Medical Nutrition Therapy for Pulmonary Disease
advertisement

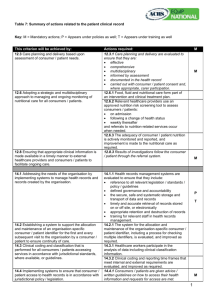
Medical Nutrition Therapy for Pulmonary Disease 報告者:臺北醫學大學•市立萬芳醫院 報告日期:民國 90 年 11 月 15 日 徐家瑜 營養師 @Relationships between nutrition and the pulmonary system @Bronchopulmonary dysplasia # Bronchopulmonary dysplasia(BPD) is a chronic lung condition of infancy that occurs most frequently in premature infant following respiratory distress syndrome(RDS) in the neonatal period. #nutritional status and assessment---1.Because lung size is stature-dependent, linear growth is important for the growth of healthy lung tissue and for the resolution of the condition 2.Resons for growth failure among infants with BPD include increased energy needs combined with iadequate dietary intake, gastroesophageal reflux, emotional deprivation, and chronic hypoxia #nutritional requirements and care---I. energy---II. macronutrients---III. vitamins and minerals---IV. diet modification----- @Cystic fibrosis #figure 37-2 #Pathophysiology and diagnostic criteria----Diagnostic criteria: 1.neonatal screening for cystic fibrosis 2.sweat test: Elevated levels of sodium and chloride(>60mnEq/L) in collected sweat samples are indicative of CF 3.positive result on the sweat test and the presence of chronic lung disease, failure to thrive and malabsorption, or a family history of CF Pathophysiology: 1.Approximately 85% CF patients have pancreatic insufficiency. 2.Decreased bicarbonate secretion can further reduce digestive enzyme activity. 3.Decreased bile acid reabsorption contributes further to fat malabsorption. 4.CF-related diabetes mellitus #Nutritional status and assessment---1.factors interfering with adequate intake and retention of nutrients : 2.table 37-4 #Nutritional requirements and care---I. nutritional requirements and intervention need to be integrated with other therapies II. the goals: 1. control maldigestion and malabsorption 2. to promote optimal growth or maintain weight for height and pulmonary function 3. prevent nutritional deficiences 4. table37-5 III. pancreatic enzyme replacement therapy IV. For children or infant unable to swallow capsules, the capsules can be opened and the microspheres mixed with PH<6 food. V. energy---age, gender, basal metabolic rate, physical activity, respiratory infection, severity of lung disease, and severity malabsorption @Chronic obstructive pulmonary disease(COPD) # COPD is characterized by slowly progressive obstruction of airways. Subdivide two categories: I. emphysem II. chronic bronchitis # Nutritional status and assessment---(1) Nutritional depletion is evidenced clinically by low body weight for height, reduced triceps fatfold measurements. (2)Depletion appears related to pulmonary complications. (3)assessment---1. components of nutritional assessment in COPD are listed in Table 37-9 2. determine body composition, anthropometric measurements, biochemical indicators of nutritional status 3. the medication profile should be assessed for food and nutrient interactions. 4. other pertinent assessments focus on blood oxygen saturation, anorexia… #Nutritional requirements and care-----The primary goals: to facilitate nutritional well-being, maintain an appropriate lean body mass: adipose tissue ratio, correct fluid imbalance, and manage drug-nutrient interactions I. energy—requirements are elevated in COPD and they vary for each individual II.macronutrients— 1. sufficient protein: 1.0-1.5 gram/kg dry body weight 2. A balanced ratio of protein(15 to 20% of calories) with fat (30 to 45% of calories) and carbohydrate(40 to 55% of calories) 3. underlying conditions III.vitamins and minerals---1. vitamin and mineral requirements depend on the underlying lung Pathology, other concurrent diseases, medical treatments and weight status. 2. magnesium and calcium 3. magnesium and phosphorus : because of their cofactor roles in ATP 4.patients with cor pulmonale and fluid retention require sodium and fluid restriction. #Diet modification-----resting before meals, eating small portions of nutrient-dense foods, planning expectorant medication usage apart from mealtimes, enteral nutritional supplementation @Asthma #Known as hyperactive airways, is classified as a reversible obstructive respiratory disorder #May be related to allergen exposure, including foods #In young children, this can result in permanent oral structure malform-ation #Nutritional requirement and care---I. magnesium II. chronic use of prescribed corticosteroids III. medications relate to nutritionally relevant, side effects @Aspiration #At increased risk are infants, toddlers, elderly people, and individuals with oral, upper gastrointestinal neurologic, or muscular abnormalities #Proper body positioning when eating is essential for everyone @Lung cancer @Pneumonia and Tuberculosis #Among the pulmonary infections with nutritional implications are pneumonia and TB #Pneumonia usually occurs as a nosocomial infection or as a consequence of food, fluid, or secretion aspiration. #Isoniazid(INH) depletes pyridoxine(vitamin B6) and interferes with vitamin D metabolism #Isoniazid(INH) can decrease absorption of calcium and phosphorus @Respiratory failure #Central factors in failure to wean from oxygen support or mechanical ventilation are respiratory muscle weakness and retention of carbon dioxide # Nutritional status and assessment------I. depend on the underlying disease process , prior nutritional status, and age. II. Hypercatabolism or hypermetabolism may be present. III. Body composition fluctuations are the halmark nutritional assessment indicators #Nutritional requirements and care -----I. the goals: 1.meet basic nutritional requirements 2.preserve lean body mass, restore respiratory muscle and strength 3.maintain fluid balance 4.improve resistance to infection 5.facilitate weaning from oxygen support and mechanical ventilation II. energy: 1.to prevent the use of the body’s own reserves of protein and fat 2.To estimate initial caloric requirements, the Harris-Benedict equation, modified for stress as well as the underlying disease, can be used. 3.indirect calorimetry is most useful, except for the patients who are mechanically ventilated 4.overfeeding should be avoided III. macronutrients----1.nitrogen balance 2.The basic requirements for carbohydrate and fat are infl-uced by the underlying organ system decompensation, the patient’s respiratory status, and vntilation methods used. 3.Some clinicians start with 1.2-1.4xREE. Protein is calculated as 1.5-2.0grams/kg dry body weight. Nonprotein cal-ories are evenly divided between fat and carbohydrate. IV. Vitamins and minerals----1.RDA 2.The intake of vitamins and mineral s necessary for anabolism, wound healing, and immunity, as well as antioxidant functions, may need to increased. 3.monitor minerals the function as electrolytes 4.monitor mineral balance 5.monitor K,Ca,Mg V. Diet modification-----Oral: Tube feeding: