advances in cardiovascular-copper research
advertisement

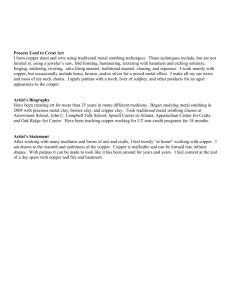
ADVANCES IN CARDIOVASCULAR-COPPER RESEARCH Leslie M. Klevay United States Department of Agriculture, Agricultural Research Service,Grand Forks Human Nutrition Research Center, Grand Forks, ND, USA Based on remarks at the First International Bio-Minerals Symposium of the International Association of Bioinorganic Scientists in Salt Lake City where Dr. Klevay received the Klaus Schwarz Commemorative Medal. Some of the concepts also were presented at the workshop “Ischemic Heart Disease and Malnutrition” at Experimental Biology ‘01 in Orlando and at the XVII World Congress of the International Society for Heart Research in Winnipeg. Abstract Copper frequently is low in the Western diet so closely associated with heart disease risk. Some of these diets are in the intake range used in successful depletion experiments of men and women and are low in comparison to suggested, desirable intakes. Assessment of nutritional status for copper is difficult. More than a dozen research articles reveal low organ copper and low activities of enzymes dependent on copper in people with cardiovascular disease. The nearly 80 identified anatomical, chemical and physiological similarities between animals deficient in copper and people with ischemic heart disease support the concept that these low concentrations of copper and low enzyme activities are indicative of poor copper status. Some links between the copper deficiency theory on the etiology and pathophysiology of ischemic heart and other general explanations for this illness have been found. The nutritional essentiality of copper was established for animals in 1928 when growth and hemoglobin improved after rats fed a cow’s milk diet were supplemented with copper; nutritional scientists studying copper became preoccupied with hematology for more than half a century(1). Now there is more research on cardiovascular effects of copper deficiency than on hematology(1). Although a link between copper and the cardiovascular system began to be made in 1939 by Bennetts and Hall(2), this shift in emphasis occurred gradually from the early 1970’s(1,3). Emphasis in this review will be restricted to copper deficiency and cardiovascular disease. Copper in the Western Diet Four successful copper depletion experiments with diets of conventional foods and involving more than 30 men and women have been summarized(4,5) revealing that daily copper intakes of 0.65 to 1.02 mg were insufficient. Approximately one-third of daily diets in Belgium, Canada, the United Kingdom and the United States are within this range(6,7). Recent results on daily intakes of 80 men and women randomly selected in Baltimore are consonant(8). It is possible to interpolate the graph of these authors to reveal 36 and 60% of daily copper intakes are less than the recently published Estimated Average Requirement and the Recommended Dietary Allowance, respectively, for adults(9). Assessment of Nutriture Assessment of nutritional status, or nutriture, is not always easy. Dann and Darby(10) described five zones of nutriture from saturation, i.e., maximal storage without early toxicity, to clinically manifest nutritional disease which, when severe, can be diagnosed without the assistance of the laboratory. Although they emphasized vitamins, their principles are equally applicable to trace elements(11). Golden(12) includes copper among the nutrients that are reduced in tissue concentration in deficiency. Numerous experiments with animals support this statement. Prohaska (13) tabulated some cuproenzymes that are altered in copper deficiency. Extracellular superoxide dismutase, lysyl oxidase and Cu, Zn-superoxide dismutase (EC 1.15.1.1) were prominent. Lysyl oxidase (EC 1.4.3.6) is required for the cross linking of collagen and elastin. The superoxide dismutases protect against oxidative damage. Enzyme activities and copper concentrations are suggested as being potentially useful in diagnosing copper deficiency with no single indicator being adequate in all situations(9). Decreased tissue concentration or decreased enzyme activity may correspond to Dann and Darby’s third and fourth zones of nutriture: potential and latent deficiency disease(10). Signs of Low Copper Nutriture? Several authors have found a decrease in the concentration of copper in the presumably normal heart muscle of people with ischemic heart disease in comparison to accident victims, et c.