SADS - The Oliver King Foundation
advertisement

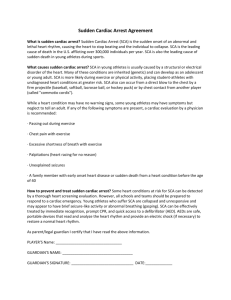
Sudden Arrhythmic Death Syndrome Dr. Simon Modi – Consultant Cardiologist/Electrophysiologist, Dr. Robert Cooper – Cardiology Specialist Registrar, Suzanne Kelly – Heart Rhythm Specialist Nurse Liverpool Heart and Chest Hospital Sudden Arrhythmic Death Syndrome (or SADS) is the term used to describe a group of medical conditions that lead to sudden, unexpected and life threatening instability of the heart’s rhythm. In various forms it is also known as Sudden Cardiac Arrest (SCA), Sudden Cardiac Death (SCD), Sudden Infant Death (SID) or Sudden Unexplained Death (SUD). We will use the term Sudden Cardiac Arrest (SCA) for the purpose of this website. In the majority of cases the unstable heart rhythm (arrhythmia) that develops is a rhythm called Ventricular Fibrillation (VF), where the main pumping chambers of the heart (the ventricles) lose all rhythm and regularity and start beating at heart rates in excess of 250 beat per minute. Ventricular fibrillation is incompatible with life and will cause sudden collapse, seizure like activity and cardiac arrest (total loss of heart function). If diagnosed quickly then cardiac massage (CPR) and a shock from a defibrillator can quickly restore the normal rhythm of the heart and signs of life. Sudden Cardiac Arrest is uncommon in young people. In the general population the chance of SCA is highest in people with known angina, heart attacks or furred arteries but because these conditions are rare in the under 35’s sudden cardiac arrest in the young tends to be caused by other diseases. What is the Difference between a Heart Attack and Sudden Cardiac Arrest? Heart Attacks occur when the blood supply to the heart (coronary arteries) suddenly blocks or narrows. It will commonly cause chest, throat or arm pain, heaviness or tightness. Disruption to the blood supply will lead to damage to the muscle and cells of the heart. This can lead to heart failure (loss of strength of the heart’s pump due to weak heart muscle) and rarely can lead to disturbance of the heart rhythm. This can be in the form of slowing of the heartbeat, quickening of it or cardiac arrest. Most people who have heart attacks do not develop sudden cardiac arrest. In contrast sudden cardiac arrest (SCA) relates purely to a sudden life threatening rhythm disturbance of the heart (usually ventricular fibrillation) but does not need problems with the arteries to be present. In particular, when SCA occurs in younger people, the chances of it being caused by blocked arteries is much lower because blocked arteries are generally a disease of the over 35’s (particularly male smokers with diabetes, high blood pressure, high cholesterol or blocked arteries in the family). In the younger age group, SCA tends to be causes more commonly by underlying diseases of the heart muscle or diseases of the electric circuits in the heart. How Common is SCA in the under 35’s? Due to a number of factors it is difficult to know exact numbers. Several facts are known: 1. SCA occurs in approximately 3 in 100000 12-35 year olds competing regularly in sport 2. Competing regularly in sport increases your chance of cardiac arrest by nearly 3 fold 3. Screening for cardiac conditions with a medical consultation and an ECG (EKG) significantly reduces rates of SCA in the young. 4. Prompt resuscitation with CPR and defibrillation improves outcomes significantly 5. SCA in the young is undoubtedly more difficult for families, friends and communities to adjust to than in older populations. 6. Some estimates suggest that SCA occurs in approximately 10 people under the age of 35 every week in the UK What Causes SCA? Conditions causing SCA can be split into 4 main categories; abnormalities of the heart blood supply, the heart muscle and the heart’s electrics. The 4th category includes ‘other conditions’ that although not specifically heart conditions can have a ‘knock on’ effect on the heart’s function. All conditions have a single common feature, that of the ability to suddenly destabilize the heart’s rhythm and cause SCA. Blood Supply The heart is kept nourished by a series of arteries (coronary arteries) supplying its muscle and electrical circuits. Sudden blockage of these arteries (as in heart attack) can destabilize either heart pumping strength or heart rhythm as previously described. Blocked arteries tends to be a disease of the over 35’s. It is more common in males, smokers and people with a strong family history of blocked arteries (angina, stents or bypass surgery). Conditions such as sugar diabetes, high blood pressure and high cholesterol also cause blocked arteries. Other than blockages, disruption to heart arteries can also occur in the form of spasm (sudden narrowing of arteries reducing blood supply), sudden rupture and congenital abnormalities of the origin of the arteries (can lead to compression of the blood supply). All can cause SCA but are very rare. Other than SCA, coronary artery disease can cause chest pain (chest, shoulder, throat, arm, jaw or upper abdomen) or tightness on exertion. It can sometimes cause excessive belching, shortness of breath or clamminess. Rest will often cause symptomatic relief within 5-10 minutes. Heart Muscle Diseases Diseases of the heart muscle (cardiomyopathies) are the commonest cause of SCA in the young. Two conditions Hypertrophic Cardiomyopathy and Arrhythmogenic Right Ventricular Cardiomyopathy are the commonest causes of sports field related deaths (approx. 