UKGTN_RESPONSE_Commissioning_for_patients_Oct_10
advertisement

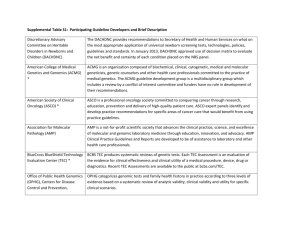
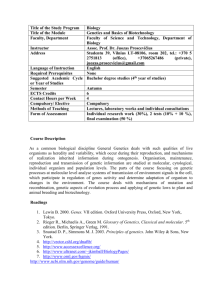
RESPONSE TO THE PUBLIC CONSULTATION: LIBERATING THE NHS: COMMISSIONING FOR PATIENTS Submission by: Project Team: Programme Director Clinical Advisor: Scientific Advisor (molecular): Scientific Advisor (cytogenetic): Public Health Advisor UK Genetic Testing Network (UKGTN) Project Team Jacquie Westwood Dr Shehla Mohammed (Consultant Geneticist and Head of Service, Guys & St Thomas’ Hospital) Su Stenhouse (Head of Laboratory, South West Scotland Regional Genetics Centre, Glasgow) Val Davison (Head of Laboratory, Birmingham Regional Genetics Centre) Dr Mark Kroese (Consultant in Public Health, Peterborough PCT) UKGTN Knowledge & Communications Manager UKGTN Programme Manager UKGTN Business & Corporate Support Officer Contact: Dr Jacqui Hoyle Jane Deller Tarita Turtiainen UKGTN, c/o NHS Specialised Services, NHS London, 2nd Floor Southside, 105 Victoria Street, London, SW1E 6QT Tel: 020 7932 3969, email: UKGTN.Enquiries@london.nhs.uk The United Kingdom Genetic Testing Network: Context The UKGTN Steering Group was established in 2002 and is part of NHS Specialised Services hosted by NHS London. Prior to the publication of the White Paper ‘Our Inheritance – Our Future; Realising the potential of genetics in the NHS’ UKGTN was set up to prepare NHS genetic laboratories for the future. The role was to facilitate co-operation and work sharing between different laboratories in collaboration with the National Genetics Reference Laboratories. Recently the Government response to the House of Lords report on Genomic Medicine has named UKGTN as an organisation that will facilitate change in the NHS in response to genomic advances. UKGTN is also working with member laboratories on related aspects outlined in the Department of Health’s Response to the Report of the Second Phase of Independent Review of NHS Pathology Services in England focusing on quality, innovation, prevention and productivity (QIPP). The UKGTN supports QIPP and will be holding a national conference in November 2010 based around the QIPP agenda. Professor Sir John Burn will Chair the conference and provide a key note address. The conference will cover care pathways, provider efficiency, reducing inefficiencies in diagnostics, organisation of laboratories, system efficiencies and inspiring innovation. UKGTN is a clinical network of NHS laboratory scientists, clinical geneticists that collaborate with genetics commissioners and patient representatives. The Steering Group is Chaired by Professor Peter Farndon. UKGTN aims to promote the provision of high quality equitable genetic testing services for NHS patients across the UK. This involves evaluating new tests that would not meet the NICE diagnostic selection criteria and recommending to specialised services commissioners those appropriate for service. There are 52 member laboratories from regional genetics and other specialist laboratories. A small project team and four working groups carry out the work on behalf of the Steering Group. The working group members are nominated representatives from healthcare professional groups, member laboratories and patient representatives from across the UK. UKGTN has established links with NICE Diagnostic Programme Board to ensure there is no duplication in the evaluation of genetic tests. UKGTN advises the Diagnostic Programme Board of new developments that have wider implications for NHS which may benefit from an evaluation by NICE. The UKGTN seeks to link the UKGTN Testing Criteria with NICE quality standards where appropriate. 1 RESPONSIBILITIES In what practical ways can the NHS Commissioning Board most effectively engage GP consortia in influencing the commissioning of national and regional specialised services and the commissioning of maternity services Care pathway management is the best way of involving the GP consortia in the management of services at all levels. The Map of Medicine provides a number of care pathways which could be linked to the developing NICE quality standards. Specialised laboratory services, including the companion diagnostics (e.g. herceptin), should be incorporated into the relevant pathways where applicable. How can the NHS Commissioning Board and GP consortia best work together to ensure effective commissioning of low volume services?. The Genetics Education and Development Centre engages with all clinicians in order to provide effective resources in the management of genetic conditions. For the commissioning of low volume services not covered by Specialised Services National Definition Set (SSNDS) it is critical that collaborative commissioning arrangements are developed between GP consortia including supporting governance arrangements or alternatively this responsibility could be placed with the NHS Commissioning Board working with GP consortia. FREEDOMS, CONTROLS AND ACCOUNTABILIES Are these the right criteria for an effective system of financial risk management? What support will GP consortia need to help hem manage risk UKGTN supports risk share across specialised services and its links with diagnostics. It considers that specialised services should have a standalone budget that is not linked with GP consortia as usually the referrers to medical genetics and requests for tests are from clinical consultants. Furthermore, as part of the care pathways for genetic conditions clinical consultants are tasked with gate keeping and triaging requests to ensure clinical appropriateness. Advances in genomic medicine will impact on all levels of commissioning including GP consortia who will commission services that are not contained in the SSNDS such as Haematology and Familial Hypercholesterolemia. It is important to recognise that specialties undertaking genetic tests can optimise efficiencies as the tests can replace other diagnostic investigations within the care pathway. Gene Dossiers include testing criteria which list the types of medical professionals that should be ordering the test and the phenotypic presentation where it would be appropriate to request testing. The testing criteria draws on information and evidence provided in the submitted evaluation forms. Healthcare professionals have reported that these criteria are a useful tool when considering whether or not to order a genetic test for a patient. Clinical scientists find it helpful when considering if it is appropriate to test and to gatekeep requests ensuring appropriate use of resources. Currently the UKGTN is gathering information on the current commissioning arrangements in place in each SCG for genetic testing services to inform a consistent approach to commissioning and inform model contracts including risk share. The UKGTN has worked in collaboration with the Clinical Molecular Genetics Society to develop a standard currency to measure workload in molecular genetics diagnostic