Learning and Development Committee
advertisement

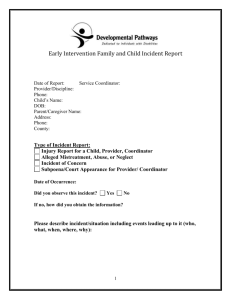
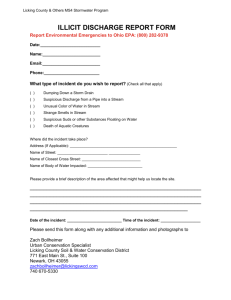
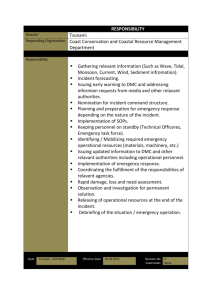
Adverse Incidents Policy 1 SCOPE This policy covers the reporting and examination of adverse incidents that occur in the context of the MHRT undertaking its functions. It will not include incidents that fall within the definition of a “blameworthy act” by an AMHS staff member, a suspected performance issue, or an issue that is under investigation by a relevant entity. It also does not include general complaints. 2 PURPOSE 2.1 To identify system failures that result in harm 2.2 To understand contributing factors and identify practically achievable actions to prevent future harm 3 REFERENCE 3.1 Compliments and Complaints Policy 3.2 Root Cause Analysis Training and Reference Manual, Queensland Health Patient Safety Centre 3.3 Queensland Health Clinical Incident Management Implementation Standard 3.4 Mental Health Act 2000 Section 438, Section 4 and Section 8. 4 DEFINITIONS 4.1 Adverse Incident – an event in which unintended or unnecessary harm resulted in association with an MHRT hearing. It includes actual harm and the threat of harm. It also includes a near miss/close call. 4.2 Harm – death, injury, and/or disability; unintended or unnecessary physical, psychological or social harm to a person. An example of harm may include patient suicide or other self-injury, actual assault of a person, verbal threats of violence, 4.3 “Blameworthy Act” means any of the following— (a) an intentionally unsafe act; (b) deliberate patient abuse; (c) conduct that constitutes a criminal offence (Health Services Act S 38O) 4.4 Contributing Factors – the events which contributed to the incident 4.5 Causal statement – a statement denoting a necessary relationship between one event (the cause) and another event (the effect) which is the direct consequence of the first event 4.6 Chain of events – refers to the concept that many contributing factors lead to an adverse incident rather than one single event 4.7 Corrective Action – direct actions taken in the short, medium and long-term to minimise risk of harm to persons Document Control: POAD01 Form No: POL/101 09/0115 Version No: 01 Page 1 of 3 “PRINTED COPIES ARE UNCONTROLLED” 4.8 Preventive Action – direct actions taken in the short, medium and long term to prevent harm to persons 4.9 Document – includes any part of a document in writing, any book, map, plan or drawing or other writing that identifies or describes anything; any device in which sound data is embodied; any device in which one or more images are embodied, and any other record of information (Evidence Act 1977) 4.10 Incident Severity Code – the assessment of consequences associated with an adverse incident, used to determine the appropriate level of analysis, action and escalation for adverse incidents. 5 PROCESS 5.1 Necessary Actions – MHRT staff and members directly involved in an adverse incident shall in the first instance attend to his/her own safety, and then the safety of the person harmed (patient, staff member). For example, immediate necessary actions may include use of the duress alarm to call hospital security, call for additional hospital staff, call for medical assistance. Intermediate actions may include relief from duty, support and/or counselling for staff or member directly involved. 5.2 Timing of Reporting – MHRT Staff and/or members who are involved directly or indirectly in an adverse incident, or become aware that an adverse incident has occurred shall report the incident immediately to the President or Executive Officer. Other stakeholders (including AMHS staff, non-government service providers, lawyers, support persons, and patients) who are involved directly or indirectly with an adverse incident in association with an MHRT hearing will also be encouraged to report the incident to the Tribunal President immediately. The timeframe for examining the incident will be a maximum of 30 working days. 5.3 Incident Severity Code determines: the level of escalation for notification the depth of analysis indicated time frames required Level 1 Level 2 Level 3 Incident resulting in death (e.g. suicide) or actual physical harm (e.g. assault); major rights infringement (e.g. breach of confidential information into the public arena) Incident involving threatening language, explicit threat of harm to self or others Near miss; no actual harm resulting however patient distress greater than what could reasonably be expected from a Tribunal hearing; concern for patient safety President notified same business day; Minister/Director-General/Director of Mental Health advised President notified next working day; AMHS Director/Manager advised President notified within 3-5 working days 5.4 Gathering Information – All persons involved directly or indirectly in the incident will be identified and given an opportunity to provide information about what happened. It may be necessary to speak to the people involved to gain more information. A plan of questioning will be Document Control: POAD01 Form No: POL/101 09/0115 Version No: 01 Page 2 of 3 “PRINTED COPIES ARE UNCONTROLLED” developed prior to any interview with any stakeholder. All interviewees will be given information about the process. A person may bring a support person to the interview if he/she wishes. Information should be gathered as close as possible in time to the incident. Questions should focus on what, why, when, where, how. Information gathering will also focus on the events leading up to the incident, and beyond the incident. No special privilege attaches to any information given except those relating to confidentiality under the Mental Health Act 2000. 5.5 Analysis – All the information will be integrated into a detailed chain of events document. The analysis will involve the formulation of a “problem statement” (i.e what happened, for example, “the patient hit a member of the treatment team in the face while leaving the hearing”). Immediate and intermediate contributing factors will then be considered. Problem Statement -> Immediate CF -> Intermediate CF -> Cause Immediate CF -> Intermediate CF -> Cause Immediate CF -> Intermediate CF -> Cause Immediate CF -> Intermediate CF -> Cause It is important to establish a link (why) between each of the boxes in the contributing factors diagram. It is then possible to develop causal statements and recommendations. Some causes are similar and can be grouped together. 5.6 Recommendations/Actions – recommendations may carry an effort/effect rating. For example: High effect – environmental changes; action by leader; simplify processes Moderate effect – checklist/cognitive aid; enhanced documentation; increase staffing/decrease workload Low effect – double checks, warnings/labels, new procedure/memo/policy; training Low end recommendations are those that are of low effect and require low effort. High end recommendations require high effort and are of high effect. An examination of an adverse incident should result in 1-3 recommendations/actions that: would have prevented the incident are practically achievable are robust and stand up to external scrutiny 5.7 Outcome measures - must be determined for each of the recommendations/actions. 6 ATTACHMENTS – Adverse Incidents Operational Procedure Document Control: POAD01 Form No: POL/101 09/0115 Version No: 01 Page 3 of 3 “PRINTED COPIES ARE UNCONTROLLED”