(14-18). Low copper in leucocytes has been found in men with poor coronary arteries on angiograms(19) and in Japanese who live in Brazil where heart disease risk is high in comparison to Japan, where risk is low(5,20). Tilson and Dubick et al. found low liver copper(21) and decreased aortic superoxide dismutase(22), respectively, in people with aortic aneurysm. Others have found decreases in copper dependent enzymes in people with abnormal cardiovascular physiology or structure. Vivoli et al.(23) and Bergomi et al.(24,25) found inverse correlations between blood pressure and superoxide dismutase activity and lysyl oxidase, respectively, in hypertension. The results of Russo et al. were similar(26). Angiogram patients with a history of myocardial infarction had less superoxide dismutase in plasma than similar patients without such a history(27). Decreased activity also was found in diseased coronary arteries(28). Perhaps people with low enzyme activities are people who habitually eat diets low in copper. If so, then ischemic heart disease corresponds to Dann and Darby’s fifth zone of nutriture: clinically manifest deficiency disease(10). These observations can be interpreted as evidence of copper deficiency only if other observations are corroborative. Rock et al.(29) supplemented healthy, middle-aged people with copper and found their red cells to be less easily oxidized in vitro after six weeks of supplementation. This experiment reveals that healthy people may benefit from higher copper intakes. Similarities Between Copper Deficiency and Ischemic Heart Disease Tables 1-3 summarize anatomical, chemical and physiological similarities between animals deficient in copper and people with ischemic heart disease. Tabulation of these similarities began in 1987(30). The titles of the tables were changed from ‘similarities between’ to ‘the anatomy of ’ in 2000(5). The number of tabulated entries has grown more than 6-fold from the dozen(31), when I first began to notice the likeness of the two syndromes, until now. The work of numerous authors is incorporated into Tables 1-3. Their work has been cited in earlier writings; citation of most primary references is omitted here for the sake of brevity. Table 1. The Anatomy of Copper Deficiency and Ischemic Heart Disease Aortic valve thickening Arterial Elastic degeneration Fibrosis Foam cells Hemorrhage (intramural) Mucopolysaccharide increase Necrosis Smooth muscle proliferation Atrial Thrombosis Bone density decrease Coronary artery Dissecting aneurysms Elastic fragmentation Hyalinization Necrosis Smooth muscle degeneration Sudanophilia Thrombosis Hemopericardium Hemothorax Myocardial infarction Pericarditis Pleural effusion Ruptured papillary muscle Small stature Ventricular Aneurysm Calcification Edema Fibrosis Hemorrhage (focal) Hypertrophy Infiltration (neutrophil and round cell) Myocyte-myocyte struts decreased Necrosis (myocardial cell) Rupture Thrombosis (endocardial) Table 2. The Chemistry of Copper Deficiency and Ischemic Heart Disease Decreased Cardiac copper Cardiac iron Dihomo-y-linolenic acid Hepatic zinc Lecitin:cholesterol acyltransferase Leucocyte copper Lipoprotein lipase Na/K-ATPase Myocardial cytochrome oxidase Plasma retinol Exacerbated by Homocysteine Ironb Salt a - Risk factor. See Table 1 for further explanation. b - Newly added, see text. Increased Cardiac sodium Cholesterolemiaa Serum ferritin Homocysteinemiab Thiobarbituric acid reactive substances Thromboxane A2/prostacyclin Triglyceridemia Uricemia Mitigated by Aspirin Beer Clofibrate Table 3. The Physiology of Copper Deficiency and Ischemic Heart Disease Abnormal electrocardiograms Blocks bundle brancha first degree second degree third degree Decreased Arterial dilation with acetylcholine Blood pressure under load Glucose tolerancea Hearing Longevity Exacerbated by His-ventricular interval increased Pathological Q waves P wave morphology altered QT interval increased R waves are tall ST segmenta Ventricular