95%). Other conditions such as Dilated Cardiomyopathy, Myocarditis and Infiltrative Cardiomyopathies are also known to cause SCA. Many of these conditions will be silent (i.e. no symptoms before SCA) however exertional dizziness, faints, shortness of breath or chest pain can occur. All of these conditions disrupt the muscle structure of the heart thereby disturbing the normal passage of electricity though the heart. Under certain circumstances (e.g. illness, extreme exertion) this can lead to SCA. Electrical Diseases Electrical diseases relate to the way in which the heart is ‘wired’ or the way in which the heart cells manage electricity. Wiring problems that can lead to SCA relate predominantly to a condition called Wolff-Parkinson-White syndrome in which an extra wire exists connecting the top and bottom chambers of the heart (atria and ventricles). Other ‘electrical’ diseases alter the way in which each heart beat electrical signal is generated, conducted and re-generated and under certain circumstances can lead to SCA. These conditions include Long QT syndrome (LQT), Catecholaminergic Polymorphic VT (CPVT), Brugada syndrome (BS), Early Repolarization Syndrome (ERS), Short QT syndrome (SQT) and idiopathic ventricular fibrillation (IVF). Most of these conditions can cause dizziness or faints but will largely go unrecognized until SCA occurs. Certain triggers for fainting (other than exertion) such as large meals, fever, swimming, alarm clocks, sleep and use of antibiotic or antihistamine medication can raise suspicion of the presence of one of these conditions. Other Causes In certain sports, sudden impact to the chest (e.g. ball or physical contact) that happens at a specific time during a normal heart rhythm can cause SCA. This happens even when no underlying heart problems are present (i.e. completely healthy muscle, arteries and electrics). This condition, called Commotio cordis, has been seen most commonly in sports with high speed, small, solid balls (e.g. baseball). It cannot be medically screened for but can be avoided by the use of impact protecting vests. Other conditions that lead to SCA are rare and may have no direct relation to the heart. These can include conditions such as the rupture of major blood vessels (aortic dissection), to epilepsy & bleeding in the brain or imbalance of salts and minerals in the body. All these conditions can alter the way in which oxygen and minerals are delivered to the heart or brain leading to a ‘knock-on’ effect of SCA. Screening Screening, in the form of a medical consultation and an ECG has been in place for Italian athletes since 1982. Italian death rates in 12-35 year olds competing regularly in sport appear to have dropped significantly and now are approximately the same as those of nonathletes of the same age. This has become Italian law. Currently no regulations exist in the UK sporting arena. Graph showing decline in SCA of under 35 year old Italian athletes since the introduction of a national screening programme in 1982. (Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. Journal of the American Medical Association 2006;296:1593–1601.) Medical consultations focus on the presence of abnormal symptoms during exertion (dizziness, excess fatigue, faints, chest pain or palpitations) as the majority of athletes having SCA will have had some prior warning signs, however subtle. The medical consultation should also look for a ‘sinister’ history in the athlete’s family. This could include something as obvious as SADS in the family, to more subtle signs such as unexplained drowning or single vehicle car accidents, uncontrolled seizures despite medication, cot death or recurrent miscarriages. Each of these features has been linked with SADS. ECGs are quick and easy tests to perform. They can be performed in less than 5 minutes by sticking 10 leads across the patient’s chest and limbs and recording the heart’s electrical activity. In athletic people a normal ECG is highly likely to represent a normal heart. An abnormal ECG however may represent either a normal variant or underlying heart or electrical disease. Screening of all athletes is controversial mainly due to the rarity of SCA in the young and the potential difficulty of distinguishing ECG changes in the ‘normal athlete’ from those in an ‘abnormal’ heart. Nevertheless, continued and advancing knowledge in this area seeks to change these opinions slowly.