Managing Hyperglycaemia in Acute Coronary Syndrome
advertisement

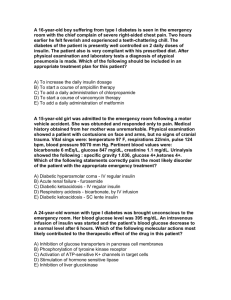
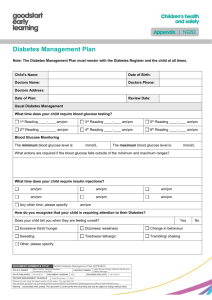
Managing Hyperglycaemia in Acute Coronary Syndrome If there are any questions please contact: Diabetes Liaison Nurses: EXT 4198. BLP: 7721/7881 Mon - Fri, 9 - 5 PM Diabetes Registrars: Bleep 7021/7018 Dr Marc Atkin EXT 4991 (secretary) Dr Kate Allen EXT 4477(secretary) Dr Tony Robinson. EXT 4530 (secretary) Dr Alex Ward. EXT 6232 (secretary) Based on NICE guidance 130 All patients admitted to hospital with an acute coronary syndrome should have their glucose checked on admission. In all patients with hyperglycaemia (blood glucose > 11mmol/l) consider whether they may have diabetic ketoacidosis (DKA) or a hyperosmolar hyperglycaemic state (HHS). If either of these diagnoses is confirmed management should be according to the appropriate protocol. Patients with Pre-existing Diabetes Please send blood for HBA1c if no result in the last 3 months Admission glucose < 11mmol/l Continue usual diabetes treatment if possible. Stop metformin and pioglitazone in patients with heart failure* Stop metformin in any patient with an eGFR < 30ml/min. Monitor blood glucose at least 4 times per day. Review and adjust therapy to maintain glucose within target range (4-11mmol/l) – if patients have had to stop pioglitazone and/or metformin it is more likely other treatments will need to be adjusted. Inform diabetes team of admission at the start of the next working day. Admission Glucose > 11mmol/l Exclude diagnosis of DKA/HHS – if confirmed manage according to protocol If the patient is unwell (heamodynamically unstable, heart failure, renal failure) Consider IV sliding scale insulin to maintain glycaemic control (target 4-11mmol/l without hypoglycaemia) using the adult intravenous insulin prescription chart. If on a sliding scale insulin infusion, once glucose under 12mmol/l run IV insulin with IV dextrose. Usually run with 5% dextrose 2 litres over 24 hours with potassium added in line with guidance if potassium less than 5.5mmol/l. Consider 1 litre of 10% dextrose to run over 24 hours with IV insulin in place of 5% dextrose where fluid overload is a concern If the patient is on long acting insulin (glargine or detemir) continue this whilst on the sliding scale. If the patient on an insulin pump and able to adjust themselves, they should continue to use, but if too unwell convert to a sliding scale. Check urea and electrolytes at least once in every 24 hours whilst on sliding scale insulin infusion. Aim to keep the patient on a sliding scale insulin infusion for as short a time as possible. Review the use of the sliding scale at least once every 24 hours. When stopping the sliding scale follow the guidelines for the removal of intravenous insulin infusion removal. On stopping the sliding scale patients should usually be returned to previous diabetes treatment. Stop metformin and pioglitazone in patients with heart failure Stop metformin in any patient with an eGFR < 30ml/min and/or creatinine > 150. Monitor blood glucose at least 4 times per day after coming off a sliding scale. Review and adjust therapy to maintain glucose within target range (4-11mmol/l) – if patients have had to stop pioglitazone and/or metformin it is more likely other treatments will need to be adjusted. Inform diabetes team of admission at the start of the next working day. If Patient is Not Unwell Do not routinely start an IV sliding scale insulin infusion Continue usual diabetes treatment if possible. Stop metformin and pioglitazone in patients with heart failure Stop metformin in any patient with an eGFR < 30ml/min and/or creatinine > 150. Monitor blood glucose at least 4 times per day. Review and adjust therapy to maintain glucose within target range (4-11mmol/l) – if patients have had to stop pioglitazone and/or metformin it is more likely other treatments will need to be adjusted. Inform diabetes team of admission at the start of the next working day. Patients without Pre-existing Diabetes Admission laboratory glucose >7 < 11mmol/l No need to routinely monitor blood glucose levels. Arrange HbA1c. Inform GP of result on discharge summary If HbA1c >48mmol/mol patient may have undiagnosed diabetes – in an asymptomatic patient the abnormal result will need to be confirmed on a separate day usually by the GP after the patient has been discharged – diagnosis of diabetes should be made in line with WHO guidance. If HbA1c > 48mmol/mol on admission blood test inform diabetes team. Admission glucose > 11mmol/l Arrange HbA1c Exclude diagnosis of DKA/HHS – if confirmed manage according to protocol If the patient is unwell (heamodynamically unstable, heart failure, renal failure) Consider IV sliding scale insulin to maintain glycaemic control (target 4-11mmol/l without hypoglycaemia) using the adult intravenous insulin prescription chart. If on a sliding scale insulin infusion, once glucose under 12mmol/l run IV insulin with IV dextrose. Usually run with 5% dextrose 2 litres over 24 hours with potassium added in line with guidance if potassium less than 5.5mmol/l. Consider 1 litre of 10% dextrose to run over 24 hours with IV insulin in place of 5% dextrose where fluid overload is a concern. Review the use of the sliding scale at least once every 24 hours. Check urea and electrolytes at least once in every 24 hours whilst on sliding scale insulin