premature beats Pregnancy Increased Blood pressurea Euglobulin clot lysis time Female thrombosis Male sudden death a - Risk factor. See Table 1 for further explanation. It is important to realize that each entry in these tables represents observations made both on deficient animals and sick people, often based on several observations on each group. My seven intervening theoretical articles cite hundreds of research articles. Enumeration and citation here are restricted either to similarities found recently or to recently found references to similarities found earlier. The observations on people are based mainly on epidemiology and pathology, although some are from noninvasive, diagnostic procedures. The observations on animals are taken from numerous experiments on copper deficiency made since 1928(32). Together, these collected observations and their accompanying discussion in my earlier writing provide the basis for what may become a unified theory of the etiology and pathogenesis of ischemic heart disease(33). In retrospect, many of the experiments can be considered successful attempts to produce characteristics of ischemic heart disease in animals deficient in copper. As noted above, the superoxide dismutases dependent on copper protect against oxidative damage. The thiobarbituric acid reactive substances in Table 2 are indicative of oxidative damage. Because animals deficient in copper can be somewhat protected from this deficiency by dietary antioxidants and because the hypercholesterolemia, hypertension, hypercoagulability of blood(34) and endothelial vasodilator function have evidence of impaired oxidative defense(35), copper may be an antioxidant nutrient for cardiovascular health (34). Anatomy Rate of loss of bone mineral density in the hip was associated directly with increased mortality from coronary heart disease(36). Cardiac enlargement in copper deficiency has been found again(37). Chemistry Aspirin mitigated copper deficiency(38,39), at least in part, by increasing liver copper(40). Serum cholesterol is low in people with Wilson’s disease, probably because of the increased liver copper(33). Observations from Framingham showing that uricemia can be used to predict heart disease mortality have been confirmed(41,42). Elevated plasma homocysteine is an independent risk factor for premature coronary atherosclerosis in men(43). Homocysteine is increased in plasma of rats deficient in copper(44); high homocysteine also interferes with copper utilization(45). Salonen, et al.(46) suggested high stored iron, as assessed by serum ferritin, is an independent risk factor for coronary heart disease. Rats fed marginal copper can be made deficient by a high intake of iron(47). Copper in heart, liver and plasma was decreased and plasma cholesterol was increased. Physiology The decreased hearing in elderly people exacerbated by hypertension and hypercholesterolemia(48) increases the association between hearing loss and ischemic heart disease(5). This phenomenon may result from a greater sensitivity to noise if feeding cholesterol to chinchillas(49) produces alterations in copper utilization as have been found in other species(50,51) (see below). The Lipid Hypothesis The lipid hypothesis probably is the most widely accepted and most intensively studied hypothesis on the origin of ischemic heart disease. In brief, large amounts of dietary fat are toxic. Failures of the lipid hypothesis in addition to those mentioned here can be found in earlier writings(5,30,33,52-54). This hypothesis, in reality at least three separate hypotheses(30,52,53), has failed to explain much of ischemic heart disease. Most important, perhaps, are the lack of relationship of fat intakes to risk when data are collected in single nations(52,55), freedom from heart disease with high plasma cholesterol and heart disease with low cholesterol(5), and lack of association between dietary fat intake and serum cholesterol(56,57). If nearly everyone in the wealthiest nations eats too much of the wrong kind of fat, then dietary fat is not of epidemiologic interest(55). Epidemiology has not revealed that women eat less, or better fat, than men. Nor is there an experiment showing that women (or female animals) tolerate