Assessment Guideline for Bipolar - Behavioral Healthcare Providers
advertisement
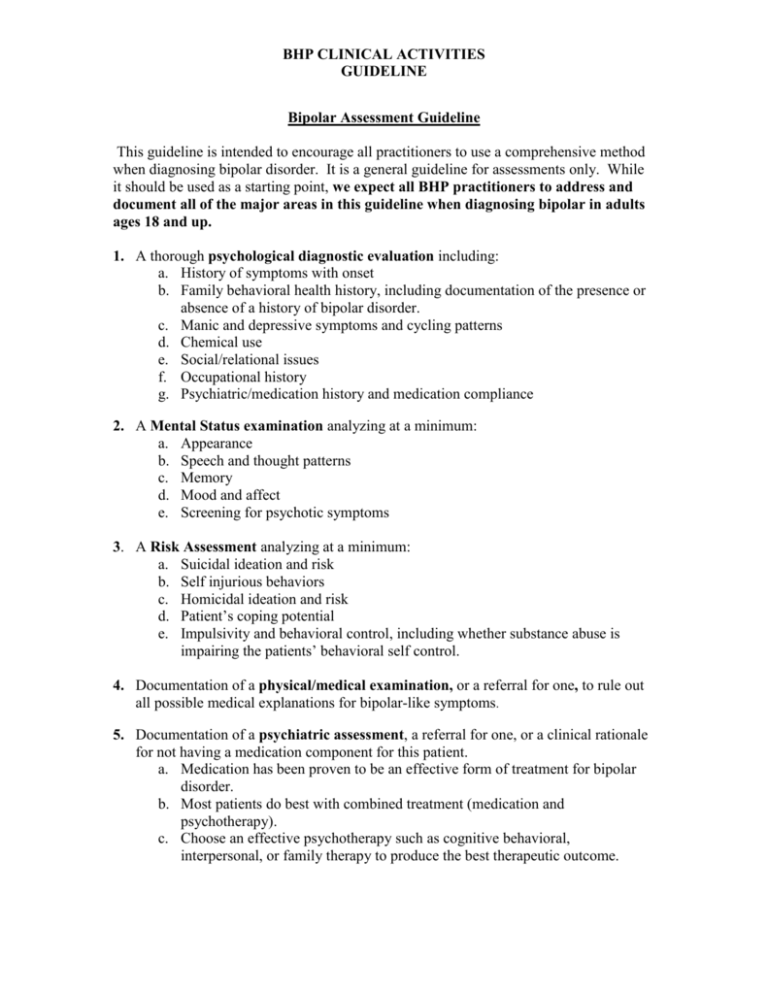
BHP CLINICAL ACTIVITIES GUIDELINE Bipolar Assessment Guideline This guideline is intended to encourage all practitioners to use a comprehensive method when diagnosing bipolar disorder. It is a general guideline for assessments only. While it should be used as a starting point, we expect all BHP practitioners to address and document all of the major areas in this guideline when diagnosing bipolar in adults ages 18 and up. 1. A thorough psychological diagnostic evaluation including: a. History of symptoms with onset b. Family behavioral health history, including documentation of the presence or absence of a history of bipolar disorder. c. Manic and depressive symptoms and cycling patterns d. Chemical use e. Social/relational issues f. Occupational history g. Psychiatric/medication history and medication compliance 2. A Mental Status examination analyzing at a minimum: a. Appearance b. Speech and thought patterns c. Memory d. Mood and affect e. Screening for psychotic symptoms 3. A Risk Assessment analyzing at a minimum: a. Suicidal ideation and risk b. Self injurious behaviors c. Homicidal ideation and risk d. Patient’s coping potential e. Impulsivity and behavioral control, including whether substance abuse is impairing the patients’ behavioral self control. 4. Documentation of a physical/medical examination, or a referral for one, to rule out all possible medical explanations for bipolar-like symptoms. 5. Documentation of a psychiatric assessment, a referral for one, or a clinical rationale for not having a medication component for this patient. a. Medication has been proven to be an effective form of treatment for bipolar disorder. b. Most patients do best with combined treatment (medication and psychotherapy). c. Choose an effective psychotherapy such as cognitive behavioral, interpersonal, or family therapy to produce the best therapeutic outcome. Exceptions to BHP Guidelines If a practitioner determines that major aspects of the guideline criteria are not appropriate for the member he/she is treating, or, if any aspect of the assessment portion of the guideline is not appropriate for the member, the practitioner must clearly document this in writing. The following documentation should exist in the assessment/treatment plans for the member: 1st Identify which of the major 5 numbered aspects of the criteria is being addressed. 2nd State clearly the reason why the suggested guideline criteria is not appropriate. 3rd State your alternative assessment or treatment plans. Evidence of a Physical or Medication Evaluation We do not require or believe that it is the job of the practitioner to ensure that the patient sought care by a medical physician but only that this was taken into account during the assessment. We do require that the practitioner ask about this, make a referral as indicated and document this in the chart. It is also beneficial to obtain medication adherence information as applicable. A medical provider may be a primary care physician, pediatrician, psychiatrist, physician assistant, advanced practice nurse or other independent medical practitioner, as appropriate to the age and issue of the patient. The following are acceptable means of evidence that the recommendation and/or occurrence of a physical/medication evaluation were taken into account. The presence of a medical write up, labs, other medical reports. 1) Documentation that patient was referred to/from a physician. 2) Co-existing charts between therapist and psychiatrist. 3) Documentation of refusal to see a physician 4) Evidence of exchange of information with a physician. Regulatory / External Resources: NCQA: QI 5.0. 7.0, 9.0 References: American Psychiatric Association. (2002). Practice guideline for the treatment of patients with bipolar disorder. American Journal of Psychiatry, 159(4). Frank, E., Kupfer, D., Thase, M., Mallinger, A., Swartz, H., Eagiolini, A., Grochocinski, V., Houck, P., Scott, J., Thompson, W., & Monk, T. (2005). Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Archives of General Psychiatry, 62(9), 996-1004. Minnesota Department of Human Services (2008). MHCP Provider Manual-Mental Health Services (Chapter 16). Ostacher, M., & Sachs, G. (2006). Update on bipolar disorder and substance abuse: Recent findings and treatment strategies. Journal of Clinical Psychiatry, 67(9). Thase, M. (2005). Bipolar depression: Issues in diagnosis and treatment. Harv. Rev. Psychiatry, 13(5), 257-271. Vieta, E., Pacchiarotti, I., Scott, J., Sanchez-Moreno, J., Di Marzo, S., & Colom, F. (2005). Evidence-based research on the efficacy of psychologic intervention in bipolar disorders: A critical review. Current Psychiatry Reports, 7, 449-455. Regulatory / External Resources: NCQA: QI 5.0. 7.0, 9.0 Date Effective: March, 2009 Date Reviewed by Clinical/QIC Team: March 2009, July 14, 2010; July 20, 2011, July 18, 2012