Sample mini 2
advertisement

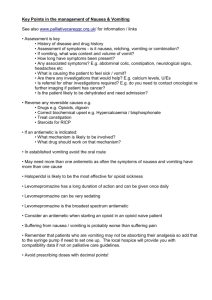
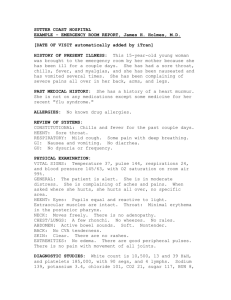
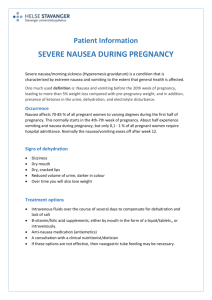
Client Situation This 85-year-old female presented to the ER on February 5th, with nausea and vomiting. Vitals were 35.6, 80, 18, 99/70, 98% R/A. Client had not been eating solid foods for past week and was also unable to tolerate fluids. Client had no BM times 3 days and no urine output on Feb. 5th. Client had gastric resection in 2004 for cancer and these current stomach problems are thought to be due to reoccurrence of the cancer and possible metastasis. Questionable GI obstruction. Client has a history of #rt. Hip, gallbladder removal, and has bilateral intraocular lens replacement. Tests are in the process of being performed to confirm a diagnosis of Ca of stomach with METS. Client is cheerful, but has little support and lives alone. Seems to be coping well with the reoccurrence of cancer and will be interesting to see how her coping ability continues as the disease progresses. Scientific Literature Rationale The incidence of gastric cancer has slowly decreased since 1960 but the reason for this is unknown. It is twice as common in men as in women, has a higher prevalence in whites and in individuals with pernicious anemia. There are no specific causes of gastric cancer, but latest research indicates that H. pylori increases the incidence of gastric cancer. Other factors thought to increase an individual’s likelihood of developing gastric cancer are diet, genetic factors and smoke (Black, Hawks, and Keene, 2001). Cancer usually arises in the mucosa lining and often spreads into the pancreas, liver, lungs, and bones. The prognosis for stomach cancer depends on the stage of the tumour and metastasis. The prognosis for an individual diagnosed with advanced gastric cancer is not good. The survival rate is almost zero (Black, Hawks, and Keene, 2001). Due to the area affected clients often experience nausea and vomiting. They are also at risk for altered nutrition and TPN or a jejunostomy tube may be used to help prevent malnutrition (Black, Hawks, and Keene, 2001). List of Prioritized Nursing Diagnostic Statements 1. Imbalanced nutrition: Less than body requirements r/t nausea and vomiting secondary to cancer of the stomach amb client taking in less than recommended daily intake. 2. Nausea r/t effects of cancer on stomach amb client experiencing nausea and vomiting. 3. Deficient fluid volume r/t vomiting and nausea amb decreased urinary output. 4. PC: GI bleeding 5. Impaired urinary elimination r/t decreased fluid intake amb decreased urinary output. 6. Constipation r/t possible obstruction secondary to cancer of the stomach amb no bowel movement times 3 days. 7. Risk for impaired oral mucous membranes r/t malnutrition. 8. Impaired comfort r/t effects of cancer on stomach amb client experiencing nausea and vomiting. 9. Risk for grieving r/t losses associated with cancer. 10. Risk for acute pain r/t effects of cancer on stomach. 11. Risk for self-care defecit sydrome r/t decreased self-care ability and lack of adequate supports and resources. Client Goals Client will be comfortable. Client Outcomes 1. Client’s nausea and vomiting will be controlled through medication administration by Feb. 15, 2005. 2. Client’s pain will be minimal while disease progresses (indefinite). Interventions Client and Nurse Interventions Diagnostic Statements A. Insure client is aware of the need to try and maintain nutrition 1, 2, 8 as long as this does not cause her discomfort. B. Eliminate noxious stimuli. 1, 2, 8 C. Medicate client for nausea and vomiting as needed. 1, 2, 8 D. Monitor nausea for any patterns related to time of day and if 1, 2, 8 nausea begins after drinking fluids. E. Monitor for vomitus (amount, time of day, blood). 2, 4 F. Medicate client prior to meals if client experiences nausea at 1, 2, 8 meal times. G. Provide good mouth care, especially after vomiting. 1, 7 H. Avoid lying flat after eating. 2 I. Encourage fluids. 1, 3, 5, 7 J. Ask client about fluids she likes and dislikes. 1, 3, 5 K. Monitor oral mucous membranes for breakdown (ex. Lesions 1, 7, 8 or inflammation). L. Monitor client for signs and symptoms of dehydration. 1, 3, 5, 7 M. Monitor client for signs and symptoms of GI bleeding. 4 N. Monitor urine for colour, cloudiness, and amount. 3, 5 O. Ask client about any genito-urinary symptoms. 5 P. Administer laxatives/stool softeners regularly. 6 Q. Schedule times for defecation into daily routine. 6 R. Provide client with privacy when using bathroom. 6 S. Monitor input and output. 1, 3, 5 T. Encourage activity. 6 U. Encourage fluid intake. 1, 3, 5, 7 V. Monitor results of tests for possible obstruction. 2, 6 W. Teach client about the importance of good oral hygiene. 1, 2, 3, 7, 8 X. Perform mouthcare after meals and before sleep. 7 Y. Lubricate lips as needed. 7 Z. Avoid alcohol based mouthwashes. 7 AA. Ask client if she is experiencing nausea and vomiting 1, 2, 8 and encourage her to tell me about any episodes of nausea and vomiting. BB. Ask client what can be done to make her feel more comfortable. CC. Develop therapeutic relationships with client. DD. Encourage client to discuss her feelings related to condition. EE.Determine support persons available to client. FF. Teach client that the grieving process is unique to each individual. GG. Provide support to family members. HH. Ask client if she is experiencing any pain. II. Administer medications for pain as needed. JJ. Assure client there is no reason to have pain, that medications can be helpful. KK. Assess any misconceptions client may have regarding pain medications (ex. Addiction). LL. Encourage client to perform ADL’s as able. MM. Encourage client to ask for help when needed. NN. Help client perform ADL’s when needed. OO. Schedule rest periods between ADL’s 8 9 9 9 9 9 8, 10 8, 10 8, 10 10 11 11 11 11 Evaluation Client’s diagnosis is still questionable. Diagnostic findings are not conclusive although there is evidence of cancer of the bowel. Due to client’s possible obstruction on clinical day, a medication used to help control her nausea and vomiting could not be administered and objective one was not met. I feel that this now this medication can now be administered, there will be less difficulty in controlling client’s nausea and vomiting. Interventions are still relevant and client did find several helpful. With changes in medications client’s nausea and vomiting should be effectively control. Client is still pain free and is comfortable despite the nausea and vomiting. Therefore client’s second objective and goal have been met and this will continue to be important goal and objective for client as her disease progresses especially due to her not being a candidate for surgery. Client’s lab values are becoming more unbalanced and appetite is still low. Her condition has changed very little from the past week but is likely to worsen as her disease progresses. Maintaining client’s comfort and preventing pain are still priorities in her nursing care.
![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)