fat better than men (or male animals). Differences in fat consumption cannot explain why men with ischemic heart disease tend to die suddenly(5,58,59) and women tend to die with thrombosis(5,58), seasonal variations in cholesterol or statistical associations between paired risk factors such as serum uric acid and cholesterol(5). Plasma homocysteine also can be predicted by measurement of total cholesterol or blood pressure in Norwegians(60). Other characteristics of ischemic heart disease unexplained by dietary fat were discussed earlier(5). Recently a systematic review of 27 trials stating the intention to reduce or modify fat intake revealed that cardiovascular mortality could be reduced by these measures. Longer trials provided stronger evidence of protection, but there was little effect on total mortality(61). It seems that this dietary change can change the words (not the date) on the death certificate(62,63). Other dissents from the lipid hypothesis are available(64-67). Animal Models of Human Disease Agents suspected of causing human illness should be able to produce characteristics of the illness in animals. This production may be difficult, and may not occur for all phenomena or in all species. In general, medicine has advanced when illnesses similar to those of people have been produced in animals by putative agents. Skepticism is proper when an hypothesis has been advanced for many years and yet evidence from animals is minimal or lacking. It is surprising how few of the characteristics of ischemic heart disease have been produced in animals fed various amounts and types of dietary lipid (5). Abnormal electrocardiograms, glucose intolerance and hyperuricemia are prominent among these characteristics. Experimental production in animals of characteristics of ischemic heart disease is particularly important in view of Stehbens’ contention(65,66) that coronary heart disease and atherosclerosis are not as closely associated as is generally believed. Conversely, when putative agents produce illness in animals only because of unsuspected properties such as a chemical impurity, the hidden characteristic is revealed to be the actual agent. Examples are the minor constituent of tryptophan supplements in producing the eosinophilia myalgia syndrome(68,69) and contaminated meperidine in rapidly producing acute severe parkinsonism(70). There has been much effort devoted to producing atherosclerosis, in contrast to ischemic heart disease, in animals. Experimental diets containing cholesterol or cholesterol plus cholic acid to produce atherosclerosis were introduced in the first quarter of the 20th century. These diets were shown to disrupt copper utilization later(50,51); results have been confirmed and extended(71-73). It may be appropriate to revise interpretations of experiments in which these dietary additives were used and to reformulate resulting hypotheses. Phenomena attributed to dietary cholesterol in reality may have been the result of copper deficiency as was found for some diets high in lard(74) without the additives. Copper deficiency seems to produce lesions both resembling atherosclerosis and characteristics of ischemic heart disease in animals. General Explanations of Ischemic Heart Disease Long ago I read a poem(75) which seems to apply to ischemic heart disease. Blind men visited an elephant to learn its properties. Each evaluated only part of the elephant, but attempted to conceptualize its entirety. Individual inferences were correct, were narrow and were inadequate to characterize the elephant as a whole (Figure 1). The elephant was thought to be similar to a rope, a tree, a wall, et c. I think it is important to consider all aspects of ischemic heart disease, not only those aspects related to lipid metabolism(54). Chamberlin(76) urges ‘’the method of multiple working hypotheses’’ when studying complex phenomena to promote thoroughness and to prevent neglect of important data. Theories attempting to explain important natural phenomena have been found wanting historically if they explained only limited characteristics of the phenomena(77,78). Kuhn argues that theories incorporating other theories contribute to scientific progress(30,33,79). McCormick(80) has