low level of concern
advertisement

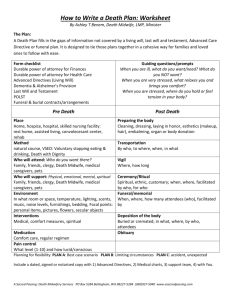
WORKING WITH MOTHERS AND THEIR UNBORN BABIES WHERE THERE ARE CONCERNS FOR THE WELFARE OF THE UNBORN CHILD Working with Mothers and their Unborn Babies where there are Concerns for the Welfare of the Unborn Child T:Paeds SNM/Protocols/concerns for welfare of unborn babies Updated Feb07 Working with Mothers and their Unborn Babies where there are Concerns for the Welfare of the Unborn Child Introduction: Research indicates that young babies are particularly vulnerable to abuse but that work carried out in the antenatal period can help minimise harm if there is early assessment, intervention and support. Working Together (2006) specifically identifies the need of the Unborn Child. Purpose: The purpose of this protocol is to ensure that a clear system is in place to respond to concerns for the welfare of an unborn child and to maintain clear and regular communication. Scope: This joint protocol particularly applies to Social Services staff, police and health. Definitions: Concerns for the welfare of an unborn child include: Concerns that the mother’s current behaviour, e.g. known mental health concern or substance misuse poses a threat to the unborn baby. Concerns that the mother may not be able to care for the baby to an acceptable standard, e.g., significant learning difficulty, previous neglect or other children on the child protection register or have been removed from parental care. Concerns that the behaviour of the father (or any other person) poses a threat to the unborn baby, e.g. domestic abuse or known allegation or conviction for offences against children < 18yrs. Concerns that the behaviour of the father (or any other person) will impact on the ability of the mother to care for the baby to an acceptable standard. The presence of one of these factors does not automatically require referral but they highlight the need to consider the known pre-disposing factors to child abuse. Early Identification & Assessment: All professionals working with families need to be alert to the factors that may indicate a potential risk to the child either before or after birth. It is vital that assessments are started early and that information is shared so that the child and family have the necessary support and best start to family life thereby minimising the need for child protection intervention. Any assessment must include details of the mother’s partner, wider social and family history and environmental factors (as can be found in the Common Assessment Framework) as well as the obstetric history. T:Paeds SNM/Protocols/concerns for welfare of unborn babies Updated Feb07 Routine Antenatal Enquiry The National Service Framework for Children, Young People and Maternity Services (D.O.H, 2004) states that all pregnant women must be offered a supportive environment and the opportunity to disclose Domestic Violence and that local services are trained to respond appropriately. This means that on initial booking, or at another appropriate time (see RCM position paper 19a), the midwife will raise the issue of domestic abuse. Research informs us that 30% of domestic violence starts in pregnancy and that domestic violence is a prime cause of miscarriage or still birth (Why Mothers Die, Department of Health, 2001). A significant number of expectant mothers will need referral to other services See appendix B & C for flowcharts Low Level of Concern: 1. Initial Contact (Approx 8-12 weeks gestation) If in the initial assessment the health professional has some level of concern (considering the risk factors) the family should be informed and that there is a need to liaise and possibly refer to other professionals/agencies. The midwives may refer the pregnant mother to the Social Care (Children’s Services) team following their ‘booking-in’ appointment and Obstetric Booking Assessment form that takes place at approximately 10-12 weeks of pregnancy. If the family already have an identified social worker, then the referral needs to be made to them. The referring midwife must confirm the referral in writing, either by letter or confidential fax, within 48 hours. The Social Care (Children’s Services) team will acknowledge receipt of referral to the midwife and decide on next course of action within one working day. When concerns are raised, at any time to Social Care (Children’s Services) team, by someone other than the midwife, then the Social Services worker involved must bring them to the attention of the named community midwife, if known, or the child protection lead midwife or named nurse for acute or primary health. This enables the midwife to continue to monitor and support the family. If the midwife makes a referral, they must inform the Senior Community Midwife, G.P & Consultant Obstetrician