infusion. Aim to keep the patient on a sliding scale insulin infusion for as short a time as possible. Consider whether the patient requires ongoing treatment for possible diabetes before stopping the IV sliding scale insulin infusion. If unsure consult with diabetes team. Do not start metformin or pioglitazone in patients with heart failure. Do not start metformin in patients with renal failure (eGFR < 30 ml/min and/or creatinine > 150) When sliding scale has been stopped monitor blood glucose at least 4 times per day. Review and adjust/start diabetes therapy to maintain glucose within target range (4-11mmol/l) Inform diabetes team of admission at the start of the next working day. If Patient is Not Unwell Do not routinely start an IV sliding scale insulin infusion Monitor blood glucose at least 4 times per day. Consider whether the patient requires treatment for hyperglycaemia. If uncertain consult with diabetes team. Do not start metformin or pioglitazone in patients with heart failure. Do not start metformin in patients with renal failure (eGFR < 30 ml/min and/or creatinine > 150) Review and start/adjust therapy to maintain glucose within target range (4-11mmol/l) Inform diabetes team of admission at the start of the next working day. In patients not previously known to have diabetes it is important to confirm (or not) the diagnosis even when glucose is raised on admission. If the HbA1c is > 48mmol/mol on admission this should be confirmed on another day usually after discharge unless the patient is symptomatic when one abnormal HbA1c is sufficient. Any patient with HbA1c > 48mmol/mol not previously known to have diabetes should be notified to the diabetes team. If the HbA1c on admission is < 48mmol/mol the patient may have stress hyperglycaemia only. This test should be communicated to the GP and recommendation made that annual screening for diabetes should be undertaken using fasting glucose or HbA1c. For Patients Having a Coronary Angiogram with/without Intervention Who Are Treated With Metformin There is no need to stop metformin in patients with serum creatinine within the normal range and/or eGFR > 60ml/min (Standards of Intravascular Contrast Agent Administration to Adult Patients Second Addition) In patients with eGFR 30-60ml/min metformin should be stopped before angiography. Patients should monitor blood sugars at least 4 times per day pre-meal and pre bed after metformin has been stopped. If glucose rises outside the desired range (> 11mmol/l) diabetes treatment should be reviewed to assess whether current therapy requires uptitration or additional therapy needs to be started. The patient should be given the contact details of the diabetes nursing team (see above) and be advised to contact them or their GP if the glucose values increase outside the desired range. Urea and electrolytes must be checked at 48 hours post angiography – this will need to be undertaken by the GP if the patient has gone home and this must be communicated clearly to the GP on the discharge summary Metformin should only be restarted if the eGFR >30mmol/l and/or the creatinine is not more than 30% worse than baseline on the 48 hour post angiogram blood test If metformin not restarted at 48 hours the urea and electrolytes should be rechecked at 7-10 days post angiography to assess whether metformin can be restarted. If at any point the GP is worried about the patient’s renal function this should be discussed in the first instance with the cardiology team who undertook the angiography. Check laboratory glucose on all patients admitted with acute coronary syndrome Known diabetes? yes no Admission glucose greater than 11mmol/l? Admission glucose greater than 11mmol/l? no yes Monitor glucose QDS for 48 hours and adjust therapy as required (Inform diabetes team at the beginning of the next working day). no yes* No need to monitor glucose. Do HbA1c if >7mmol/l and inform gp of result on discharge. If 48mmol/mol likely new diabetes – inform diabetes team. Has the patient got DKA or HHS? (see separate guidance) yes no Do HbA1C Is the patient unwell? (haemodynamically unstable, heart or renal failure) Manage according to DKA/HHS protocol yes Consider sliding scale insulin infusion using adult intravenous insulin prescription chart **. (Inform diabetes team at the beginning of the next working day). no Monitor blood glucose at least 4 times per day. Consider adjusting usual diabetes medication to maintain control (4-11mmol). (Inform diabetes team at the beginning of the next working day of admission) Review use of insulin infusion at least every 24 hours. *In patients not previously known to have diabetes it is important to confirm (or not) the diagnosis. If the HbA1c is > 48mmol/mol on admission this should be confirmed on another day (usually after discharge) unless the patient is symptomatic when one abnormal HbA1c is sufficient. If the HbA1c is < 48mmol/mol the patient may have stress hyperglycaemia only. This test should be communicated to the GP and recommendation made that annual screening for diabetes should be undertaken using fasting glucose or HbA1c.. **Once glucose under 12mmol/l run IV insulin with IV dextrose. Usually run with 5% glucose 2 litres over 24 hours with potassium added in line with guidance if potassium less than 5.5mmol/l. Consider 1 litre 10% dextrose to run over 24 hours with IV insulin in place of 5% dextrose where fluid overload is a concern.