referred to the multifactorial aetiology of coronary heart disease as a dangerous delusion. I have illustrated how the term ‘’multifactorial’’ could have been applied to pellagra(81), scurvy(53) and beri beri(55) if it had been in the medical vocabulary when these illnesses were considered as complicated as is ischemic heart disease today. It is, and has been, my hope that ischemic heart disease eventually will be simplified to the degree that these deficiency diseases have been simplified. Questions arise. What produces the phenomena in Tables 1-3 and other characteristics of ischemic heart disease such as arterial spasm and endothelial damage, connective tissue damage...thrombi, and so on(33,53,54)? What determines who lives long and who dies early of ischemic heart disease when people eat the Western diet for a lifetime? Four general explanations have been advanced to answer these questions. The lipid hypothesis may have outlived its usefulness(5) and will not be discussed further. The homocysteine hypothesis of McCully(82,83) and the iron hypothesis of Sullivan(67,84,85) provide unifying ideas(5) that may be helpful in understanding the origins of the many phenomena of ischemic heart disease. Barker has advanced the fetal programming hypothesis in two editions of his book (54). In brief, small babies who do not catch up in growth in a year are likely to be hypertensive and glucose intolerant in middle age. Numerous research articles develop and refine the ideas of these authors. The copper deficiency theory is offered as the simplest and most general explanation of the etiology and pathophysiology of ischemic heart disease(5). Some links between this theory and other explanations that have been proposed have been provided here and elsewhere(30,52). Copper deficiency has produced more characteristics of ischemic heart disease in animals than has any other nutritional insult. This production supports the belief that low copper concentrations and low activities of enzymes dependent on copper in people with cardiovascular disease are signs of poor copper nutriture. If copper deficiency is the leading nutritional deficiency, world wide, of agricultural animals(86), can people be far behind? Figure 1 Legend The poem can be found at http://www.wordfocus.com/word-act-blindmen.html. My thanks to my cousin Theodore C. Klevay for the cartoon used with permission. References 1. L.M. Klevay, (1997) Copper as a supplement to iron for hemoglobin building in the rat (Hart et al., 1928). J. Nutr., 127, 1034S-1036S. 2. H.W. Bennetts and H.T. Hall, (1939) "Falling Disease" of cattle in the south-west of western Australia. Aust. Vet. J., 15, 152-159. 3. L.M. Klevay, (2000) Cardiovascular disease from copper deficiency--a history. J. Nutr., 130, 489S492S. 4. L.M. Klevay and D.M. Medeiros, (1996) Deliberations and evaluations of the approaches, endpoints and paradigms for dietary recommendations about copper. J. Nutr., 126, 2419S-2426S. 5. L.M. Klevay, (2000) Trace element and mineral nutrition in disease: Ischemic heart disease. In Clinical nutrition of the essential trace elements and minerals: The guide for health professionals, J.D.Bogden and L.M.Klevay, eds., Humana Press Inc., Totowa, NJ. Pp. 251-271. 6. L.M. Klevay, J.P. Buchet, V.W. Bunker, B.E. Clayton, R.S. Gibson, D.M. Medeiros, P.B. MoserVeillon, K.Y. Patterson, L.J. Taper, and W.R. Wolf,Copper in the western diet (Belgium, Canada, U.K. and USA). In Trace Elements in Man and Animals - TEMA 8, M.Anke, D.Meissner, and C.F.Mills, eds., (1993) Verlag Media Touristik, Gersdorf, Germany. Pp. 207-210. 7. L.M. Klevay, (1998) Lack of a recommended dietary allowance for copper may be hazardous to your health. J. Am. Coll. Nutr., 17, 322-326. 8. Y. Pang, D.L. MacIntosh, and P.B. Ryan, (2001) A longitudinal investigation of aggregate oral intake of copper. J Nutr. , 131, 2171-2176. 9. Copper. In Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium and zinc, National Academy of Sciences, Washington, D.C. (2001) Pp. 7.1-7.27. 10. W.J. Dann and W.J. Darby, (1945) The appraisal of nutritional status (nutriture) in humans; With especial reference to vitamin deficiency disease. Physiol. Rev., 25, 326-346. 