social work, PT, OT, speech pathology, physiatry, psychology, nursing, and home care services. This interdisciplinary experience is the central mechanism for learning the methods of functional recovery and comprehensive discharge planning that are essential to successful care in the rehabilitative setting. ● Didactic Teaching Rounds- One-hour weekly sessions are devoted to case-based teaching rounds that focus on post-acute issues. These talks provide residents with exposure to a core base of knowledge in neurologic evaluation, common post-hospital syndromes (e.g. infections and procedure complications), and in rehabilitative medicine. ● Bedside Rounds- The attending physician leads residents on bedside rounds 3-5 times per week. These rounds allow residents to observe patients’ functional progress and to discuss newly admitted patients. This process provides residents with an opportunity to directly implement tools of functional assessment as the patients are undergoing their rehabilitation. ● Family Meetings- Residents participate as the primary physician during family meetings for each patient on the rehabilitation unit. These meetings include the patient, family, and interdisciplinary staff and focus on all issues that affect patients’ recovery and discharge plan. The meetings occur after 7-10 days on the unit, last for 30-45 minutes, and aim to improve communication between team members and patients and their families. ● Didactic Conference- Two weekly seminars are devoted to discussing the clinical and scientific basis of geriatric medicine and serve as an integral part of the post-acute/rehabilitation rotation. These conferences review major topics in geriatric medicine and reinforce learning that occurs on the postacute unit. III “AMBULATORY” GERIATRICS TEACHING PROGRAM A. “Ambulatory Geriatrics Curriculum The curriculum for an outpatient rotation in geriatrics will cover the following: a) Primary and Preventive Health Care ● ● ● ● ● Understand the proper use of immunizations in elderly patients Environmental strategies for fall prevention Risks and benefits of cancer screening in the aging population Methods for prevention of drug toxicity Establish clear advance directives b) Management of Common Outpatient Geriatric Problems ● Urinary incontinence- Understand the physiologic, behavioral, and pharmacologic causes of urinary incontinence. Residents should become familiar with the wide range of treatment options available, including pelvic muscle exercises, biofeedback, behavioral change, as well as drug and surgical therapies. ● Dementia- Residents refine skills in neurologic and mental status evaluation and learn to distinguish clinical features of various dementing diseases. They also learn to work within an interdisciplinary team that provides the medical and social resources needed for the support of demented patients and their families. This includes evaluation of elderly drivers. ● Osteoporosis- Residents learn to understand the risk factors, etiology, evaluation, and treatment options for metabolic bone disease in the elderly. The focus is on methods of preventive care that can reduce the burden of disability from osteoporosis. ● Rheumatologic Disease- Specific teaching goals include the assessment of function in patients with musculoskeletal disorders, diagnosis and management of osteoarthritis, tendonitis, bursitis, crystalinduced joint disease, late-onset connective tissue disease, and the use of local and systemic therapies for these conditions. Residents also gain experience in assessing and managing patients with musculoskeletal pain, falls, and a need for joint replacement. c) Interdisciplinary approach A primary teaching goal is for residents is to understand and appreciate the critical role of all team members in the primary care of elderly patients. Residents learn to respect and work cooperatively with every caregiver. This is accomplished by the following practices. ● ● ● ● ● B. Coordination of home nursing and rehabilitative services with nurses and therapists Establishment of social and personal care support via social work and community resources Developing collegial working relationships with aides or family caregivers who provide the bulk of patients’ personal care needs Learning to involve pastoral care staff in stressful or end-of-life circumstances Learning to manage patients with terminal illness from experience in a home hospice care team that includes family caregivers, nurses, aides, and social work staff Key Elements of an Ambulatory Geriatrics Teaching Program ● Primary Care Geriatrics Practice- The primary focus of this experience is on management of multiple chronic illnesses, reducing polypharmacy, and the maintenance of independence. Residents work in an outpatient clinic under supervision of physicians with expertise in primary care geriatric medicine. ● Urinary Continence Clinic- In this clinic, residents work with a clinical nurse specialist and physician with expertise in bladder dysfunction. They perform new patient evaluations for the comprehensive diagnosis and management of urinary incontinence. Teaching tools include a standard continence interview form, bladder ultrasound testing, and specialized examination techniques to allow pelvic and bladder function assessment. ● Geriatric Rheumatology Practice- In this specialty program, residents focuses on the diagnosis and treatment of musculoskeletal disease with the goal of attaining maximal function with minimal drug toxicity. Residents work directly under the supervision of a physician who has expertise in geriatric medicine and musculoskeletal diseases of elderly patients. ● Physician Supervision- In each setting, residents see patients under the guidance of a physician with expertise in geriatric medicine. This supervision is critical to developing strong role models who can communicate enthusiasm and knowledge about the subject of geriatric medicine. In particular, residents benefit greatly from exposure to physicians with experience in geriatric medicine and additional expertise in Rheumatology, infectious diseases, home care, urinary continence, and osteoporosis. ● Weekly Didactic Sessions- Each week during the rotation, residents participate in a block of three 45minute small group seminars on an array of topics in geriatric medicine. These seminars are case-based and re-emphasize the principles raised in residents’ clinical experiences in various geriatric ambulatory clinics H:geriatric.fellowship.curriculum HURLEY MEDICAL CENTER GERIATRIC FELLOWSHIP PROGRAM CURRICULUM INFORMATION Elective (3 months) Geriatric Outpatient Clinic (1 month) Geriatric Inpatient Service (2 months) Geropsychiatry (1 month) Hospice Care (1 month) PMR Inpatient (1 month) PMR Consultative (1 month) Sleep Disorder/Urology (2 months)