if appropriate. N/B It is the responsibility of the professional making the referral to follow up a referral if there is no response within the given timeframe. T:Paeds SNM/Protocols/concerns for welfare of unborn babies Updated Feb07 Initial assessment If initial assessment is deemed necessary from the Social Care (Children’s Services) team, this must be completed within 7 working days. If child protection concerns are identified, a ‘Strategy Discussion’ will be held with the police, the child protection lead midwife or the named Community Midwife. An agreement will be made and recorded about the next step. Throughout pregnancy the midwife will continue to monitor and support the family. If at any time concerns resurface then the Social Care (Children’s Services) team must be contacted with the new information. Post-natally the midwife will again monitor and offer support until handover to the Health Visitor. The Health Visitor will maintain contact with the family and as for all families will take a lead role in assessment and intervention. See appendix B & D for flowcharts 2. Medium/High Level of Concern: This level of concern relates to when there are concerns that an unborn baby may be “in need” (section 17) or “in need of protection” (section 47) which means that their basic physical and/or psychological needs will not be met and is likely to impair the child’s health or development. See www.swcpp.org.uk for further guidance Where initial contact is made by professionals primarily working with the adult family members, e.g. Police, probation, housing or voluntary agency, and there is this level of concern then the Social Care (Children’s Services) team must be notified regarding the unborn baby. Any professional who has concerns for the welfare of the unborn child must ensure that the midwifery service is aware of the concerns and that any relevant information is passed on. Once the referral has been made the processes are exactly the same as for any child in need/child protection referral N/B Remember that at any stage you can consult with Social Care (Children’s Services) team before making a referral. See appendix B & E for flowcharts T:Paeds SNM/Protocols/concerns for welfare of unborn babies Updated Feb07 Escalation policy If after following all protocols flowcharts the professional still has concerns, then they would need to contact the named professional for child protection who if necessary will implement the relevant escalation policy. Practice Guidance: Although this protocol does not explicitly mention fathers and extended family members it is implicit that they must be included as appropriate in the casework with the mother and unborn child. T:Paeds SNM/Protocols/concerns for welfare of unborn babies Updated Feb07 Appendix B Multi-Agency Pre-Birth Protocol NO CONCERN IDENTIFIED Midwifery Assessment (booking-in) to include Routine Enquiry into Domestic Violence MEDIUM/HIGH LEVEL CONCERN OF 3rd trimester 28- birth 2nd trimester 14-28 weeks 1st trimester 0-14 weeks LOW LEVEL OF CONCERN Ongoing midwifery assessment throughout pregnancy Ongoing midwifery assessment throughout pregnancy Ongoing midwifery assessment throughout pregnancy Inform GP, health visitor & other relevant professionals Discussion with other professionals involved including GP. Early referral from midwife to health visitor. Consult with Social Care for Children’s Services & referral if necessary Ongoing midwifery assessment. Relevant information passed to health visitor or other professionals as required Communication and consultation with all professionals involved with the family. Joint assessment between health visitor & midwife plus appropriate others including escalation if concerns outside of health Antenatal contact by health visitor with all first time mums. To start the health visit or assessment process Antenatal contact by health visitor with all first time mums. To start the health visit or assessment process Plan agreed with parents and midwife Ongoing routine midwifery assessment Review by health visitor if requested Liaison with all professionals involved with family. Intervention as planned Communication and consultation with all professionals involved with the family. Joint midwife and health visitor visit if necessary. Families of med/high level of concern will be discussed at multi-agency maternity liaison meetings. If required multiprofessional/multi-agency meeting to plan assessment and intervention. Initiation of section 47 inquiries Antenatal contact by health visitor with all first time mums. To start the health visit or assessment process Joint assessment including all professionals involved with family. Intervention as planned Strategy discussions CP conference Monitoring of action plans Newborn birth visit by health visitor & handover