11. L.M. Klevay, Dietary requirements for trace elements in humans. In Trace element-analytical chemistry in medicine and biology, vol. 4, P.Brätter and P.Schramel, eds., Walter de Gruyter & Co., Berlin. (1987) Pp. 43-60. 12. M.H.N. Golden,Severe malnutrition. In Oxford Textbook of Medicine, D.J.Weatherall, J.G.Ledingham, and D.A.Warrell, eds., Oxford University Press, Oxford. (1996) Pp. 1278-1296. 13. J.R. Prohaska, (1990) Biochemical changes in copper deficiency. J. Nutr. Biochem., 1, 452-461. 14. P.O. Wester, (1965) Trace elements in human myocardial infarction determined by neutron activation analysis. Acta Med. Scand., 178, 765-788. 15. T.W. Anderson, L.C. Neri, G.B. Schreiber, F.D. Talbot, and A. Zdrojewski, (1975) Ischemic heart disease, water hardness and myocardial magnesium. Can. Med. Assoc. J., 113, 199-203. 16. B. Chipperfield and J.R. Chipperfield, (1978) Differences in metal content of the heart muscle in death from ischemic heart disease. Am. Heart J., 95, 732-737. 17. O. Penttilä, P.J. Neuvonen, J.J. Himberg, P. Siltanen, A. Järvinen, and E. Merikallio, (1986) Auricular myocardial cation concentrations in certain heart diseases in man. Trace Elem. Med., 3, 47-51. 18. N. Zama and R.L. Towns, (1986) Cardiac copper, magnesium, and zinc in recent and old myocardial infarction. Biol. Trace Elem. Res., 10, 201-208. 19. G.D. Kinsman, A.N. Howard, D.L. Stone, and P.A. Mullins, (1990) Studies in copper status and atherosclerosis. Biochem. Soc. Trans., 18, 1186-1188. 20. G.W. Mielcarz, A.N. Howard, N.R. Williams, G.D. Kinsman, E. Moriguchi, Y. Moriguchi, S. Mizushima, and Y. Yamori, (1997) Copper and zinc status as a risk factor for ischemic heart disease: A comparison between Japanese in Brazil and Okinawa. J. Trace Elem. Exp. Med., 10, 29-35. 21. M.D. Tilson, (1982) Decreased hepatic copper levels. A possible chemical marker for the pathogenesis of aortic aneurysms in man. Arch. Surg., 117, 1212-1213. 22. M.A. Dubick, C.L. Keen, R.A. DiSilvestro, C.D. Eskelson, J. Ireton, and G.C. Hunter, (1999) Antioxidant enzyme activity in human abdominal aortic aneurysmal and occlusive disease. Proc. Soc. Exp. Biol. Med., 220, 39-45. 23. G. Vivoli, M. Bergomi, S. Rovesti, M. Pinotti, and E. Caselgrandi, (1995) Zinc, copper, and zinc- or copper-dependent enzymes in human hypertension. Biol. Trace Elem. Res., 49, 97-106. 24. M. Bergomi, S. Rovesti, M. Vinceti, R. Vivoli, E. Caselgrandi, and G. Vivoli, (1997) Zinc and copper status and blood pressure. J. Trace Elem. Med. Biol., 11, 166-169. 25. L.M. Klevay, (1998) Comments on Bergomi, et al. J. Trace Elem. Med. Biol., 12, 1. 26. C. Russo, O. Olivieri, D. Girelli, G. Faccini, M.L. Zenari, S. Lombardi, and R. Corrocher, (1998) Anti-oxidant status and lipid peroxidation in patients with essential hypertension. J. Hypertens., 16, 1267-1271. 27. X.L. Wang, T. Adachi, A.S. Sim, and D.E. Wilcken, (1998) Plasma extracellular superoxide dismutase levels in an Australian population with coronary artery disease. Arterioscler. Thromb. Vasc. Biol., 18, 1915-1921. 28. U. Landmesser, R. Merten, S. Spiekermann, K. Buttner, H. Drexler, and B. Hornig, (2000) Vascular extracellular superoxide dismutase activity in patients with coronary artery disease: relation to endothelium-dependent vasodilation. Circulation, 101, 2264-2270. 29. E. Rock, A. Mazur, J.M. O'Connor, M.P. Bonham, Y. Rayssiguier, and J.J. Strain, (2000) The effect of copper supplementation on red blood cell oxidizability and plasma antioxidants in middleaged healthy volunteers. Free Radic. Biol. Med., 28, 324-329. 30. L.M. Klevay, (1987) Ischemic heart disease. A major obstacle to becoming old. Clin. Geriatr. Med., 3, 361-372. 31. L.M. Klevay, (1980) Interactions of copper and zinc in cardiovascular disease. Ann. N. Y. Acad. Sci., 355, 140-151. 32. E.B. Hart, H. Steenbock, J. Waddell, and C.A. Elvehjem, (1928) Iron in nutrition. VII. Copper as a supplement to iron for hemoglobin building in the rat. J. Biol. Chem., 77, 797-812. 33. L.M. Klevay, (1990) Ischemic heart disease: toward a unified theory. In Role of Copper in Lipid Metabolism, K.Y.Lei and T.P.Carr, eds., CRC Press, Boca Raton. Pp. 233-267. 34. K.G. Allen and L.M. Klevay, (1994) Copper: an antioxidant nutrient for cardiovascular health. Curr. Opin. Lipidol., 5, 22-28. 