laboratories. The unit of measurement is the final patient report which can be easily counted and represents the outcome of the molecular diagnostic process. A PCR amplicon or its equivalent grades the complexity of the 2 report. This is easily counted for any test and provides transparency. For each band a multiplier is assigned, the “weight” of that band. The number of reports issued for diseases in that band is multiplied by the weight for the band to give a final workload figure which has been termed Molecular Units – MolUs. The system is flexible and can be adapted to take account of developing technologies and automation. It is recognised that this system could be applied in development of national tariffs. The UKGTN supports the use of ICD-10 although UKGTN has found that it is not sufficient to cover all the genetic conditions for coding within Trusts. The UKGTN has been liaising with the National Genetics Reference Laboratory on the international development to improve the coding and classification of genetic conditions to address the deficit in information available for recording clinical management for rare conditions. It is expected that the World Health Organisation will publish ICD-11 in 2014 that will contain improved genetic coding. What are the key elements that you would expect to see reflected in a commissioning outcomes framework The UKGTN would expect to see standards for high quality services in the commissioning outcomes framework. The UKGTN promotes quality standards in genetic testing. UKGTN Membership is conditional on the laboratory meeting the required quality criteria (e.g. Clinical Pathology Accreditation) and participating in External Quality Assurance schemes. UKGTN membership is therefore an indicator of quality and provides reassurance in the safety of the testing services provided. The UKGTN has an internationally recognised process (commonly referred to as the “Gene Dossier process”) to evaluate new genetic tests (within its scope) being proposed for NHS service nationally from its member laboratories. Tests that meet the UKGTN evaluation process are recommended to commissioners for funding. The NHS Directory of Genetic Testing is reviewed annually listing all the tests that have been through this process and the associated testing criteria to promote appropriate referrals. Currently there are 487 diseases on Directory which equates to 659 tests (i.e. disease/gene pairs). The Genetic Alliance UK (formerly the Genetic Interest Group) reports that patients have recognised the increased availability of genetic tests because of the UKGTN system. Different approaches are used internationally, but the UK is seen as a world leader in an equitable provision of genetic tests The UKGTN recommends tests on the basis of testing criteria which essentially lists the types of medical professionals that should be ordering the test and the phenotypic presentation where it would be appropriate to request testing. The testing criteria draws on information and peer – reviewed evidence provided in the evaluation forms. Healthcare professionals have reported that these criteria are a useful tool when considering whether or not to order a genetic test for a patient. Clinical scientists find it helpful when considering if it is appropriate to test. The UKGTN, in collaboration with the PHG Foundation, has developed a commissioning guideline for ophthalmology services for patients with inherited eye conditions and will develop future commissioning guidelines as required for inherited conditions. Education in genetics for all disciplines within the NHS is essential. Clinical experts in genetics and non genetics across the disciplines have an important mutual role to play in order to develop skills and competencies within care pathways. The National Genetics Education and Development Centre provides resources to facilitate a wider knowledge base across specialities and commissioning organisations. 3 PARTNERSHIP How can GP consortia and the NHS Commissioning Board best involve patients in making decisions that are built on patient insight GP consortia and the NHS Commissioning Board would need to involve patient support groups and patients in decision making, especially around development of care pathways. Involvement could be from representatives nominated by patient support groups. Workshops and working groups focusing on particular areas of care and either nationally or regionally based could be used as a method to gain patient insight. The UKGTN is committed to working more closely with patient support groups and has already included patient representation by involving the main patient interest group for medical genetics, Genetic Alliance UK. This organisation is an umbrella group for over 130 individual support groups for inherited genetic conditions. The UKGTN and Genetic Alliance UK recently held a workshop to explore the problems encountered by patients with rare inherited conditions in getting a diagnosis. Following the workshop recommendations are being put forward to support professionals in diagnosing patients with rare inherited conditions. Future regular meetings between UKGTN and a range of patient support groups are planned to ensure that patients continue to have a strong voice in addressing key issues in their care pathway. How can multi-professional involvement in commissioning most effectively be promoted and sustained Multi professional involvement in commissioning can be promoted through professional networks that include all groups involved in delivering a service i.e. clinicians, commissioners, patients and other healthcare professionals involved in the care for example clinical scientists. UKGTN is an excellent example in a specialised service of how working collaboratively within a network enables an effective systematic approach to support the equitable commissioning of services. For rare conditions it may be more efficient to support national networks. The UKGTN, as the name suggests, is a network for the whole of the UK. It allows for co-ordination of genetic testing services across the UK and avoids duplication (by doing things once). It provides a one-stop forum for healthcare professionals involved in providing genetic services, patient support groups for inherited conditions and commissioners to influence policy development and national delivery of services. For example, the UKGTN supported the introduction of array CGH technology in cytogenetic laboratories by evaluating the clinical utility and providing robust advice to commissioners. The UKGTN website includes an online database which lists all the member laboratories and the testing services that they provide. This database is searchable by geographic area, by condition and by gene/OMIM number. Clinicians and scientists find the website an invaluable tool and the general public use it to see which centres provide which testing and may call the centres directly for clinical advice. 4