from midwife to health visitor. Follow up as planned. Services will be determined according to need T:Paeds SNM/Protocols/concerns for welfare of unborn babies Updated Feb07 Appendix C ROUTINE ANTENATAL ENQUIRY No concerns identified at initial assessment 3rd trimester 28- birth Initial assessment by midwifery services indicate no concerns Assessment continues throughout pregnancy 2nd trimester 14-28 weeks 1st trimester 0-14 weeks Midwifery Assessment (booking-in) Health visitor informed regarding pregnancy and outcome of early assessment by midwife Health visitor contact with family as soon as possible after 24 weeks gestation. Health visitor assessment to be based on the common assessment framework. Plan and ongoing contact agreed with family and midwife T:Paeds SNM/Protocols/concerns for welfare of unborn babies Updated Feb07 Appendix D LOW LEVEL OF CONCERN The assessment identified that the family will require core child care/health visiting/midwifery services with limited extra intervention 3rd trimester 28- birth 2nd trimester 14-28 weeks 1st trimester 0-14 weeks Midwifery Assessment (booking-in) Midwifery/health visiting assessment identifies that the family will require core child care/health visiting/midwifery services with limited extra intervention from other agencies, i.e. Social Care (Children’s Services) Midwife to discuss with health visitor, GP and other professionals involved with family, or as appropriate All professionals involved with the family who have an input into the assessment should be kept informed of the current information and stage of assessment. Health visitor to make contact with family as soon as possible. Joint assessment with midwife plus other professionals as appropriate. It may be necessary at this point to consult with Social Care (Children’s Services). Concerns must be monitored and evaluated and additional advice taken if necessary. Assessment should identify concerns and plan intervention to reduce risk Midwife should maintain contact with family and professionals, and take lead role in continuing assessment , monitoring and intervention. Services will be determined according to need T:Paeds SNM/Protocols/concerns for welfare of unborn babies Updated Feb07 Appendix E MEDIUM/HIGH LEVEL OF CONCERN The assessment indicates that this may be a child in need or at risk of significant harm who is unlikely to achieve and maintain a reasonable standard of health and development without high level intervention from a number of different services. There is an indication that there is a likelihood of impairment of health and development. Midwifery Assessment (booking-in) 2nd trimester 14-28 weeks Ongoing midwifery assessment. Inform GP, health visitor & other relevant professionals Communication and consultation with all professionals involved with the family. Joint assessment between health visitor & midwife plus appropriate others including escalation of concerns outside of health During the early antenatal period, the midwife must inform health visitor, GP and other relevant professionals, i.e. Social Care (Children’s Services) about the outcome of her initial assessment and the analysis of risk. An early consultation with the children’s social care may be appropriate to take advice regarding referral/intervention, particularly if other children in the family or concerns regarding mother’s well being All professionals involved with the family who have an input into the assessment should be kept informed of current information and stage of assessment. Health visitor must make contact with family as soon as possible. Ongoing assessments should be reviewed or made jointly between midwife and health visitor and include consideration of further consultation with or referral to children’s social care. If a referral to Social Care (Children’s Services) is necessary, the contact must be made at the earliest opportunity to enable an early planning meeting to look at the common framework assessment. A strategy meeting should be convened and a child protection/planning meeting arranged if necessary 3rd trimester 28- birth N/B If concerns of substance misuse (drug/alcohol), then substance misuse assessment must be completed and specialist midwife informed Liaison with all professionals involved with family. Intervention as planned T:Paeds SNM/Protocols/concerns for welfare of unborn babies Ongoing assessment and intervention as planned. Midwife and health visitor to ensure there is close liaison regarding assessed risk, plan for delivery and perinatal period. If child protection conference is necessary, it should be held at a time that will optimise the planning for assessment and ongoing intervention with the parents/family. This may be before 24 weeks if specific risk to the mother or unborn baby is identified Updated Feb07