35. S.M. Lynch, B. Frei, J.D. Morrow, L.J. Roberts, A. Xu, T. Jackson, R. Reyna, L.M. Klevay, J.A. Vita, and J.F. Keaney, Jr., (1997) Vascular superoxide dismutase deficiency impairs endothelial vasodilator function through direct inactivation of nitric oxide and increased lipid peroxidation. Arterioscler. Thromb. Vasc. Biol., 17, 2975-2981. 36. D.M. Kado, W.S. Browner, T. Blackwell, R. Gore, and S.R. Cummings, (2000) Rate of bone loss is associated with mortality in older women: a prospective study. J Bone Miner. Res, 15, 1974-1980. 37. C. Farquharson and S.P. Robins, (1988) Female rats are susceptible to cardiac hypertrophy induced by copper deficiency: the lack of influence of estrogen and testosterone. Proc. Soc. Exp. Biol. Med. , 188, 272-281. 38. A. Lopez-Anaya, C. Dawson, C. Gonzales, M. Bacolod, and V. Kishore, (1994) Pharmacokinetics and pharmacodynamics in copper deficiency. I. Antiinflammatory activity of aspirin. Biol. Trace Elem. Res. , 40, 161-176. 39. M. Fields, C.G. Lewis, and I. Bureau, (2001) Aspirin reduces blood cholesterol in copper-deficient rats: a potential antioxidant agent? Metabolism, 50, 558-561. 40. L.M. Klevay, (1986) Aspirin hypocholesterolemia associated with increased microsomal copper in liver. Nutr. Res., 6, 1281-1292. 41. J. Fang and M.H. Alderman, (2000) Serum uric acid and cardiovascular mortality the NHANES I epidemiologic follow-up study, 1971-1992. National Health and Nutrition Examination Survey. JAMA, 282, 2404-2410. 42. M. Tomita, S. Mizuno, H. Yamanaka, Y. Hosoda, K. Sakuma, Y. Matuoka, M. Odaka, M. Yamaguchi, H. Yosida, H. Morisawa, and T. Murayama, (2000) Does hyperuricemia affect mortality? A prospective cohort study of Japanese male workers. J Epidemiol., 10, 403-409. 43. J.J. Genest, J.R. McNamara, D.N. Salem, P.W. Wilson, E.J. Schaefer, and M.R. Malinow, (1990) Plasma homocysteine levels in men with premature coronary artery disease. J. Am. Coll. Cardiol., 16, 1114-1119. 44. T. Tamura, K.H. Hong, Y. Mizuno, K.E. Johnston, and C.L. Keen, (1999) Folate and homocysteine metabolism in copper-deficient rats. Biochim. Biophys. Acta, 1427, 351-356. 45. J.C. Brown and J.J. Strain, (1990) Effect of dietary homocysteine on copper status in rats. J. Nutr., 120, 1068-1074. 46. J.T. Salonen, Nyyss, H. Korpela, J. Tuomilehto, R. Seppanen, and R. Salonen, (1992) High stored iron levels are associated with excess risk of myocardial infarction in eastern Finnish men. Circulation, 86, 803-811. 47. L.M. Klevay, Iron overload can induce mild copper deficiency. (2001) J. Trace Elem. Med. Biol., 14, 237-240. 48. Y.L. Chen and Y.P. Ding, (1999) Relationship between hypertension and hearing disorders in the elderly. East. Afr. Med. J., 76, 344-347. 49. T. Morizono and M.A. Sikora, (1982) Experimental hypercholesterolemia and auditory function in the chinchilla. Otolaryngol. Head. Neck Surg., 90, 814-818. 50. L.M. Klevay, (1982) Metabolic interactions among cholesterol, cholic acid and copper. Nutr. Rep. Int., 26, 405-414. 51. L.M. Klevay, (1988) Dietary cholesterol lowers liver copper in rabbits. Biol. Trace Elem. Res., 16, 51-57. 52. L.M. Klevay, (1983) Copper and ischemic heart disease. Biol. Trace Elem. Res., 5, 245-255. 53. L.M. Klevay, The role of copper, zinc, and other chemical elements in ischemic heart disease. In Metabolism of Trace Metals in Man, Vol. 1, O.M.Rennert and W.Y.Chan, eds., CRC Press, Boca Raton, FL. (1984) Pp. 129-157. 54. L.M. Klevay, (1993) Ischemic heart disease: nutrition or pharmacotherapy? J. Trace Elem. Electrolytes Health Dis., 7, 63-69. 55. L.M. Klevay, (1990) Some environmental aspects of ischaemic heart disease. Environ. Management Health, 1, 9-17. 56. T.Gordon. Section 24: The Framingham Study-An epidemiological investigation of cardiovascular disease. 9. 1970. Washington,D.C., U.S. Government Printing Office. 57. W.R. Harlan, A.L. Hull, R.P. Schmouder, F.E. Thompson, F.A. Larkin, and J.R. Landis, (1983) Dietary intake and cardiovascular risk fac- tors, Part II. Serum urate, serum cholesterol, and correlates. Vital Health Stat., 11, 1-94. 58. R.E. Spiekerman, J.T. Brandenburg, R.W. Achor, and J.E. Edwards, (1962) The spectrum of coronary heart disease in a community of 30,000: A clinicopathologic study. Circulation, 25, 57-65. 59. D.J. Lerner and W.B. Kannel, (1986) Patterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am. Heart J., 111, 383-390. 60. O. Nygärd, S.E. Vollset, H. Refsum, I. Stensvold, A. Tverdal, J.E. Nordrehaug, P.M. Ueland, and G. Kvale, (1995) Total plasma homocysteine and cardiovascular risk profile The Hordaland homocysteine study. JAMA, 274, 1526-1533. 61. L. Hooper, C.D. Summerbell, J.P. Higgins, R.L. Thompson, N.E. Capps, G.D. Smith, R.A. Riemersma, and S. Ebrahim, (2001) Dietary fat intake and prevention of cardiovascular disease: systematic review. Br. Med. J., 322, 757-763. 62. L.M. Klevay, (1987) Cholesterol reduction: Safety, other concerns. Ann. Intern. Med., 107, 421. 63. L.M. Klevay, (1990) Motivation for cholesterol screening. J. Lab. Clin. Med., 115, 263-264. 64. U. Ravnskov, The cholesterol myths. Exposing the fallacy that cholesterol and saturated fat cause heart disease , New Trends Pub., Washington, D.C., (2000). 65. W.E. Stehbens, (2001) Coronary heart disease, hypercholesterolemia, and atherosclerosis. I. False premises. Exp. Mol. Pathol., 70, 103-119. 66. W.E. Stehbens, (2001) Coronary heart disease, hypercholesterolemia, and atherosclerosis. II. Misrepresented data. Exp. Mol. Pathol., 70, 120-139. 67. J.L. Sullivan, (1996) Iron versus cholesterol--perspectives on the iron and heart disease debate. J. Clin. Epidemiol., 49, 1345-1352. 68. J.L. Troy, (1991) Eosinophilia-myalgia syndrome. Mayo Clin. Proc., 66, 535-538. 69. F.L. Mastaglia, (2001) Iatrogenic (drug-induced) disorders of the nervous system. In Neurology and general medicine, M.J.Aminoff, ed., Churchill Livingstone,Pp. 593-615. 70. C.D. Marsden, (1996) Movement disorders. In Oxford Textbook of Medicine, vol. 3, D.J.Weatherall, J.G.Ledingham, and D.A.Warrell, eds., Oxford University Press, Oxford. Pp. 39984022. 71. M. Vlad, E. Bordas, R. Tomus, D. Sava, E. Farkas, and G. Uza, (1993) Effect of copper sulfate on experimental atherosclerosis. Biol. Trace Elem. Res., 38, 47-54. 72. M. Vlad, G. Uza, M. Zirbo, and D. Olteanu, (1995) Free radicals, ceruloplasmin, and copper concentration in serum and aortic tissue in experimental atherosclerosis. Nutrition, 11, 588-591. 73. D.J. Lamb, G.L. Reeves, A. Taylor, and G.A. Ferns, (1999) Dietary copper supplementation reduces atherosclerosis in the cholesterol-fed rabbit. Atherosclerosis, 146, 33-43. 74. L.M. Klevay, (1985) Atrial thrombosis, abnormal electrocardiograms and sudden death in mice due to copper deficiency. Atherosclerosis, 54, 213-224. 75. J.G. Saxe, The blind men and the elephant. In A treasury of the familiar, vol. 1, R.L.Woods, ed., Spencer Press, Chicago. (1942) Pp. 8-9. 76. T.C. Chamberlin, (1965) The method of multiple working hypotheses. Science, 148, 754-759. 77. W.D. Bancroft, (1931) How to ripen time. J. Physical. Chem., 35, 1904-1921. 78. J. Neyman, Introduction: Copernicus (Mikolaj Kopernik): An Intellectual Revolutionary. In The heritage of Copernicus: Theories "pleasing to the mind", (1974) Pp. 1-22. 79. T.S. Kuhn, The Structure of Scientific Revolutions,2 ed., The University of Chicago Press, Chicago, (1970) Pp. 95,154,169. 80. J. McCormick, (1988) The multifactorial aetiology of coronary heart disease: a dangerous delusion. Perspect. Biol. Med., 32, 103-108. 81. L.M. Klevay, The role of copper and zinc in cholesterol metabolism. In Advances in Nutritional Research, Vol. 1, H.H.Draper, ed., Plenum Publishing Corp., New York. (1977) Pp. 227-252. 82. K.S. McCully, The Homocysteine Revolution, Keats Publishing, Inc., New Canaan, (1997). 83. K.S. McCully and M. McCully, The heart revolution :the B vitamin breakthrough that lowers homocysteine, cuts your risk of heart disease, and protects your health,1st ed. ed., Harper Collins, New York, NY, (1999). 84. J.L. Sullivan, (1981) Iron and the sex difference in heart disease risk. Lancet, 1, 1293-1294. 85. J.L. Sullivan, (1996) Iron versus cholesterol--response to dissent by Weintraub et al. J. Clin. Epidemiol., 49, 1359-1362. 86. C.F. Mills, Changing perspectives in studies of the trace elements and animal health. In Trace elements in man and animals-TEMA 5, C.F.Mills, I.Bremner, and J.K.Chesters, eds., Commonwealth Agricultural Bureaux, Farnham Royal, U.K. (1985) Pp. 1-10.